Transurethral resection of the prostate is the gold standard of surgical treatment of lower urinary tract symptoms associated to benign prostate hyperplasia. The new GreenLight PhotoVaporization has been shown to be an alternative that is as effective for this condition as the transurethral resection of the prostate.
ObjectivesTo compare the efficiency of GreenLight PhotoVaporization 120W versus transurethral resection of the prostate in the treatment of benign prostate hyperplasia (BPH) in a 2-year time horizon from the Spanish health service perspective.
MethodsA cost utility analysis was performed retrospectively with the data from 98 patients treated sequentially with transurethral resection of the prostate (n: 50) and GreenLight PhotoVaporization 120W (n: 48). A Markov model was designed to estimate the cost (2012€) and results (quality adjusted life years) in a 2-year time horizon.
ResultsThe total cost associated to GreenLight PhotoVaporization 120W treatment was less (3377€; 95% CI: 3228; 3537) than that of the transurethral resection of the prostate (3770€; 95% CI: 3579; 3945). The determining factor of the cost was the surgical phase (difference: −450€; 95% CI: −625; −158) because admission to hospital after surgery was not necessary with the GreenLight-PhotoVaporization.
ConclusionsSurgical treatment of BPH patients with GreenLight-PhotoVaporization 120W is more efficient than transurethral resection of the prostate in the surgical treatment of benign prostate hyperplasia as it has similar effectiveness and lower cost (−393€; 95% CI: −625; −158).
El gold standard del tratamiento quirúrgico de la sintomatología del tracto urinario inferior asociado a la hiperplasia benigna de próstata ha sido la resección transuretral de la próstata; GreenLight-PhotoVaporization ha demostrado ser una alternativa quirúrgica tan efectiva como aquella.
ObjetivoAnalizar la eficiencia comparada, en un horizonte temporal de 2 años, de GreenLight-PhotoVaporization 120W respecto de la resección transuretral de la próstata en el tratamiento quirúrgico de la hiperplasia benigna de próstata desde la perspectiva del sistema de salud de España.
MétodosSe realizó un análisis de coste utilidad a partir de los resultados obtenidos retrospectivamente en 98 pacientes intervenidos secuencialmente mediante resección transuretral de la próstata (n: 50) y GreenLight-PhotoVaporization 120W (n: 48). Se utilizó un modelo de Markov para estimar el coste (€, 2012) y los resultados (años de vida ajustados a calidad) tras un seguimiento de 2 años.
ResultadosEl coste total asociado al tratamiento con GreenLight-PhotoVaporization 120W fue inferior (3.377€; IC 95%: 3.228; 3.537) al de la resección transuretral de la próstata (3.770€; IC 95%: 3.579; 3.945). El determinante del coste se presenta en la fase quirúrgica (diferencia: −450€; IC 95%: −625; −158) debido a que GreenLight-PhotoVaporization 120W no precisaba ingresar al paciente tras la cirugía.
ConclusionesEl tratamiento quirúrgico de los pacientes con HBP mediante GreenLight-PhotoVaporization 120W muestra mayor eficiencia respecto de la resección transuretral de la próstata al observarse una efectividad similar y un coste inferior (−393€; IC 95%: −625; −158).
Benign prostate hyperplasia (BPH) has a high prevalence in men and is a common cause of medical consultations. Lower urinary tract inferior symptoms (LUTS) associated with BPH dramatically reduce patient quality of life.
The gold standard surgical treatment is transurethral resection of the prostate (TURP). The incorporation of 120W GreenLight PhotoVaporization (120W GL PV) represents a breakthrough in the field of urology, enabling minimally invasive surgery and increasing quality of life.1–3 Nevertheless, as with any new health technology, the technique has to be economically assessed to show the funding agency for the health system that its use represents an efficient allocation of resources.
The objective was to analyze the efficiency (over a time period of 2 years) of 120W GL PV compared with TURP in the surgical treatment of BPH.
MethodsWe conducted a cost–utility analysis based on the data retrospectively obtained from 2 samples of patients who had undergone surgery. To this end, we designed a decision model to estimate the total cost of the resources used and the results obtained after a 2-year follow-up.
Surgical alternativesThe patients assessed in this study underwent either TURP or 120W GL PV.
PopulationNinety-eight patients who presented LUTS secondary to BPH were included in the analysis. Fifty patients underwent TURP and 48 patients underwent 120W GL PV.
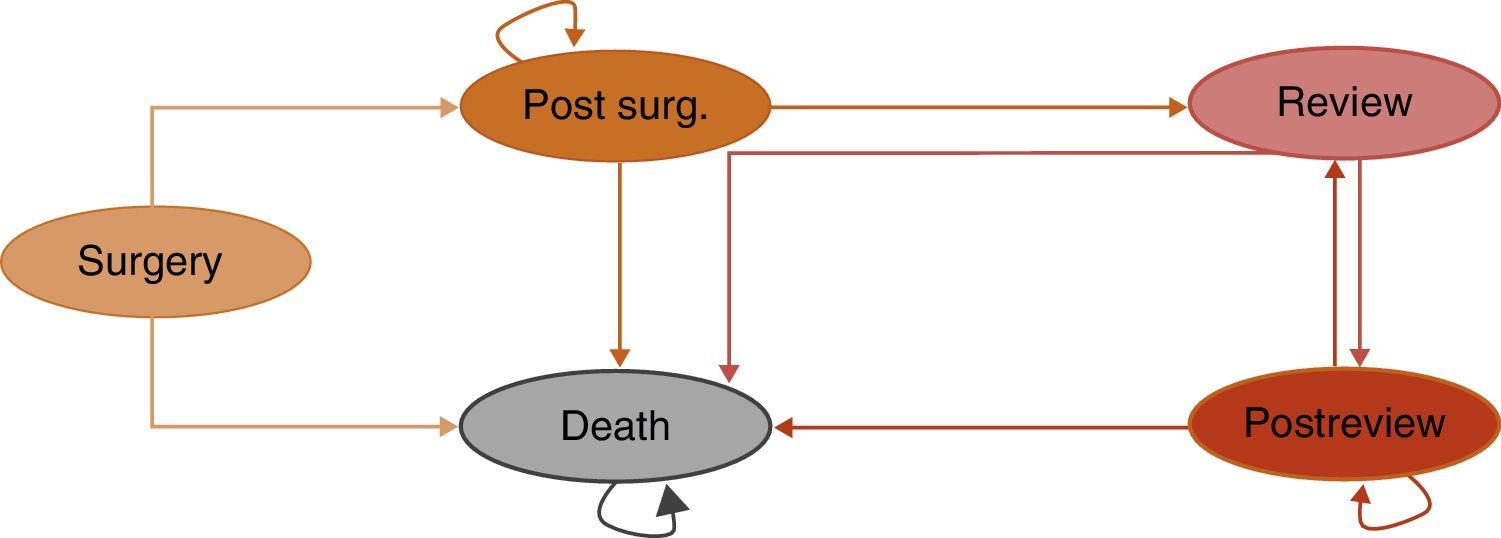
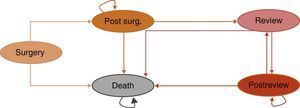
ModelWe chose a Markov model as the decision model (Fig. 1), given that it reproduces with considerable fidelity the diseases in which the patients can progress through various health stages in both directions. In other words, patients can go from a controlled health condition to a poorer one at any given moment and can subsequently recover, returning to their initial state. This progression can be repeated at any moment.
The analysis was performed with a 2-year time horizon, coinciding with the follow-up time of the patients who underwent surgery. For this reason, we applied a 3% discount rate for both costs and results, starting the first year. During this time, we analyzed the costs and results of patients during fixed time periods, called Markov cycles, lasting 1 month. The perspective adopted for the analysis was that of Spain's health system, thereby incorporating only those resources that are directly financed by the system.
The patients could move through 5 comprehensive and exclusive health states; that is, there were no other possible health states and patients could only be in a single health state at any given moment. At the end of each cycle, the patients could be in the same health state or have moved to another. The health states were as follows:
- -
Surgery: the patients undergo surgery through one of the analyzed surgical alternatives.
- -
Postsurgery: the condition of patients after surgery.
- -
Review: defined as the condition in which the patients undergo a reoperation with TURP.
- -
Postreview: analogous to postsurgery, after the reoperation.
- -
Death: as the result of any cause.
For the economic analysis, effectiveness was defined as quality-adjusted survival, expressed in quality-adjusted life-years (QALYs). These were estimated based on the product of the overall survival (measured as life-years gained [LYG]) and the utility value of each health state, as taken from the literature.4–7 The utility expresses the patient's preference for a certain health state. Its value varies mainly between 0 (for the poorest perceived condition) and 1 (for a perfect health state). Given that utility decreases progressively with age, its value was estimated by discounting the disutility value corresponding to each age.
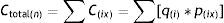
Cost dataThe costs (expressed in 2012€) were calculated based on the patients’ healthcare resource consumption during a 2-year time period as follows:
Ctotal(n), total cost of the alternative (n); q(ix), number of units of the healthcare resource used (i) in the phase (x); p(ix), unit price of the resource (i) in the phase (x). The unit prices used in the model were taken from recent publications that conducted research in urology.8–14The cost of each alternative treatment was determined based on the costs associated with the surgical procedure, with the surgical revisions and with the complications that occurred. The surgical procedure was divided into 3 separate phases: preoperative, perioperative and postoperative. The preoperative phase encompassed the period starting with the medical decision to operate and ending on the day of the surgery. The perioperative phase consisted exclusively of the surgery itself. The postoperative phase encompassed the consumption of resources from the end of the surgery to 2 years later.
The cost of the reinterventions was calculated according to the estimated incidence probability. The cost of the complications was calculated based on the cumulative incidence observed in the analyzed patient sample. The cost of the necessary equipment for the 120W GL PV was determined assuming one duration of 3 years and one use average of 100 interventions annually.
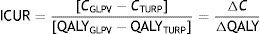
Efficacy analysisThe efficiency is calculated using the incremental cost–utility ratio (ICUR), which expresses the incremental cost necessary to achieve an additional QALY with the evaluated alternative (120W GL PV) as a substitute for the comparison (TURP):
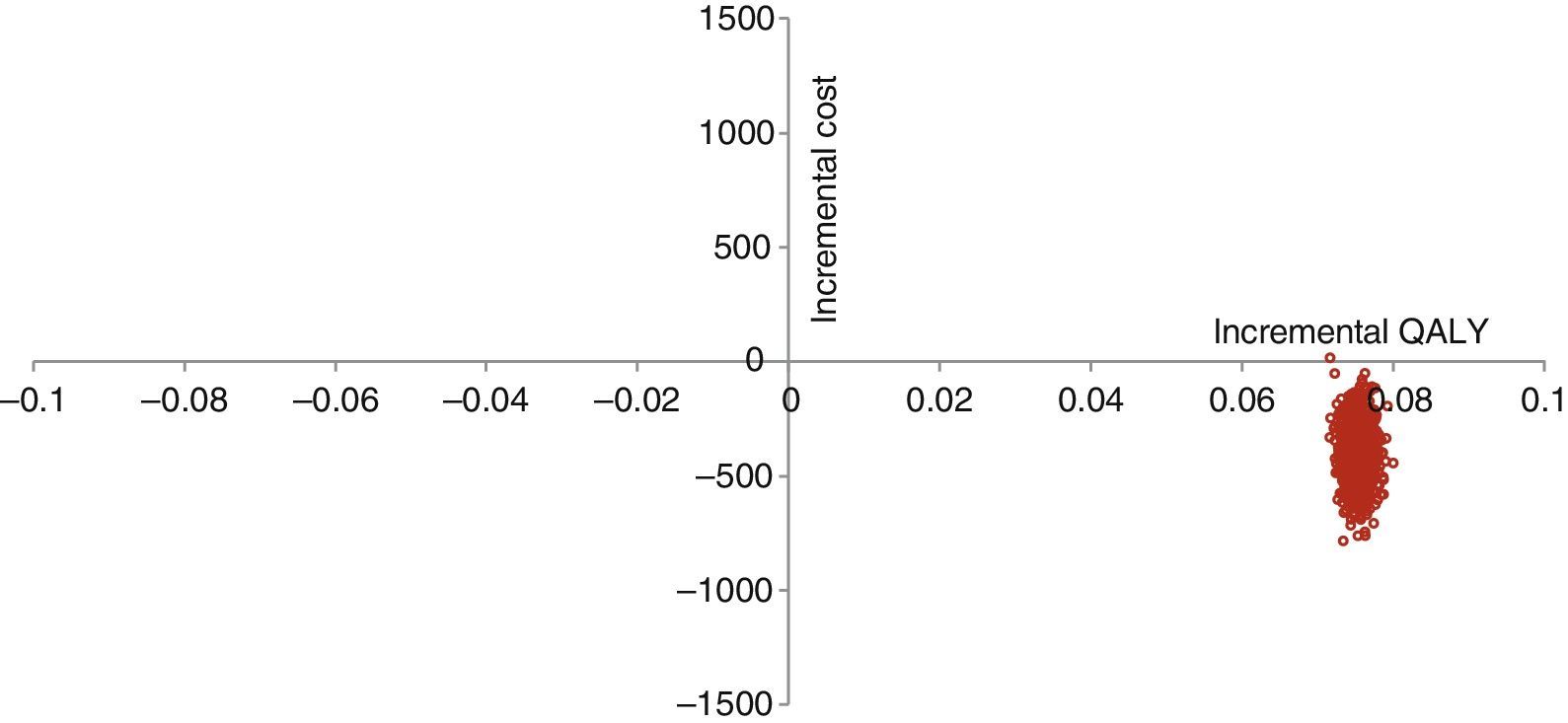
with ΔC representing the difference between the total cost of the 2 alternatives and ΔQALY the effectiveness results for each alternative.Sensitivity analysisVarious univariate and bivariate analyses were performed by modifying the most relevant variables: the incidence and cost of complications and reinterventions, cost of the equipment, postoperative costs and discount rates for costs and results. These changes were performed within a plausible range of values to evaluate the robustness of the results. We also performed a Monte Carlo simulation with 1000 iterations to analyze the second order uncertainty associated with the parameters.
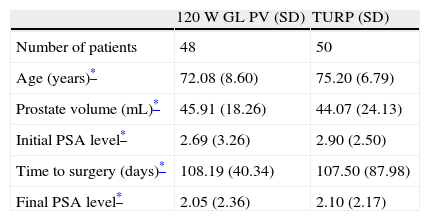
ResultsThe characteristics of the analyzed patient sample in the decision model are shown in Table 1.
Characteristics of the patient sample.
| 120W GL PV (SD) | TURP (SD) | |
| Number of patients | 48 | 50 |
| Age (years)* | 72.08 (8.60) | 75.20 (6.79) |
| Prostate volume (mL)* | 45.91 (18.26) | 44.07 (24.13) |
| Initial PSA level* | 2.69 (3.26) | 2.90 (2.50) |
| Time to surgery (days)* | 108.19 (40.34) | 107.50 (87.98) |
| Final PSA level* | 2.05 (2.36) | 2.10 (2.17) |
Abbreviations: 120W GL PV, 120W GreenLight PhotoVaporization; TURP, transurethral resection of the prostate; SD, standard deviation.
In the 120W GL PV sample, we observed (in the checkup performed after the surgery) 3 cases of urethral stenosis, which required reoperations (internal urethrotomy). In the TURP group, we observed 1 case of meatus plasty and 2 cases of urethral stenosis, which required urethroplasty and urethrotomy, respectively. Based on these data, we calculated the probability of the incidence of complications.
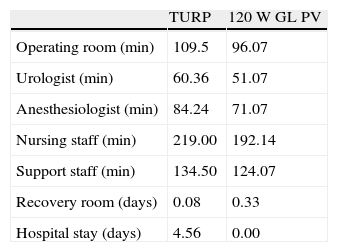
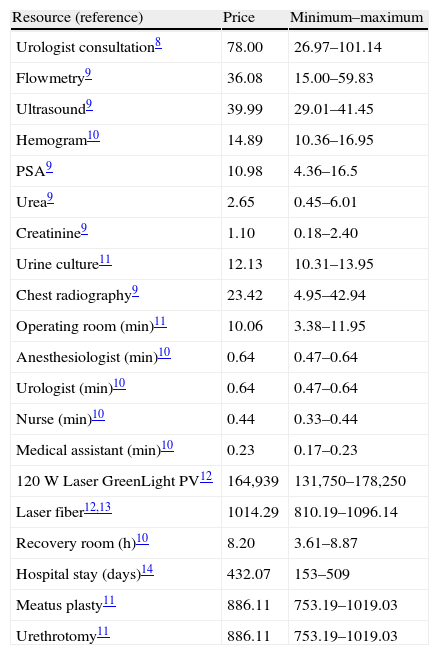
The use of healthcare resources showed no significant differences, except for those directly associated with the surgery and the length of the hospital stay (Table 2); the unit prices are indicated in Table 3.
Unit prices of the healthcare resources used.
| Resource (reference) | Price | Minimum–maximum |
| Urologist consultation8 | 78.00 | 26.97–101.14 |
| Flowmetry9 | 36.08 | 15.00–59.83 |
| Ultrasound9 | 39.99 | 29.01–41.45 |
| Hemogram10 | 14.89 | 10.36–16.95 |
| PSA9 | 10.98 | 4.36–16.5 |
| Urea9 | 2.65 | 0.45–6.01 |
| Creatinine9 | 1.10 | 0.18–2.40 |
| Urine culture11 | 12.13 | 10.31–13.95 |
| Chest radiography9 | 23.42 | 4.95–42.94 |
| Operating room (min)11 | 10.06 | 3.38–11.95 |
| Anesthesiologist (min)10 | 0.64 | 0.47–0.64 |
| Urologist (min)10 | 0.64 | 0.47–0.64 |
| Nurse (min)10 | 0.44 | 0.33–0.44 |
| Medical assistant (min)10 | 0.23 | 0.17–0.23 |
| 120W Laser GreenLight PV12 | 164,939 | 131,750–178,250 |
| Laser fiber12,13 | 1014.29 | 810.19–1096.14 |
| Recovery room (h)10 | 8.20 | 3.61–8.87 |
| Hospital stay (days)14 | 432.07 | 153–509 |
| Meatus plasty11 | 886.11 | 753.19–1019.03 |
| Urethrotomy11 | 886.11 | 753.19–1019.03 |
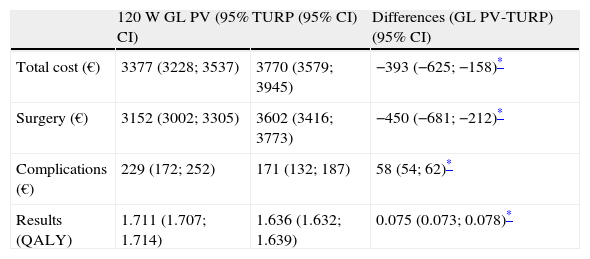
The mean total cost calculated for the surgery with 120W GL PV was less than that for TURP, while the effectiveness of GL PV was greater than that of TURP (Table 4). The Monte Carlo simulation with 1000 iterations showed that the difference in cost between the 2 surgical alternatives was statistically significant. The breakdown of the items in the total cost showed that those corresponding to the postoperative phase constituted the cost determinant as a function of the hospital stay. The graphical representation in the incremental cost effectiveness plane showed that 120W GL PV is a dominant option for its greater effectiveness (0.075 QALY) and lower cost (−393€) (Fig. 2).
Total cost and breakdown by items of surgeries performed.
| 120W GL PV (95% CI) | TURP (95% CI) | Differences (GL PV-TURP) (95% CI) | |
| Total cost (€) | 3377 (3228; 3537) | 3770 (3579; 3945) | −393 (−625; −158)* |
| Surgery (€) | 3152 (3002; 3305) | 3602 (3416; 3773) | −450 (−681; −212)* |
| Complications (€) | 229 (172; 252) | 171 (132; 187) | 58 (54; 62)* |
| Results (QALY) | 1.711 (1.707; 1.714) | 1.636 (1.632; 1.639) | 0.075 (0.073; 0.078)* |
Abbreviations: 120W GL PV, 120W GreenLight PhotoVaporization; TURP, transurethral resection of the prostate.
The univariate sensitivity analyses demonstrated the robustness of the results. The total cost of 120W GL PV was greater than that of TURP only under the following conditions: when the useful time of the 120W GL PV equipment was reduced to 1 year, when the number of operated patients at 1 year was reduced to 25 or when the cost of the hospital stay was reduced to 153€.
DiscussionThe results show that the alternative of 120W GL PV was dominant when compared with TURP due to the slightly greater effectiveness (0.075 QALY) of 120W GL PV and its lower cost (−393€) for each patient followed-up for 2 years. The cost associated with surgery was the main determinant of cost (3152€ and 3602€ respectively; difference: −450€). The breakdown of this cost in the analyzed phases indicated that the postoperative phase was responsible for this difference (2084€ and 214€, respectively; difference: 1870€), compensating for the increase in the surgical phase costs (1321€ and 2742€, respectively; difference: 1421€) associated with the equipment necessary for 120W GL PV.
As often happens with new healthcare technology, the unit price falls over time. The cost incurred by 120W GL PV has fallen from 550€ per patient to the current cost of 300€. This difference means that the current cost for the first 2 years of follow-up with 120W GL PV would be 3132€ instead of 3382€, which would mean increased cost savings.
Our effectiveness results are in line with those of controlled and randomized clinical trials with 2-year follow-ups that have evaluated 120W GL PV versus RTUP,1–3 showing a reduction in the length of hospital stay,15–17 although they do indicate an increased surgical time with 120W GL PV .15,16 Nevertheless, a previous study that analyzed a cohort of 50 patients showed that 120W GL PV can be used safely and satisfactorily in a major outpatient surgery regimen.18 In terms of the results of costs with 2-year follow-ups, Callejo et al.7 performed a systematic review and demonstrated that 120W GL PV is associated with a lower cost due to shorter hospital stays. An earlier review19 showed similar results, although it indicated that the interpretation of results was hindered by deficiencies in the design of the studies, as well as by the significant loss of patients during follow-up. Our results correlate with other economic assessments completed with 2-year horizons. Stovsky et al.20 calculated the total cost at $3589 and $4927 for 120W GL PV and TURP, respectively. In contrast, the economic evaluation by Callejo et al.7 showed a greater cost for the 120W GL PV alternative (3173€) than for TURP (2917€) due to the application in their decision model of a higher risk of reoperation with 120W GL PV (RR: 4.36). In our study, however, we observed 3 cases of reintervention (2 urethrotomies for urethral stenosis and 1 meatus plasty) in the TURP option and 3 cases of reintervention (for urethral stenosis treated with urethrotomy) with the 120W GL PV option, which explains the difference.
The results show similar effectiveness and a significantly lower cost and enable a more efficient allocation of scarce healthcare resources (a widespread healthcare problem), as well as increased patient wellbeing.
The study has a number of limitations. First, this was a retrospective nonrandomized study, which could diminish the internal validity of its results. Nevertheless, we evaluated the results from the same team of surgeons to reduce the differences of clinical practice. Second, the sample size was not very large, which increases the variability of the results. To compensate for the sample size, we conducted a resampling of 1000 iterations using the Monte Carlo simulation in the analyzed model to more accurately analyze the variability of the parameters. Third, the follow-up time was only 2 years, which could prevent the inclusion of all costs incurred and benefits obtained. However, in the analysis of the time to events, there were no significant variations starting from 18 months. Nevertheless, longer-term studies are needed to analyze this issue.
In light of the results, we can conclude that the surgical treatment of patients with BPH using 120W GL PV shows greater efficiency compared with transurethral resection of the prostate, due to the similar effectiveness but lower cost, thanks primarily to the fact that patients do not have to remain hospitalized after the surgery.
FundingThis study was funded by an unrestricted grant from American Medical Systems.
Conflicts of interestDr. A. Sanz-Granda, a specialist in the economic assessment of healthcare technology, received an unrestricted grant to conduct this study. Dr. J.M. Benejam Gual, R. García-Miralles Grávalos, A. Severa Ruíz de Velasco and J. Pons Viver have no conflicts of interest.
We would like to thank American Medical Systems for providing unrestricting funding for this study, without which the study would not have been possible.
Please cite this article as: Benejam-Gual JM, Sanz-Granda A, García-Miralles Grávalos R, Severa-Ruíz de Velasco A, Pons-Viver J. Análisis coste efectividad a 2 años del tratamiento quirúrgico de la hiperplasia benigna de próstata mediante vaporización fotoselectiva de la próstata con GreenLight-PhotoVaporization 120W versus resección transuretral de la próstata. Actas Urol Esp. 2014;38:238–243.