The COVID-19 pandemic caused by the SARS-CoV-2 virus has caused tens of thousands of deaths in Spain and has managed to breakdown the healthcare system hospitals in the Community of Madrid, largely due to its tendency to cause severe pneumonia, requiring ventilatory support. This fact has caused our center to collapse, with 130% of its beds occupied by COVID-19 patients, thus causing the absolute cessation of activity of the urology service, the practical disappearance of resident training programs, and the incorporation of a good part of the urology staff into the group of medical personnel attending these patients. In order to recover from this extraordinary level of suspended activity, we will be obliged to prioritize pathologies based on purely clinical criteria, for which tables including the relevance of each pathology within each area of urology are being proposed. Technology tools such as online training courses or surgical simulators may be convenient for the necessary reestablishment of resident education.
La pandemia COVID-19 causada por el virus SARS-CoV-2 ha ocasionado decenas de miles de muertos en España y logrado colapsar los hospitales de la red sanitaria en la Comunidad de Madrid, debido en gran parte a su particular tendencia a causar neumonías graves con necesidad de soporte ventilatorio. Este hecho ha ocasionado el colapso de nuestro centro, llegando a tener una ocupación del 130% de sus camas por enfermos COVID-19, y causando por tanto el cese absoluto de actividad del servicio de urología, la práctica desaparición de la docencia de los residentes y la incorporación de buena parte de la plantilla de urología al grupo de personal médico que atiende a estos pacientes. Para la recuperación de esta elevada cantidad de actividad suspendida será necesaria una priorización de la patología en base a criterios puramente clínicos, para la cual se proponen tablas que recogen la relevancia de cada patología dentro de cada área de la urología. Herramientas brindadas por la tecnología como la formación online o los simuladores quirúrgicos podrán ser útiles para la necesaria restitución de la formación de residentes.
Coronaviruses are RNA viruses which have originated common respiratory infections and are known since the mid-20th century. However, this family of viruses has caused two serious epidemics so far in the 21st century: SARS in 2002 and MERS in 2010.1 The latter, which is currently attacking us, and is more dangerous because of certain characteristics of its causative agent SARS-CoV-2, has become a global pandemic known as COVID-19, which has managed to put many of the world's most developed countries on guard, collapsing their health systems due to 3 main factors: its rapid spread, its high contagiousness and its special tendency to cause severe viral pneumonia requiring hospitalization, with high mortality in first world’s epidemiological scenario.2,3 Thus, in the specific case of Spain, the health network has collapsed in a short time, demanding the stewardship of material and human resources in the hospital setting for their allocation against the pandemic. Since the beginning of the epidemic declared in China at the end of 2019, and up to the date when this article is sent (8 April 2020), 1,353,361 cases have been reported worldwide,4 146,690 of them causing 14,555 deaths in Spain.5 And the Community of Madrid, where our institution provides assistance, has unfortunately been the hardest hit by the virus, representing almost 30% of the total Spanish population infected.
The strategy implemented by hospitals to flatten the contagion curve has been the absolute prioritization of the pandemic, progressively increasing the intensive care units (ICU) capacity and therefore reducing surgical activity to the minimum or, sometimes, to its complete suspension. And all this with the ultimate aim of increasing the number of free hospital beds, anesthesiology staff, medical personnel, personal protective equipment, cleaning products and operating rooms, so that they can be converted to ICUs. Therefore, following the recommendations of several scientific societies6,7 and previous experience reported by Italian,8–10 Middle Eastern11 or Far Eastern12 colleagues, the suspension of all scheduled non-oncological surgical activity (including ambulatory surgery and benign pathology) and the prioritization of uro-oncological pathology was carried out evaluating each case individually. All these integrated with the important nuance of trying to avoid admission to the ICU after surgery, which reduced the scheduled surgical procedures to a minimum. In addition, factors such as the presence of the virus in the stool,13 initial doubts about the validity of rapid disinfection procedures in endoscopy rooms or the excessive caution that accompanies any serious and unknown situation have also led to the suspension of countless relevant examinations for the diagnosis and follow-up of urological pathologies such as cystoscopies, prostate biopsies or non-urgent urological ultrasounds. Finally, as a last consequence of the above, and in addition to the very high rate of infection among the healthcare personnel, a high percentage of the staff of urology specialists and residents joined the medical team in charge of these patients in the inpatient wards, in addition to giving priority to urological emergencies and temporarily reinforcing shifts and continuing care of the specialty.
This pressing need for hospital beds, ventilators and ICU beds for COVID-19 patients has rapidly displaced medical care for other causes. Urology has been fully immersed in this dramatic public health problem caused by the pandemic, given the need to continue treating pathologies that compromise patient survival, as well as the obligation to perform urgent surgery and provide solutions to uro-oncology patients in the context of the difficult situations experienced in hospitals during this period. Urology covers the diagnosis, treatment and follow-up of 3 of the 10 cancers with the highest incidence in Europe,14 as well as high-prevalence pathologies such as lithiasis or benign prostatic hyperplasia, all being wiped out by SARS-CoV-2 in just a few days.
The number of new infection cases is supposed to decrease in the coming weeks, with the progressive availability of operating rooms and beds that will allow us to recover urological surgical activity in the hospitals of the Spanish health network. This situation will require a triage of the urological pathology based on its priority, which will allow an efficient use of the resources that are expected to be gradually restored, in order to adjust them to the predicted high demand as a consequence of the pause of previous weeks. If the initial difficulty of the pandemic from a urological point of view lay in the process of massively suspending all the activity of a high-volume service, the great challenge that lies ahead in the coming months will be to prioritize the multiplied activity expected when the critical phase of the disease is overcome in terms of public health. Therefore, the objective of this article is none other than to share the complex professional experience of adapting the urology service of a referral hospital to a pandemic of these dimensions, with different and difficult measures in each of its successive phases. And finally, creating a practical and concise guide that brings together our first-hand experience with the recommendations of several scientific societies and hospitals, in order to contribute on the recovery of urological activity suspended during this unfortunate health crisis.
Material and methodsNarrative presentation of the measures taken in our institution's urology department in the context of the initial phases of the COVID-19 pandemic, as well as a search in the main databases (Medline, Embase) to identify studies and reports related to the impact of the pandemic on our specialty. No language or year restrictions were applied, and the bibliography of the included studies was reviewed as well. The search terms were "COVID-19", "SARS-CoV-2", "coronavirus" and "urology". Finally, a narrative synthesis of the data obtained and the creation of a prioritization strategy for urological pathology for the expected de-escalating phases were carried out.
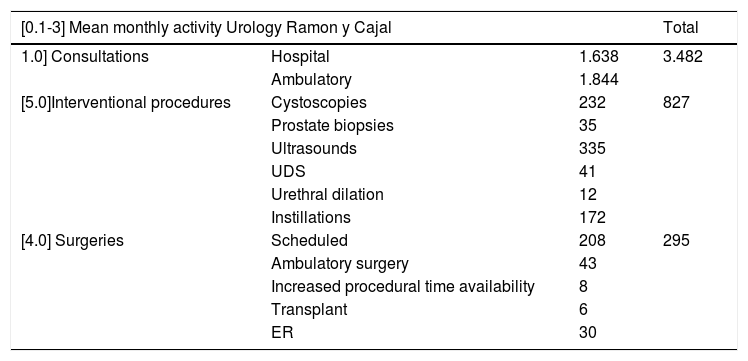
ResultsPhase 1: suspension of urological activityThe first phase of the pandemic spread caused the admission of hundreds of patients with COVID-19 infection, who rapidly occupied a large part of the hospital until it was overcrowded with an occupation of 130%. This forced the progressive suspension of the hospital's surgical activity in just a few days until it was almost completely cancelled, with the aim of obtaining sufficient ventilators and qualified spaces to support critical patients. Table 1 details the data on the activity of the department in the previous year, extracted from the institution's annual report, which is largely comparable to other high-volume hospitals in the Community of Madrid. This means that, in this initial 4-week period, an average of 295 surgeries have been suspended, represented by the following averages by specific procedures: 32.4 transurethral resections (TUR) of the bladder, 10.8 radical prostatectomies, 6.7 kidney transplants, 6.3 radical or partial nephrectomies and 4.6 radical cystectomies.
Mean monthly activity in the urology service of the Hospital Universitario Ramón y Cajal according to the different care units.
| [0.1-3] Mean monthly activity Urology Ramon y Cajal | Total | ||
|---|---|---|---|
| 1.0] Consultations | Hospital | 1.638 | 3.482 |
| Ambulatory | 1.844 | ||
| [5.0]Interventional procedures | Cystoscopies | 232 | 827 |
| Prostate biopsies | 35 | ||
| Ultrasounds | 335 | ||
| UDS | 41 | ||
| Urethral dilation | 12 | ||
| Instillations | 172 | ||
| [4.0] Surgeries | Scheduled | 208 | 295 |
| Ambulatory surgery | 43 | ||
| Increased procedural time availability | 8 | ||
| Transplant | 6 | ||
| ER | 30 | ||
Extracted from the annual report of service activity and calculation of the monthly average divided by the 12 months of the year.
UDS: urodynamic study.
Furthermore, as shown by the experience gained in these difficult weeks, and in line with what has recently been published by Chinese colleagues, mortality from COVID-19 of asymptomatic carriers or patients in the incubation phase who undergo elective surgery can reach 20.5%.15 These worrying figures also strongly justify such a drastic suspension of scheduled surgery during the initial phase of the pandemic spread.
As for the hospital's outpatient activity, a total of 3482 face-to-face consultations (Table 1) were suspended and mostly replaced by teleconsultations,16 using them to select those patients who inexorably required in-person consultation. And with regard to the 827 interventional procedures, through teleconsultation and using the institution's electronic history, those patients with tests that were hard to delay were selected, which basically were: long-term or infected ureteral stent removal, cystoscopies of suspected bladder cancer, high-risk bladder tumor controls and intravesical instillations in high-risk tumors. Given the presence of SARS-CoV-2 PCR in feces and its absence in urine to date,13 all prostate biopsies were suspended, and certain urethral dilation procedures were maintained.
Phase 2: incorporation of urologists into COVID care groupsHealthcare personnel can never be indifferent to pandemics, not only in terms of their jobs, even more so, in the purely personal sphere, as it is a sector that is particularly vulnerable due to its high exposure. A key element that should be controlled and anticipated is the shortage of personnel during these health crises, which can lead to high rates of absenteeism.17 Thus, with the hospital overloaded with 130% bed occupation, more than 300 doctors on medical leave and the complete suspension of all non-urgent surgical activity, almost half of the urology department staff, including some of the residents, joined the "Macro-COVID" group coordinated by the hospital's medical services. The department of urology, which has 42 beds, increased its capacity by 157% to a total of 66, all of which are dedicated to COVID-19 patients and are coordinated jointly with the infectious diseases and pneumology divisions.
With respect to urologic emergencies, the specialty's staff was reinforced to take care of urological pathology in the first instance. Urgent surgical activity was drastically reduced, from an average of 33 surgeries last year to only 8 in this year, always adjusting the indication in each case and balancing the risk-benefit of each intervention in a high incidence COVID-19 hospital, given the high mortality risk observed in surgical patients infected in the perioperative period.
In the event that the patient requiring urological surgery is suspected or COVID-19 confirmed, he or she should be operated in a specific operating room dedicated to this patient profile, with a negative pressure environment, separated access circuits from the other operating rooms and a respirator used exclusively for these cases.18,19 If such operating rooms are not available, post-operative disinfection protocols must follow the recommendations of each hospital's disease prevention and control department. Finally, the access and stay of personnel in the operating room must be strictly minimized, limited to surgeons, anesthesiologists and nurses.
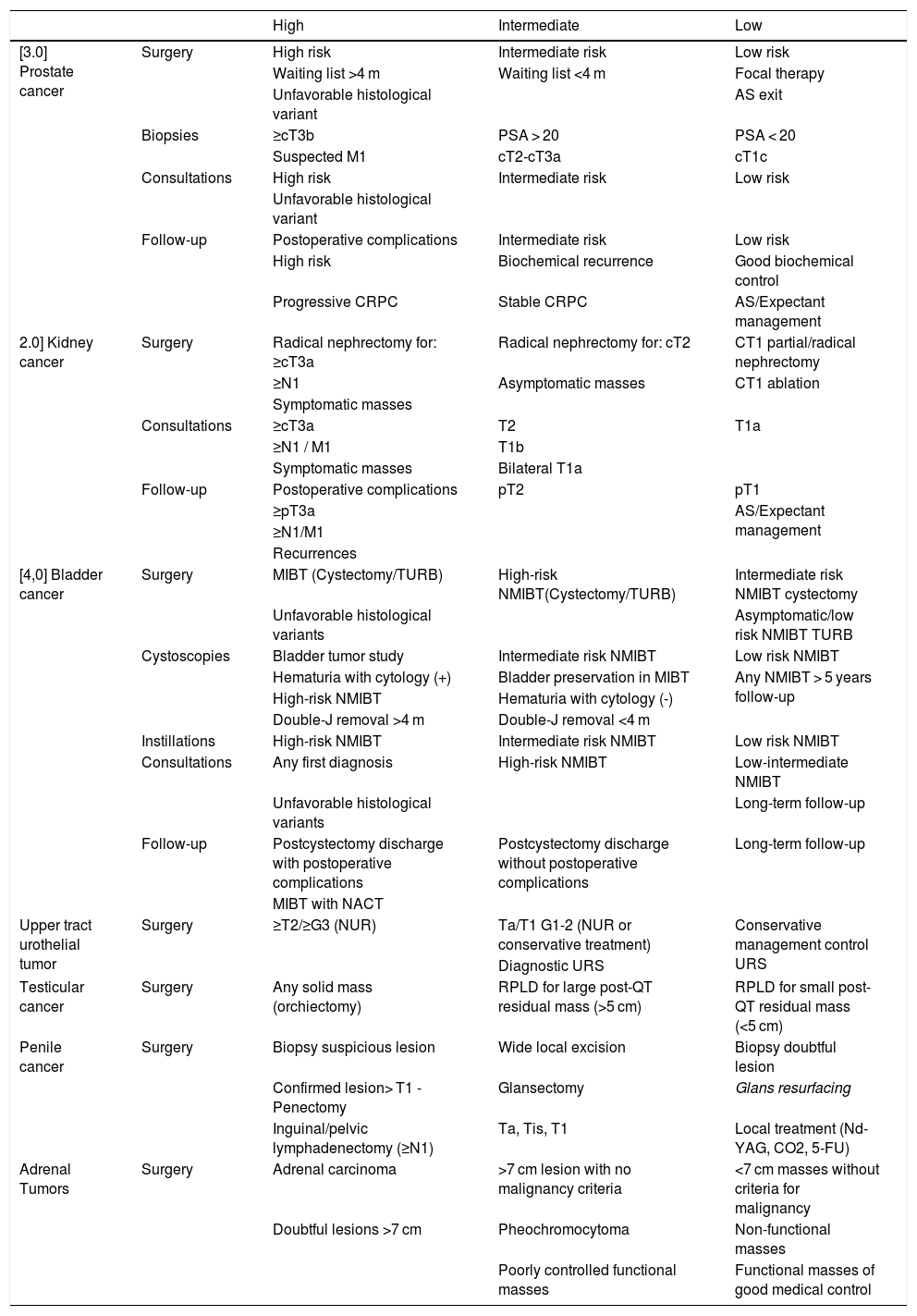
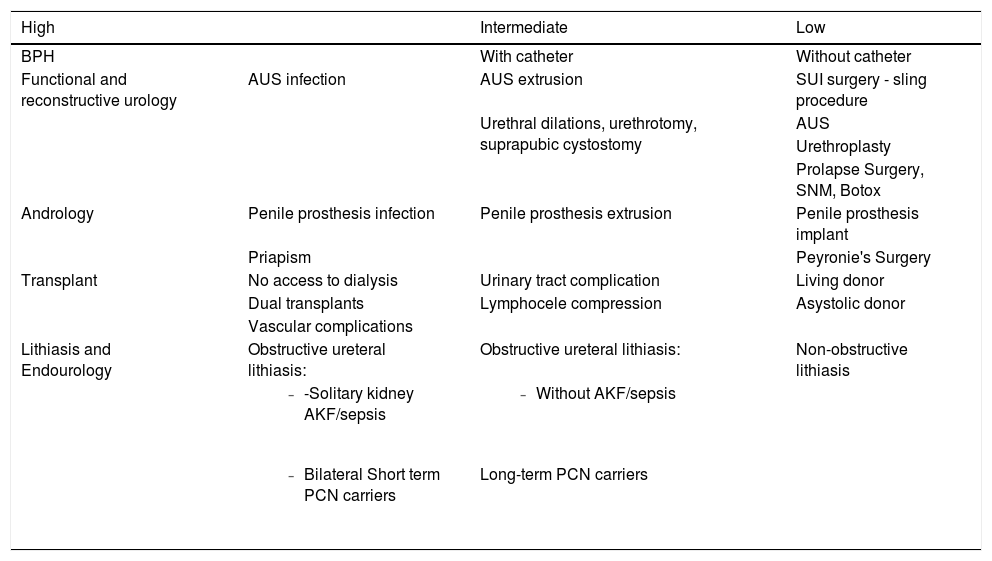
Phase 3: de-escalating and restoration of urological activityIf the initial phase of pandemic containment and department reorganization was not simple, it is likely to be followed by an even more convoluted phase. A decreased number of new infection cases is expected in the coming weeks, with the progressive availability of operating rooms and beds that will allow us to recover urological surgical activity in the hospitals of the Spanish health network. As has already been pointed out, the impact on the activity during the first 4 weeks of the pandemic has meant that our department has had to cancel approximately 295 surgeries, 3482 consultations and 827 interventional procedures, which will inevitably have to be reintroduced into the activity when it begins its recovery. To this end, it will be essential to prioritize urological pathology based on strictly clinical criteria, ignoring more than ever those non-medical causes that prioritize some procedures and paying special attention to the experience of colleagues from other countries who have faced this situation before ours.9,11,20 Although oncological pathology will prevail over benign pathology as a general rule, there are some caveats worth considering. To do so, we humbly propose a prioritization strategy of pathologies which synthetized in a visual and practical way in Tables 2 and 3. This proposal serves strictly clinical reasons and, in our opinion, can be helpful to all colleagues in decision-making processes under similar circumstances. These decisions should always be personalized, based on each patient's situation and on the availability and particularities of each institution. In no case shall these recommendations be considered as dogmas or rigid principles, and they should be subject to the healthy medical debate that undoubtedly enriches care.
Proposal for prioritization of uro-oncological pathology for the de-escalating and recovery phase.
| High | Intermediate | Low | ||
|---|---|---|---|---|
| [3.0] Prostate cancer | Surgery | High risk | Intermediate risk | Low risk |
| Waiting list >4 m | Waiting list <4 m | Focal therapy | ||
| Unfavorable histological variant | AS exit | |||
| Biopsies | ≥cT3b | PSA > 20 | PSA < 20 | |
| Suspected M1 | cT2-cT3a | cT1c | ||
| Consultations | High risk | Intermediate risk | Low risk | |
| Unfavorable histological variant | ||||
| Follow-up | Postoperative complications | Intermediate risk | Low risk | |
| High risk | Biochemical recurrence | Good biochemical control | ||
| Progressive CRPC | Stable CRPC | AS/Expectant management | ||
| 2.0] Kidney cancer | Surgery | Radical nephrectomy for: ≥cT3a | Radical nephrectomy for: cT2 | CT1 partial/radical nephrectomy |
| ≥N1 | Asymptomatic masses | CT1 ablation | ||
| Symptomatic masses | ||||
| Consultations | ≥cT3a | T2 | T1a | |
| ≥N1 / M1 | T1b | |||
| Symptomatic masses | Bilateral T1a | |||
| Follow-up | Postoperative complications | pT2 | pT1 | |
| ≥pT3a | AS/Expectant management | |||
| ≥N1/M1 | ||||
| Recurrences | ||||
| [4,0] Bladder cancer | Surgery | MIBT (Cystectomy/TURB) | High-risk NMIBT(Cystectomy/TURB) | Intermediate risk NMIBT cystectomy |
| Unfavorable histological variants | Asymptomatic/low risk NMIBT TURB | |||
| Cystoscopies | Bladder tumor study | Intermediate risk NMIBT | Low risk NMIBT | |
| Hematuria with cytology (+) | Bladder preservation in MIBT | Any NMIBT > 5 years follow-up | ||
| High-risk NMIBT | Hematuria with cytology (-) | |||
| Double-J removal >4 m | Double-J removal <4 m | |||
| Instillations | High-risk NMIBT | Intermediate risk NMIBT | Low risk NMIBT | |
| Consultations | Any first diagnosis | High-risk NMIBT | Low-intermediate NMIBT | |
| Unfavorable histological variants | Long-term follow-up | |||
| Follow-up | Postcystectomy discharge with postoperative complications | Postcystectomy discharge without postoperative complications | Long-term follow-up | |
| MIBT with NACT | ||||
| Upper tract urothelial tumor | Surgery | ≥T2/≥G3 (NUR) | Ta/T1 G1-2 (NUR or conservative treatment) | Conservative management control URS |
| Diagnostic URS | ||||
| Testicular cancer | Surgery | Any solid mass (orchiectomy) | RPLD for large post-QT residual mass (>5 cm) | RPLD for small post-QT residual mass (<5 cm) |
| Penile cancer | Surgery | Biopsy suspicious lesion | Wide local excision | Biopsy doubtful lesion |
| Confirmed lesion> T1 - Penectomy | Glansectomy | Glans resurfacing | ||
| Inguinal/pelvic lymphadenectomy (≥N1) | Ta, Tis, T1 | Local treatment (Nd-YAG, CO2, 5-FU) | ||
| Adrenal Tumors | Surgery | Adrenal carcinoma | >7 cm lesion with no malignancy criteria | <7 cm masses without criteria for malignancy |
| Doubtful lesions >7 cm | Pheochromocytoma | Non-functional masses | ||
| Poorly controlled functional masses | Functional masses of good medical control |
CRPC: castration-resistant prostate cancer; RPLD: retroperitoneal lymphadenectomy; PSA: prostate-specific antigen; CT: chemotherapy; TUR: transurethral resection of the bladder; NMIBT: non-muscle-invasive bladder tumor; MIBT: muscle-invasive bladder tumor; URS: ureterorenoscopy; AS: active surveillance.
Proposed prioritization of benign urological pathology for the de-escalating and recovery phase.
| High | Intermediate | Low | |
|---|---|---|---|
| BPH | With catheter | Without catheter | |
| Functional and reconstructive urology | AUS infection | AUS extrusion | SUI surgery - sling procedure |
| Urethral dilations, urethrotomy, suprapubic cystostomy | AUS | ||
| Urethroplasty | |||
| Prolapse Surgery, SNM, Botox | |||
| Andrology | Penile prosthesis infection | Penile prosthesis extrusion | Penile prosthesis implant |
| Priapism | Peyronie's Surgery | ||
| Transplant | No access to dialysis | Urinary tract complication | Living donor |
| Dual transplants | Lymphocele compression | Asystolic donor | |
| Vascular complications | |||
| Lithiasis and Endourology | Obstructive ureteral lithiasis: | Obstructive ureteral lithiasis: | Non-obstructive lithiasis |
|
| ||
| Long-term PCN carriers |
AUS: artificial urinary sphincter; AKF: acute kidney failure; BPH: benign prostatic hyperplasia; SUI: stress urinary incontinence; SNM: sacral neuromodulation; PCN: percutaneous nephrostomy.
The necessary personalization of each clinical case must take into account the general condition of the patients, their urological process as well as their actual condition, the risk-benefit relation of the treatment against a possible infection and the existence of possible alternative treatment options that temporarily offer a parenthesis until better and less risky sanitary conditions. In this sense, some clinical scenarios that can be considered are:
- •
Uro-oncology: in patients with high or very high-risk prostate cancer scheduled for surgery within a multimodal treatment, consider the option of three-month neoadjuvant androgen deprivation therapy. In patients with advanced uro-oncological diseases that will require chemotherapy, it is recommended not to initiate it at the slightest suspicion of COVID-19 or risk exposure and delay it for a few weeks.21,22
- •
Lithiasis: in addition to the classification shown in the table, individual measures should be considered such as antibiotic prophylaxis in patients with long-term catheterization, in patients expected to be long-term carriers or in those with a history of severe urological sepsis, in order to avoid potential new episodes of sepsis requiring ICU admission and whose mortality may reach 10%,23 given the known scarcity of this resource and the unfavorable epidemiological environment full of COVID-19 patients.
- •
Renal transplants: both the condition of immunosuppressed renal transplant recipients and the deleterious effect caused by it,24,25 as well as the ICU stay of deceased donors and the healthy condition of living donors have practically paralyzed transplant activity nationwide, with an average drop in weekly donations from 8.3 to 0.7 and transplants from 17.6 to 1.4.26 Priority should be given to those patients awaiting dual transplants with urgent need for the organ accompanying the kidney (hepatorenal or cardiorenal), as well as to the rare cases where access to dialysis is not possible.
Last but not least, the COVID-19 pandemic has also had a major impact on postgraduate residency training programs (MIR). This crisis has led to a drastic decrease in the training activities of urology residents in all areas of training (shifts, diagnostic procedures, endoscopic, open and mini invasive surgery), being more evident for residents in their final year.27 However, since the beginning of this health crisis in Spain, many of the residents from different specialties including urology, assumed their inescapable responsibility as doctors, prioritizing their duty to face a terrible pandemic that collapses the health system and paralyzes a country, representing the best example of doctor commitment to a society that will face the brutal effect of tens of thousands of deaths in only a few weeks. During this complicated period, 50% of urology residents in our center became part of the hospital's "Macro COVID" group, compared to only 7% of urology residents in Italy.27 However, it is not easy to know if this sacrifice of their valuable training time will be recovered, in view of the government measure to extend their residency contract sine die.28 Restoring their training and time lost will also be a challenge and a duty for everyone in this de-escalation phase that seems to be starting in the near future. The correct use of technology tools such as telemedicine, videoconferencing, surgical simulators, recorded surgical videos, online teaching, webinars, social networks or robotic platforms10 could help compensate for their admirable effort and responsibility in these difficult times.
ConclusionsThe pandemic caused by SARS-CoV-2 has collapsed the health system in the Community of Madrid and fully impacted all hospital activity, including that of the urology service. The practical suspension of all urological activity during the first 4 weeks has meant the cancellation of a large number of surgeries, consultations and interventional procedures in our department. The prioritization of the pathology of suspended patients based on clinical criteria will be crucial when dealing with the necessary reestablishment of this activity. The suspension in the resident training programs must be recovered with the use of technology tools which can play not only a temporary role, but perhaps a definitive one.
Conflicts of interestThe authors declare that they have no conflicts of interest.
This work is dedicated to the memory of all the victims of the pandemic and their families, especially that of José Alcaraz Ortega.
Please cite this article as: Silva D, Mendes P, Mourato C, Martins D, Mendes F, Cruz R. et al. Pandemia COVID-19: impacto y reacción rápida de la Urología. Actas Urol Esp. 2020;44:450–457.