To compare percutaneous nephrolithotomy and flexible ureterorenoscopy for treating kidney stones between 2 and 3cm.
Material and methodsA prospective, comparative, nonrandomised study was conducted with 108 patients with kidney stones between 2 and 3cm. Fifty-four patients underwent percutaneous nephrolithotomy and 54 underwent flexible ureteroscopy. We compared the following variables: lithiasis-free rate (%), surgical time, the need for an auxiliary process, postoperative complications, hospital stay, readmission rates and recovery time.
ResultsThere were no differences in the lithiasis-free rate between the 2 surgical techniques (76% for ureteroscopy vs. 87% for nephrolithotomy; p=0.1) or in the complications (29% for nephrolithotomy vs. 27% for ureteroscopy; p=0.4). A larger number of auxiliary process were needed for the ureteroscopy group (20%) than for the nephrolithotomy group (7%) (p=0.04).
The surgical time was longer for the nephrolithotomy group (121±52min) than for the ureteroscopy group (93±42min) (p=0.004).
The ureteroscopy group had shorter hospital stays (2.1±1.6 vs. 3.9±1.9 days; p=0.002), shorter convalescence (8.1±4.9 vs. 13.3±4.2 days; p=0.005) and higher readmission rates (7.4% vs. 0%, p=0.05) than the nephrolithotomy group.
ConclusionsNephrolithotomy and ureteroscopy have similar efficacy for treating kidney stones measuring 2–3cm, with no differences in complications.
Ureteroscopy results in shorter hospital stays, quicker recoveries but more readmissions and a greater need for auxiliary procedures.
Comparar la nefrolitotomía percutánea y la ureterorrenoscopia flexible para el tratamiento de la litiasis renal entre 2 y 3cm.
Material y métodosEstudio prospectivo, comparativo, no aleatorizado en 108 pacientes con litiasis renal entre 2 y 3cm; a 54 se les realizó nefrolitotomía percutánea y a 54 una ureteroscopia flexible. Las variables comparadas son: tasa libre de litiasis (%), tiempo quirúrgico, requerimiento de proceso auxiliar, complicaciones postoperatorias, estancia hospitalaria, tasas de reingreso y tiempo de recuperación.
ResultadosNo existieron diferencias en la tasa libre de litiasis entre ambas técnicas quirúrgicas (76% ureteroscopia, 87% nefrolitotomía) (p=0,1), ni en las complicaciones (nefrolitotomía: 29%; ureteroscopia: 27%; p=0,4). Se ha requerido mayor número de procesos auxiliares en el grupo de ureteroscopia (20%) frente al de nefrolitotomía (7%) (p=0,04).
El tiempo quirúrgico fue más largo en el grupo de nefrolitotomía (121±52min) que en el grupo de ureteroscopia (93±42min) (p=0,004).
El grupo de ureteroscopia tuvo menor estancia hospitalaria (2,1±1,6 vs. 3,9±1,9 días, p=0,002), menor convalecencia (8,1±4,9 vs. 13,3±4,2 días, p=0,005) y mayores tasas de reingreso (7,4% vs. 0%, p=0,05) que el grupo de nefrolitotomía.
ConclusionesLa nefrolitotomía y la ureteroscopia tienen una eficacia similar para el tratamiento de la litiasis renal entre 2–3cm, sin diferencias en las complicaciones.
La ureteroscopia tiene menor estancia hospitalaria, una recuperación más rápida pero mayor reingreso y necesidad de procedimiento auxiliar.
European guidelines updated as of 2015 recommend percutaneous surgery (PCNL) and flexible ureterorenoscopy (F-URS) as treatments of choice for calculi of 1–2cm in the lower calyx, with unfavorable factors for extracorporeal lithotripsy. PCNL is considered the technique of choice for the treatment of renal lithiasis>2cm.1,2 Although PCNL is highly effective, it continues to have a non-negligible morbidity.3,4. The technological advances applied to flexible endoscopy allow F-URS to be a valid alternative for the treatment of larger renal lithiasis,5–11 with few comparative studies between the two techniques.12,13
The main objective of this study was to compare the efficacy (stone free rate %) of both surgical techniques. The secondary objectives were to analyze and compare complications, surgical time, ancillary process requirements, readmission rates, hospital stay, and recovery time.
Material and methodsBetween January 2013 and December 2015 we performed an observational, prospective, comparative, non-randomized study of 108 patients with symptomatic renal lithiasis between 2 and 3cm.
Inclusion criteria were any patient with single or multiple symptomatic renal lithiasis (pain, infection or hematuria) between 2 and 3cm. Exclusion criteria were single kidney patients, with known kidney failure and previously diagnosed anatomical alterations (pyelo-ureteral stenosis, calyceal diverticula). Patients were explained the possibility of both treatments, with the known advantages and disadvantages of both, and according to their opinion, and under medical criteria, they were performed one technique or the other. All patients sign an informed medical consent. Assuming a stone free rate of 80% with RIRS, and about 100% with PCNL, the sample size was calculated at least at 35 patients per group, assuming a type 1 error of 5%. Finally, 54 patients underwent PCNL and 54 patients underwent F-URS.
All patients underwent a clinical evaluation that included a complete medical history with anamnesis and physical examination, routine laboratory tests (baseline serum parameters including complete blood count, coagulation, biochemistry) and an anesthetic risk assessment according to the American Anesthesiology Association (ASA). A sediment and urine culture was collected one week before the surgery. Patients with positive culture were treated with antibiotic between 5 and 7 days before the surgery, the rest were treated with 1.5g ev of cefuroxime in anesthetic induction. All patients were evaluated preoperatively with abdominal CT scan.
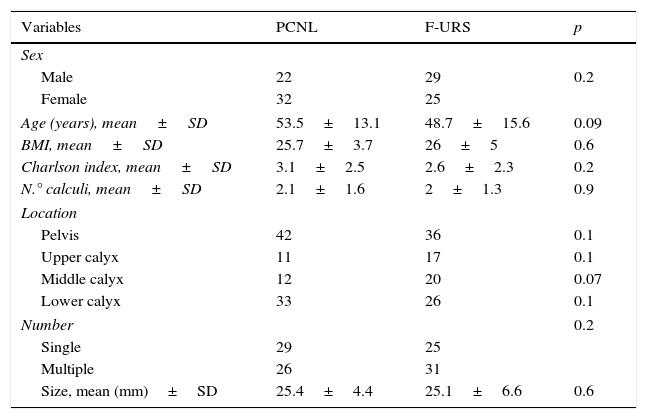
The epidemiological and clinical characteristics of the patients (sex, age, body mass index, Charlson morbidity index), as well as the data of the lithiasis (number, location, uni/multiplicity, size) were collected and compared (Table 1). The size of the stone was measured as the largest diameter. In cases of multiple lithiasis, it was defined as the sum of the largest diameters of each lithiasis.
Comparative summary table of patient clinical data and renal lithiasis data.
| Variables | PCNL | F-URS | p |
|---|---|---|---|
| Sex | |||
| Male | 22 | 29 | 0.2 |
| Female | 32 | 25 | |
| Age (years), mean±SD | 53.5±13.1 | 48.7±15.6 | 0.09 |
| BMI, mean±SD | 25.7±3.7 | 26±5 | 0.6 |
| Charlson index, mean±SD | 3.1±2.5 | 2.6±2.3 | 0.2 |
| N.° calculi, mean±SD | 2.1±1.6 | 2±1.3 | 0.9 |
| Location | |||
| Pelvis | 42 | 36 | 0.1 |
| Upper calyx | 11 | 17 | 0.1 |
| Middle calyx | 12 | 20 | 0.07 |
| Lower calyx | 33 | 26 | 0.1 |
| Number | 0.2 | ||
| Single | 29 | 25 | |
| Multiple | 26 | 31 | |
| Size, mean (mm)±SD | 25.4±4.4 | 25.1±6.6 | 0.6 |
Patient in Valdivia position modified according to Galdakao.14,15 Under general anesthesia, placement of a 6Fch ureteral catheter up to the renal pelvis was performed by means of urethro-cystoscopy. Subsequently, opacification of the urinary tract and puncture of renal cavities with a remote-controlled 18G needle were performed. In most cases, a high-pressure balloon path dilation was performed up to 24Fch, or with progressive metallic dilators telescoped according to Alken's technique, leaving 24Fch Amplatz sheath. Storz nephroscope was used without the outer sheath, and lithotripsy was performed with ultrasonic energy (Olympus). At the end of the procedure, a 20Fch nephrostomy tube was left on the way to the renal cavities. The surgical time was calculated from the beginning of the urethrocystoscopy until the placement of the nephrostomy.
Flexible ureterorenoscopy techniqueIt was performed with the patient of lithotomy and under general anesthesia. A semi-rigid transurethral ureteroscope passage was performed up to the bladder access, a safety guidewire was placed up to the renal cavities, a semi-rigid ureteroscopy was performed up to the kidney to check the ureter status and to perform a controlled dilation of it. Subsequently, ureteral access sheath 11/13 to 13/15Fch (Navigator-Boston) was placed to the pyeloureteral junction, and a flexible digital ureteroscope (Olympus or Storz) was passed. Lithotripsy was performed with 270μm fiber of Dornier Holmium laser, for multifragmentation-vaporization with an energy in the range of 0.4–0.8J at a frequency of 800–1200Hz. At the end of the procedure, all the calyceal groups were inspected to confirm adequate fragmentation. In all cases we left a 6Fch JJ renovesical catheter, which was removed on an outpatient basis after 7–10 days if there are no complications. The surgical time was calculated from the beginning of the ureteroscopy until the placement of the JJ renovesical catheter.
The efficacy of the surgical technique (% stone free rate) was evaluated at the third postoperative month with the performance of a simple abdominal Rx and a kidney and bladder ultrasound. It was considered clean of lithiasis when there is no evidence of lithiasic remains or they are <4mm.16 Those patients with symptomatic residual lithiasis undergo a second procedure that was counted and evaluated as an auxiliary process requirement.
Complications were recorded according to the modified Clavien-Dindo classification.17
Convalescence time was considered the time that elapses from the time when the patient is operated until he resumes his usual physical activity, allowing him to carry out his usual professional activity.
To analyze the results, we used the statistical program SPSS 13.0. When the distribution of numerical variables was normal, Student's ‘t’-test for mean comparison was used. The Chi square test was used to analyze the proportions of categorical variables. Statistically significant difference was considered when p was less than or equal to 0.05.
ResultsThe epidemiological and clinical characteristics of the patients (sex, age, body mass index, Charlson's morbidity index), as well as the characteristics of the lithiasis (number, location, size, and uni/multiplicity), were similar in both groups, without significant differences (Table 1).
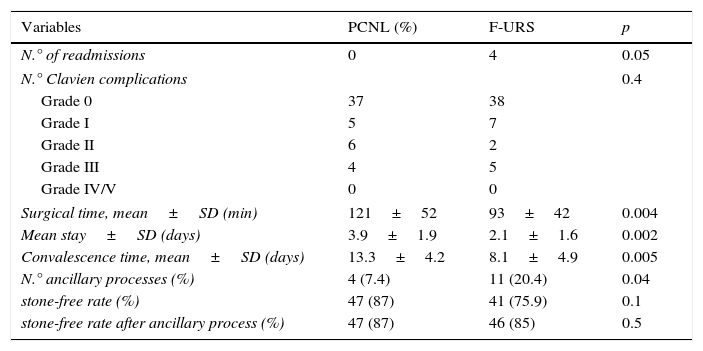
The stone-free rate was lower in the RIRS group (76%) than in the PCNL group (87%), with no significant differences (p=0.1). At 3 months, and taking into account the need for a second procedure, the stone-free rates were similar in the RIRS (85%) and PCNL (87%) group (p=0.5). A significantly higher percentage of second procedures was required due to symptomatic remains in the RIRS group (20%) versus PCNL (7%) (p=0.04). The RIRS group needed in 4 patients rigid ureteroscopy, in 5 patients extracorporeal shock wave lithotripsy, in one patient urinary diversion with a new JJ catheter, and in another one with nephrostomy. A rigid ureteroscopy, an extracorporeal lithotripsy, and 2 ureteral JJ catheterizations were required in the PCNL group (Table 2).
Comparative summary table of the results obtained.
| Variables | PCNL (%) | F-URS | p |
|---|---|---|---|
| N.° of readmissions | 0 | 4 | 0.05 |
| N.° Clavien complications | 0.4 | ||
| Grade 0 | 37 | 38 | |
| Grade I | 5 | 7 | |
| Grade II | 6 | 2 | |
| Grade III | 4 | 5 | |
| Grade IV/V | 0 | 0 | |
| Surgical time, mean±SD (min) | 121±52 | 93±42 | 0.004 |
| Mean stay±SD (days) | 3.9±1.9 | 2.1±1.6 | 0.002 |
| Convalescence time, mean±SD (days) | 13.3±4.2 | 8.1±4.9 | 0.005 |
| N.° ancillary processes (%) | 4 (7.4) | 11 (20.4) | 0.04 |
| stone-free rate (%) | 47 (87) | 41 (75.9) | 0.1 |
| stone-free rate after ancillary process (%) | 47 (87) | 46 (85) | 0.5 |
The complications of both surgical techniques were similar according to the Clavien-Dindo classification, with no significant differences between the two groups (p=0.4). There were 29% of complications in the PCNL group, all being lower than Clavien 3 (10% Clavien 1, 11% Clavien 2 and 8% Clavien 3). We observed 27% of complications in the F-URS group, all being inferior to Clavien 3 (13% Clavien 1, 4% Clavien 2, and 10% Clavien 3). 15 complications were observed in the PCNL group: 5 grade 1 complications (4 urinary infections, 1 hematuria), 6 grade 2 complications (4 transfusion, 2 prolonged fevers), 4 grade 3 complications (1 renovesical JJ catheterization due to urinary fistula, 2 renovesical JJ catheterizations due to renal colic, 1 embolization due to persistent hematuria), and no complication greater than 3. We observed 14 complications in the RIRS group: 7 grade 1 complications (6 hematurias and 1 urinary infection), 2 grade 2 complications (prolonged fever), 5 grade 3 complications (4 renovesical JJ catheterizations per renal colic and 1 percutaneous renal abscess puncture) and no major grade 3 complications.
Surgical time (mean±SD) was significantly longer in the PCNL group (121±52min) than in the RIRS group (93±42min) (p=0.004).
The RIRS group had a shorter hospital stay (mean±SD) (2.1±1.6 vs. 3.9±1.9 days, p=0.002) and a shorter period of convalescence (mean±SD) (8.1±4.9 vs. 13.3±2.4 days, p=0.005) than PCNL.
There were significantly higher re-admission rates in the RIRS group (7.4%) than in the PCNL group (0%) (p=0.05).
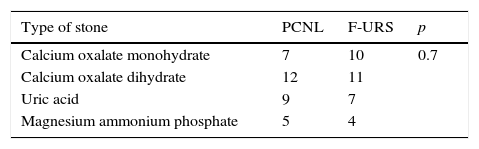
Although we have not been able to obtain the analysis of the calculi in all cases, we can observe how there are no differences in the type of calculi analyzed in relation to the technique performed (Table 3).
DiscussionAccording to the European guidelines, the technique of choice for renal lithiasis greater than 2cm is PCNL, without specifying which one (standard, mini PCNL, ultramini PCNL, or micro PCNL), and that there is an increasing tendency to perform less invasive techniques, using smaller calibres, thus reducing morbidity.18 However, studies comparing mini-PCNL vs RIRS indicate similar results (lithiasis-free rate) with the same complication rate (postoperative stay, analgesic requirement). The latest publications19–22 indicate better results with mini PCNL in average size (1.5–2cm) lower than ours. When sizes are >2cm, the results are matched with longer hospital stay for mini PCNL.23,24 Therefore, in our study, facing more complex cases (2.5cm mean size, 50% multiplicity), we compared the results to standard PCNL (24Fch), and because the applicable ultrasonic lithotripsy in standard PCNL enables aspiration of fragments. But undoubtedly, mini PCNL alone or combined with RIRS is an attractive alternative, since it makes it possible to add the advantages of both techniques with less morbidity. It remains to be determined which group of patients will be the best candidates, probably those in whom RIRS alone is less effective (hard lithiasis, multiple between 2 and 2.5cm and of more difficult retrograde access).
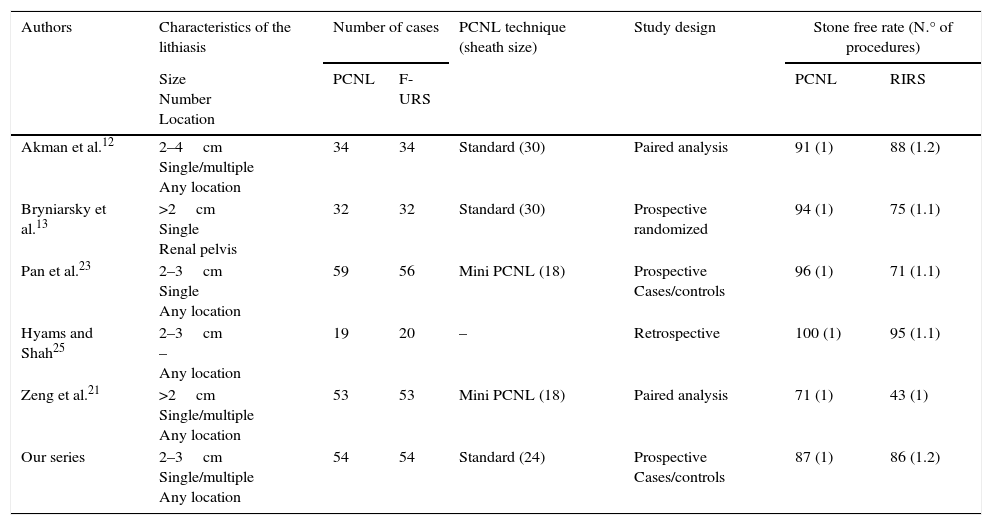
Most of the authors who have compared the efficacy of both treatments in renal lithiasis ≥2cm agree that in a single procedure the efficacy is higher with PCNL. However, these differences disappear if we take into account the repetition of the procedure10,12,21,23,25 (Table 4). We have obtained these same results. At 3 months, we verified that the efficacy of both techniques is similar, although with F-URS we need more procedures due to greater symptomatic residual lithiasis, which is also reflected in a higher re-admission rate. In a not very far away future, improvements in lasers (improvement in vaporization, aspiration systems) and the combination of less invasive anterograde-retrograde techniques (smaller caliber of endoscopes) probably allow us to reduce this residual rate.
Summary of the publications referenced in the bibliography.
| Authors | Characteristics of the lithiasis | Number of cases | PCNL technique (sheath size) | Study design | Stone free rate (N.° of procedures) | ||
|---|---|---|---|---|---|---|---|
| Size Number Location | PCNL | F-URS | PCNL | RIRS | |||
| Akman et al.12 | 2–4cm Single/multiple Any location | 34 | 34 | Standard (30) | Paired analysis | 91 (1) | 88 (1.2) |
| Bryniarsky et al.13 | >2cm Single Renal pelvis | 32 | 32 | Standard (30) | Prospective randomized | 94 (1) | 75 (1.1) |
| Pan et al.23 | 2–3cm Single Any location | 59 | 56 | Mini PCNL (18) | Prospective Cases/controls | 96 (1) | 71 (1.1) |
| Hyams and Shah25 | 2–3cm – Any location | 19 | 20 | – | Retrospective | 100 (1) | 95 (1.1) |
| Zeng et al.21 | >2cm Single/multiple Any location | 53 | 53 | Mini PCNL (18) | Paired analysis | 71 (1) | 43 (1) |
| Our series | 2–3cm Single/multiple Any location | 54 | 54 | Standard (24) | Prospective Cases/controls | 87 (1) | 86 (1.2) |
The 2 studies most similar to ours obtain similar efficacy figures for both techniques, 90% and 94% for PCNL, and 75% for F-URS. Unlike our series, in which 50% of patients had multiple lithiasis, Akman et al. only treated 25% of patients with multiple lithiasis, and in the series by Bryniarski et al. they were unique and pyelic lithiases. All of that makes the groups not entirely comparable.12,13
Evaluating surgical time comparatively, we observed longer surgical time in the PCNL group, as did Bryniarsky et al.13 However, Akman et al. found longer surgical time in the F-URS group on PCNL. These studies do not clearly describe how they count operative time. Many factors can influence the time used as the position of the patient, the source and power of energy used in lithotripsy, the technique used (vaporization or fragmentation-extraction). All these factors make comparative analyses difficult.
One of the theoretical advantages of F-URS on PCNL is the need for shorter hospital stay, lower analgesic requirements and, therefore, a faster recovery period. The majority of authors agree to point out that the hospital stay is shorter with F-URS,11,12 an aspect that we have also seen clearly in our study. Other authors have described lower analgesic requirements as an advantage of F-URS over PCNL.13 We have not found in the literature any study that mentions, as a consequence of all the above, that these advantages translate into a shorter time of convalescence or recovery. In our series we can confirm a significantly lower convalescence time with F-URS. This aspect is interesting if we take into account that the majority of the lithiasic population is active in terms of work, so we believe that it should be explained to the patients when deciding the treatment.
Few studies have compared the complications of both surgical techniques using the Clavien Dindo classification and have found no differences.27 Nor do we find differences using Clavien Dindo classification.17 29% and 27% of the patients had some complications in the PCNL and F-URS groups respectively, the majority of them being low grade. In a more voluminous series than ours, on lithiases larger than 2cm treated with F-URS, Giusti et al. obtain 25% of complications.26 Similar figures of complications can be observed with PCNL. Thus, Seitz et al. report 26%, the majority being low grade.27 These data suggest that overall there are no differences in the rates of complications or in the severity of them.
The limitation of this study, despite being observational and prospective, is the lack of randomization of the patients, although we did not observe differences in any of the variables analyzed in both groups (Tables 1 and 3). Another limitation of the study is the evaluation of results with simple Rx and ultrasound. Undoubtedly, the performance of a CT, if possible of low radiation, would have been a more complete evaluation. Another limitation of the study is to have considered fragments <4mm as free from lithiasis. We can intuit that the evolution of the fragments of laserthripsy will be the same as after extracorporeal lithotripsy, 20% of the residual fragments <5mm will have symptoms in a period of 5 years.28 However, most authors still consider this size with high chances of spontaneous expulsion, and therefore considered free of lithiasis.16,29
As a general conclusion, we can affirm that in the absence of comparative prospective randomized studies in patients with multiple lithiasis and of size between 2 and 3cm, F-URS is an alternative technique to PCNL with a similar efficacy and complication rate, shorter hospital stay, faster recovery, and shorter surgical time. In contrast, F-URS has higher re-admission rates and requires a greater number of ancillary procedures.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Pieras E, Tubau V, Brugarolas X, Ferrutxe J, Pizá P. Análisis comparativo entre nefrolitotomía percutánea y ureteroscopia flexible en litiasis renal de 2–3cm. Actas Urol Esp. 2017;41:194–199.