To perform a comparative analysis of indirect and direct costs of two minimally invasive techniques (extracorporeal shock wave lithotripsy (ESWL) vs. ureteroscopy with holmium laser (URS/RIRS)) for the treatment of renal/ureteral calculi smaller than 2 cm.
Material and methodsProspective, comparative, non-randomized study of 84 patients treated for kidney stones smaller than 2 cm between January and December 2016. Of these, 38 (45.67%) were treated with ESWL (18 renal lithiasis and 20 ureteral lithiasis) and 46 (54.32%) with URS/RIRS (22 renal lithiasis and 24 ureteral lithiasis). A total of 19 (41.3%) patients in the URS/RIRS group and 15 (39.5%) patients in the ESWL group were actively working before treatment. The variables analyzed were sex, age, number and size of lithiasis, time (days) off from work due to treatment, estimate of indirect cost due to labor productivity loss and direct treatment costs including follow-up (total number of procedures, ancillary care, visits and diagnostic tests). The 2015 Wage Structure Survey (INE) was used to estimate the indirect cost. In addition, the “Work Productivity and Activity Impairment” (WPAI) questionnaire was also used to determine the level of perceived productivity loss.
ResultsThe mean number of sessions until lithiasis resolution was achieved was 2.57 for the ESWL group and 1.04 for the URS. The mean number of days off from work in the URS group was 7.16 days and 3.18 (p = 0.034) in the ESWL group. The total indirect costs resulting from productivity loss were EUR 621.55 and EUR 276.05 for the URS and ESWL, respectively. Direct costs in the ESWL group were EUR 1382.9 and EUR 2317.71 in the URS group. The level of work impairment perceived by patients undergoing URS was 18.88% and 21.33% in the ESWL group. The degree of impairment for performing activities of daily living was 24.44% in the URS and 15% in ESWL.
ConclusionsThe ESWL technique requires a higher number of sessions for the resolution of kidney stones under 2 cm, but it has a lower impact on total costs and on the perceived degree of affectation.
Analizar de forma comparativa los costes indirectos y directos de dos técnicas mínimamente invasivas (litotricia extracorpórea (LEOC) vs ureterorrenoscopia-láser holmium (URS/RIRS)) para el tratamiento de la litiasis reno-ureteral menor de 2 cm.
Material y métodosEstudio prospectivo y comparativo, no aleatorizado de 84 pacientes tratados por litiasis reno-ureteral menor de 2 cm entre enero y diciembre de 2016. De estos, 38 (45,67%) se trataron con LEOC (18 litiasis renales y 20 litiasis ureterales) y 46 (54,32%) con URS/RIRS (22 litiasis renal y 24 litiasis ureteral). Un total de 19 (41,3%) pacientes estaban activos laboralmente en el grupo de URS/RIRS y 15 (39,5%) pacientes en el grupo de LEOC. Las variables analizadas fueron sexo, edad, número y tamaño de las litiasis, días de baja laboral debido al tratamiento, estimación del coste indirecto por la pérdida de productividad laboral y el coste directo del tratamiento aplicado incluyendo el seguimiento (número total de procedimientos, procedimientos auxiliares, visitas y pruebas diagnósticas). Para la estimación del coste indirecto se empleó la Encuesta de Estructura Salarial 2015 (INE). Además también se utilizó el cuestionario “Work Productivity and Activity Impairment” (WPAI) para determinar el grado de percepción de pérdida de productividad.
ResultadosEl número medio de sesiones hasta la resolución de la litiasis fue de 2,57 para el grupo de LEOC y de 1,04 para la URS. El promedio de días de baja laboral en el grupo de la URS fue de 7,16 días, mientras que en el caso de la LEOC fue de 3,18 (p = 0,034). Los costes indirectos totales derivados de la pérdida de productividad fueron de 621,55 euros y de 276,05 euros para la URS y LEOC respectivamente. Los costes directos en el grupo de la LEOC fueron de 1382,9 euros y 2317,71 euros en el grupo de la URS. El grado de afectación en el trabajo percibido por los pacientes sometidos a URS fue del 18,88% y del 21,33% en el grupo de LEOC. El grado de afectación para realizar actividades cotidianas fue del 24,44% en URS y del 15% en LEOC.
Conclusionesla LEOC es una técnica que precisa de un mayor número medio de sesiones para la resolución de la litiasis reno-ureteral menor de 2 cm, pero con una menor repercusión en los costes totales y en la percepción del grado de afectación.
Lithiasis is a prevalent disease, estimated between 7% and 13% in the United States, between 5% and 9% in Europe and between 1% and 5% in Asia.1 In Spain, the mean incidence of urolithiasis is 0.73%, corresponding to 325,079 new cases per year and a prevalence of 5.06%, equivalent to 2,233,214 cases.2 This pathology is characterized by its high recurrence rate, which ranges from 40% to 60% at five and 9 years, respectively.3 Moreover, we have seen a rise in its prevalence in recent years, especially in more industrially developed countries.4 In some areas, the estimated increase over the last 20 years is higher than 37%.5
For the active treatment of renal and ureteral lithiasis under 2 cm, the two most widely used techniques are extracorporeal lithotripsy (ESWL) and laser ureterorenoscopy (URS). The use of one or the other technique depends on the characteristics of the lithiasis, the anatomy of the urinary tract and the body habitus of the patient. Thus, factors that are not favorable for treatment with ESWL are cystine, calcium oxalate monohydrate and brushite lithiasis, lithiasis with high radiological densities (>1000 Hounsfield Units), unfavorable anatomical factors, patients with skin-to-stone distance, anatomical abnormalities or contraindications for performing this technique.6
The symptoms can often be disabling. For this reason, this pathology has a high impact on the patient's quality of life and causes repercussions on his/her productivity both at work and in their daily activity. In the same way, it conditions a high demand for assistance, increasing healthcare costs. Thus, the cost of this disease has escalated to $5.3 billion in the United States in 2014,7 with lithiasis currently being the second most expensive urological disease.
The objective of our study is to comparatively evaluate the direct and indirect costs derived from the treatment of renal-ureteral lithiasis under 2 cm, using two minimally invasive techniques: ESWL and URS.
Material and methodsA prospective study was conducted between January and December 2016, including 81 patients consecutively diagnosed with renal or ureteral lithiasis under 2 cm and with indication for active treatment. The choice of the technique to be applied in each case for the treatment of lithiasis (ESWL or URS) was carried out according to usual clinical practice and in accordance with the recommendation guidelines of the European Association of Urology (EAU). In this way, URS treatment was indicated in case of lower calyx lithiasis with unfavorable factors for ESWL (narrow infundibulum < 5 mm, length > 10 mm or steep infundibular-pelvic angle), in case of lithiasis with attenuation coefficient > 1. 000 HU or long skin-stone distance > 10 cm on CT, in case of contraindication of ESWL (bleeding diathesis, pregnancy, anatomical obstruction distal to the stone, severe obesity or arterial aneurysm close to the stone), or in case of distal ureteric stones in young women (to avoid the effect of ESWL on the ovary).8 In those cases where both options were valid, the choice of technique was made by consensus with the patient according to his or her preference.
In the ESWL group, treatment was done on an outpatient basis. A Siemens Lithoskop electromagnetic lithotripter was used, with location of the lithiasis with an integrated fluoroscopy system. In all cases, the procedure was performed under analgesia/sedation with intravenous (iv) pethidine hydrochloride at doses ranging from 20-50 mg, depending on patient weight and treatment tolerance, and with a premedication of 4 mg iv ondansetron. In selected cases 0−2 mg iv midazolam was associated. The average waves received per session was 5200 (±1500), at a trigger frequency of 120 shock waves per minute, with the maximum intensity reached varying according to the patient's tolerance and the location of the stone.
In the URS/RIRS group, the procedure was performed as an inpatient procedure under general anesthesia. The endoscopic access was first carried out with a semi-rigid ureterorenoscope (Karlz Storz®), after the passage of a safety guidewire. If the stone was located in the upper part of the lumbar ureter or at the pyelocaliceal level, a flexible ureterorenoscope Flex X2 (Karlz Storz®) with previous ureteral access sheath passage (Retrace® or Navigator®) was used. The fragmentation source employed was a Holmium laser Ho:YAG (Auriga XL Boston Scientific®). The fiber used was 270 μm. Both laser settings for vaporization (0.5 J, 18 Hz) and fragmentation (1.2–2.5 J, 8 Hz) were used at the surgeon's discretion according to stone hardness. Leaving a double J stent for a maximum of two weeks in 90% of the cases, in cases of great manipulation, ureteral injuries, ureteral stenosis or long surgeries (never exceeding one hour).
The follow-up of the patients varied according to the technique applied. In the case of the ESWL group, they were monitored for seven to 10 days after treatment. In case it was not effective, a new treatment was carried out seven to 10 days after the consultation. In the case of the URS group, they were evaluated at 15–21 days. The imaging test used was the abdominal X-ray and ultrasound in cases with intensely radiopaque stones or a CT scan in cases of weakly radiopaque or radiolucent stones.
The technique was considered effective if the patient had no residual stones or clinically insignificant residual fragments (< 3 mm) persisted at three months follow-up.
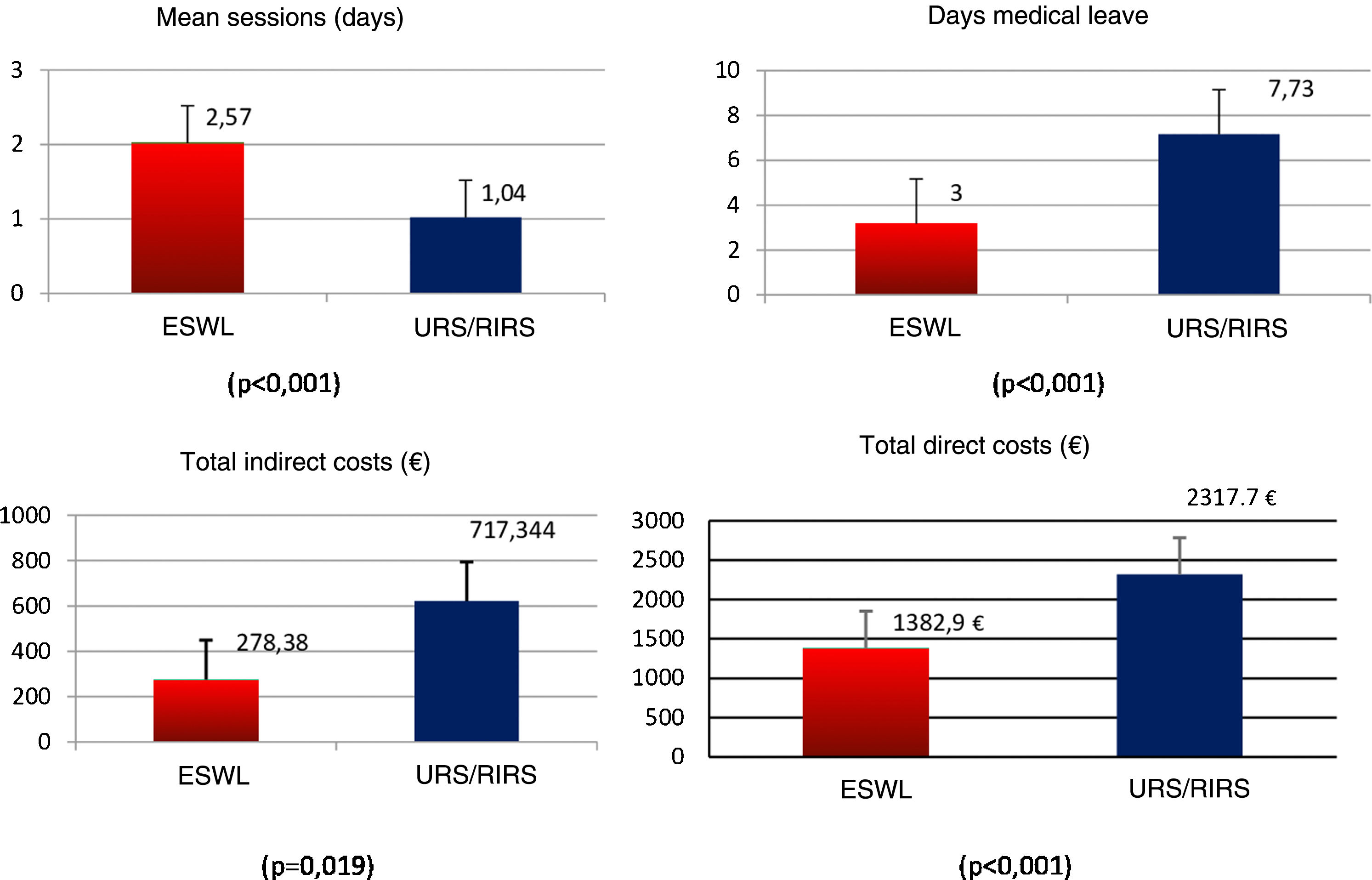
For each patient included in the study, we assessed their employment status and the days of medical leave required until the resolution of the lithiasis (taking into account the days allocated to the procedure and subsequent recovery). For employed patients, the indirect costs of the days of medical leave to the patient were estimated in each case, by calculating the monthly earnings from the Structure of Earnings Survey 2014 (NSI). In turn, direct cost data were calculated using the total number of treatments and auxiliary procedures, as well as follow-up costs. This information was obtained from the financial information system of the hospital (FIS). To evaluate the patient's perceived work productivity and daily activity impairment, the “Development of the Work Productivity and Activity Impairment (WPAI) Questionnaire”9 validated in Spanish was administered (Fig. 1). Questions 5 and 6, both Likert type, from 0 to 10, were analyzed.
The SPSS version 21 software was used for statistical analysis. The T Student statistical test was used for the comparison of quantitative variables if they followed a normal distribution or the Mann-Whitney U in case of non-parametric distribution. The Chi-square test was used for the comparison of qualitative variables. All statistical tests were carried out with a statistical significance of 0.05 and estimates with a 95% confidence interval (Fig. 1).
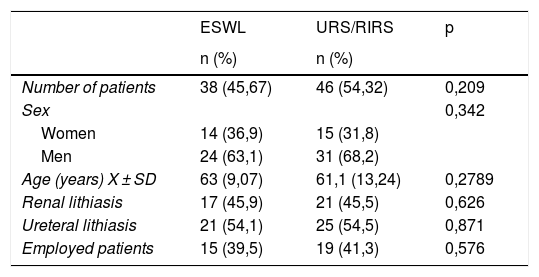
ResultsA total of 38 patients (45.67%) were treated with ESWL and 46 (54.32%) with URS/RIRS. The descriptive and comparative analysis of the demographic variables according to the treatment received are represented in Table 1.
Descriptive and comparative analysis of the main demographic variables according to treatment groups.
| ESWL | URS/RIRS | p | |
|---|---|---|---|
| n (%) | n (%) | ||
| Number of patients | 38 (45,67) | 46 (54,32) | 0,209 |
| Sex | 0,342 | ||
| Women | 14 (36,9) | 15 (31,8) | |
| Men | 24 (63,1) | 31 (68,2) | |
| Age (years) X ± SD | 63 (9,07) | 61,1 (13,24) | 0,2789 |
| Renal lithiasis | 17 (45,9) | 21 (45,5) | 0,626 |
| Ureteral lithiasis | 21 (54,1) | 25 (54,5) | 0,871 |
| Employed patients | 15 (39,5) | 19 (41,3) | 0,576 |
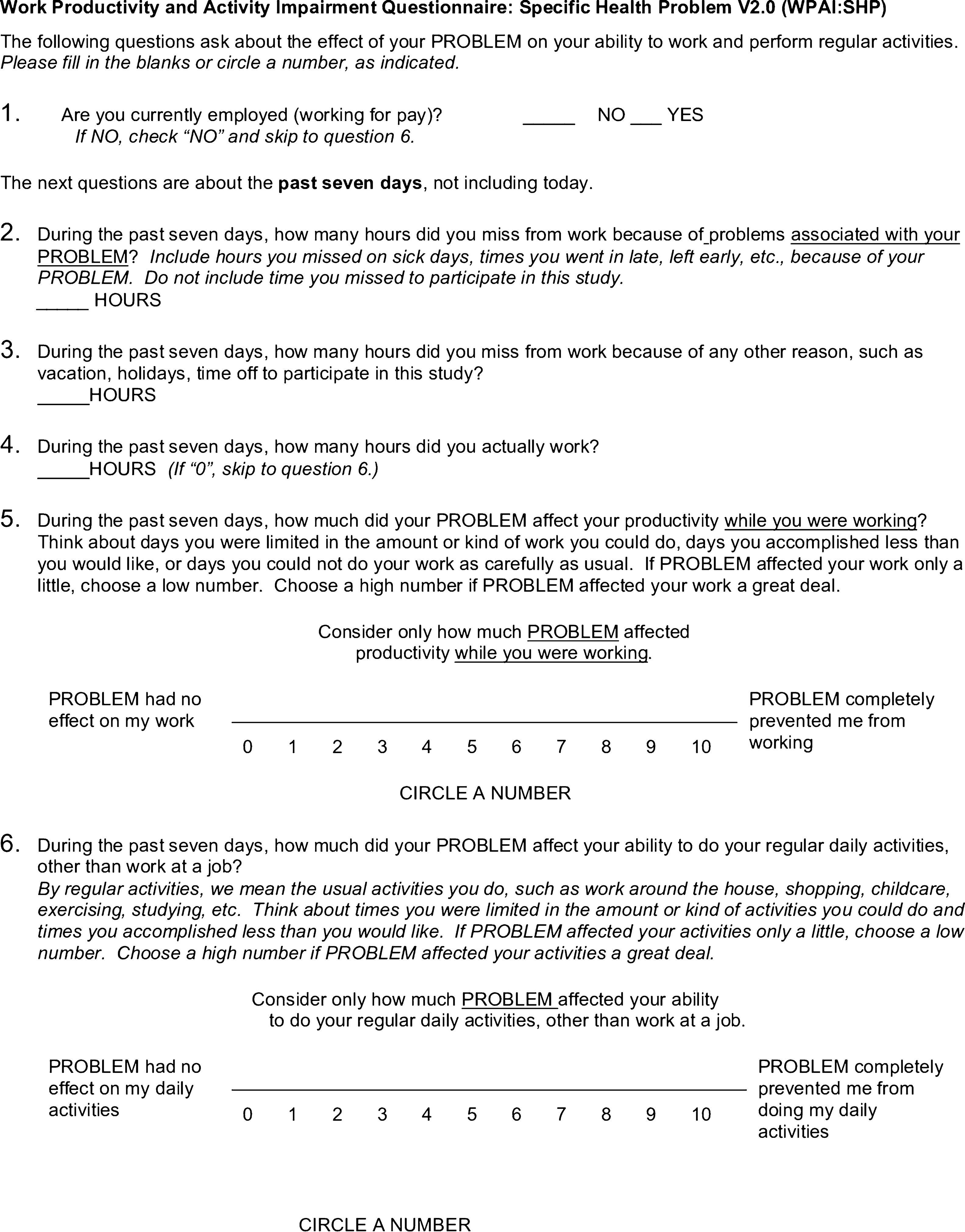
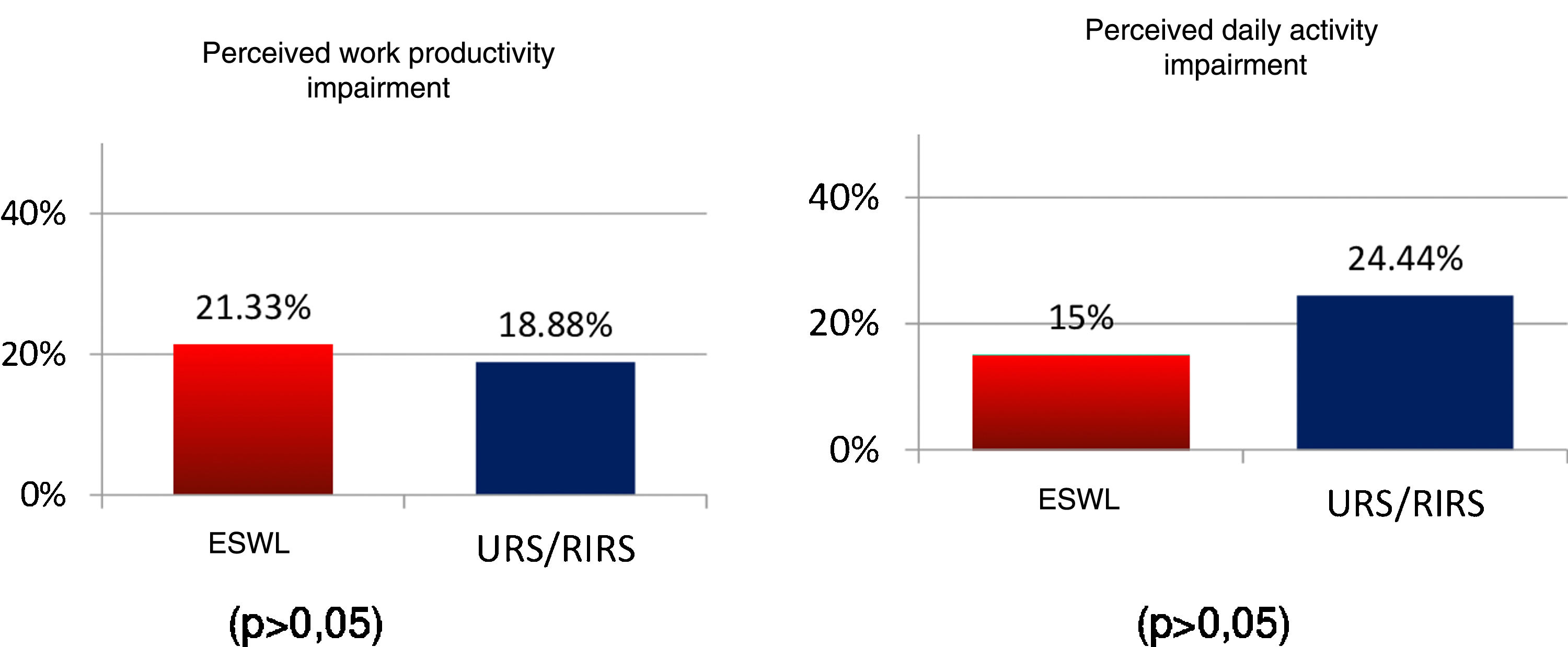
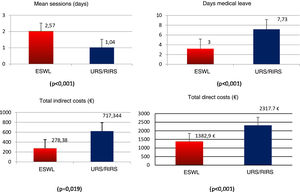
The mean number of sessions required until resolution of lithiasis was 2.57 (±1.46) in the ESWL group, compared to 1.04 (±0.20) in the URS/RIRS group (p < 0.0001). Considering employed patients, the mean number of medical leave days required until resolution of the lithiasis was 3 (±2.32) days for those who received ESWL, compared to 7.73 (±8.94) days for patients who underwent URS/RIRS (p < 0.0001). The estimated average indirect costs for these medical leave days was €278.38 (±216.21) in the ESWL group compared to €717,344 (±830.51) in the URS/RIRS group (p = 0.019). The direct costs derived from the total number of treatments and ancillary procedures, as well as the mean follow-up costs was €1,382.9 (±784.4) in the ESWL group compared to €2,317.71 (±457.96) in the URS/RIRS group (p < 0.0001) (Fig. 2). Mean hospital stay was 1.2 days (±0.4) for URS/RIRS patients.
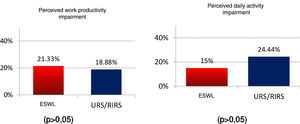
The results of the WPAI questionnaire, in terms of the patient's perceived work productivity impairment, we found that the percentage of impairment was 18.88% for the URS group and 21.33% for the ESWL group. With regard to the perceived daily activity impairment, we found a level of impairment of 24.44% for the URS group compared to 15% for the ESWL group, with no statistically significant differences observed (Fig. 3).
DiscussionTo our knowledge this is the first study that compares and evaluates the overall costs (direct and indirect) between two widely accepted techniques for the treatment of renal-ureteral lithiasis under 2 cm. In most published studies comparing different treatments for renal-ureteral lithiasis in the literature, the most common variables have been lithiasis-free rate and the complications associated with each technique. In fact, the most relevant recommendation guidelines base their indications exclusively on these variables and on series of centers with a high number of cases and experience. However, the costs associated with active treatment of lithiasis are very high, mainly due to the technological development of endourological treatments and the cost of the ancillary devices employed.7
After this analysis, we can say that cost-effectiveness studies in this pathology are necessary to help the clinician make decisions, extending their critical capacity by incorporating the cost variable in the shared decision making. In recent years, the presence of this type of study has increased in the scientific literature, but with a wide variability in the results obtained, depending on each specific country, health system, geographical area and even hospital type.10,11 This variability hinders extrapolation of results, due to significant differences in costs between countries or even regions within the same country, as well as in the procedures associated to each treatment. However, these studies do not analyze the indirect costs associated with medical leave, loss of productivity or the inability to carry out everyday activities. These are relevant aspects to consider if we involve the patient in decision making and address his/her preferences based on recovery time or impact on their work or daily activity.
Current trends in the treatment of renal-ureteral lithiasis show an increase in retrograde endourological techniques to the detriment of extracorporeal lithotripsy, with the use of percutaneous nephrolithotomy remaining stable in its standard and miniaturized variants.12 This trend is due to the significant technological development in the field of endourology and the possibility of addressing increasingly complex cases or challenges. However, there are important variations in the choice of technique according to the countries analyzed.
However, lithiasis-free rate plays a key role in choosing one or the other technique. If the lithiasis-free rate in ESWL does not exceed 64%, the model seems to predict that this technique is not cost-effective.13 In our series, this value is of 79.1% for renal lithiasis in the first session and 93.8% for ureteral lithiasis. In terms of costs, we find that the costs of a session of ESWL is €286.06 and €1,409.89 for a URS, finding in this way that the first line combination of ESWL with URS as an alternative is better than a first line treatment with URS. As in the case of renal lithiasis, the mean cost of ESWL was €1,069.53, while in the case of RIRS/URS it was €2,841.06. In our experience, with more than 350 patients analyzed, ESWL is more cost-effective for renal-ureteral lithiasis smaller than 2 cm.14
Lotan et al. concluded in their initial studies that the economic analysis of this pathology is very complex and must take into account several factors.15 There is a meta-analysis that includes only 12 studies, and its conclusion seems to differ from our results.16 They mention a great risk of bias in their study, since the samples are too heterogeneous, differing in the costs of both techniques by more than 100 times the price among several studies; therefore, the results obtained may be biased.
Patients in the URS/RIRS group have been treated on an inpatient basis. This fact makes us wonder why URS/RIRS expenses are so high in comparison to ESWL in our studies.17 However, the costs of an admission in our hospital does not imply an important increase in the overall costs of the technique, since the difference is €127.7 (€417.21 with admission and €289.51 for ambulatory treatment). Another variation we may find, which is not described in these studies, is the possibility of not using a double J stent in such procedures. In our series, a double J stent was placed after URS/RIRS for a maximum of 2 weeks. This way, the days off from work could be justified. However, in Spain, patients are entitled to one week of medical leave after surgery. In addition, we can find that the mean shock wave numbers are higher in our series than in those exposed in the meta-analysis by Geraghty et al. We carried out this scheme because the application of a higher number of waves has been shown to be more effective with a similar safety profile.18 All these, and the choice of the technique based on the composition, size, location and anatomy of the patient, can make our results more cost-effective than other studies.
On the other hand, if we talk about the WPAI questionnaire, we observe a similar work productivity impairment (slightly higher in the ESWL group). In contrast to the daily activity impairment which is higher in the URS/RIRS group, evidently because of the stent placement. However, these differences are not statistically significant enough to make any statements.
The main limitations of our study have been the impossibility of stratifying and analyzing patients according to the size and location of lithiasis, due to a small sample size. Still, the completion of the surveys is voluntary and not all patients cooperate with their participation. In turn, the use of the double J stent in patients treated by URS/RIRS could behave as a bias in the comparative study with ESWL. However, the study reflects the reality of our clinical practice and analyses costs in a real treatment setting, so in our opinion, it cannot be considered a bias. The absence of randomization may also be a limitation, but it was excluded because it is not ethically correct to offer a less effective technique in patients who are candidates for one technique or another.
ConclusionAccording to the results of our study, extracorporeal lithotripsy is shown to be a technique with lower direct and indirect costs than ureterorenoscopy for the treatment of renal-ureteral lithiasis under 2 cm.
FundingThe authors state that they have not received any funding.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Perez-Ardavin J, Lorenzo L, Caballer-Tarazona V, Budía-Alba A, Vivas-Consuelo D, Bahilo-Mateu P, et al. Análisis comparativo de costes directos e indirectos de dos técnicas mínimamente invasivas, para el tratamiento de la litiasis renoureteral menor de 2 cm. Actas Urol Esp. 2020;44:505–511.