Virtually all kidney transplantation (KT) Centers worldwide have been forced to rapidly adapt to the challenges raised by the COVID-19 pandemic.1 Notably, KT recipients diagnosed with COVID-19 have experienced adverse clinical outcomes,2,3 posing concerns on the safety of KT during this period. As such, the number of donations and KTs from deceased donors has suffered a critical reduction in several Countries.4
In this scenario, while KT programs from living donors have been suspended at most Centers (including ours), whether KT programs from deceased donors should be continued during such an emergency scenario is still matter of debate.5 Moreover, there is still lack of data on the rate of COVID-19 after KT, as well as on the safety of minimally-invasive surgery in this setting. Yet, being KT from deceased donors a highly valuable “urgent” surgical procedure, maintaining this activity even during emergency scenarios is paramount.
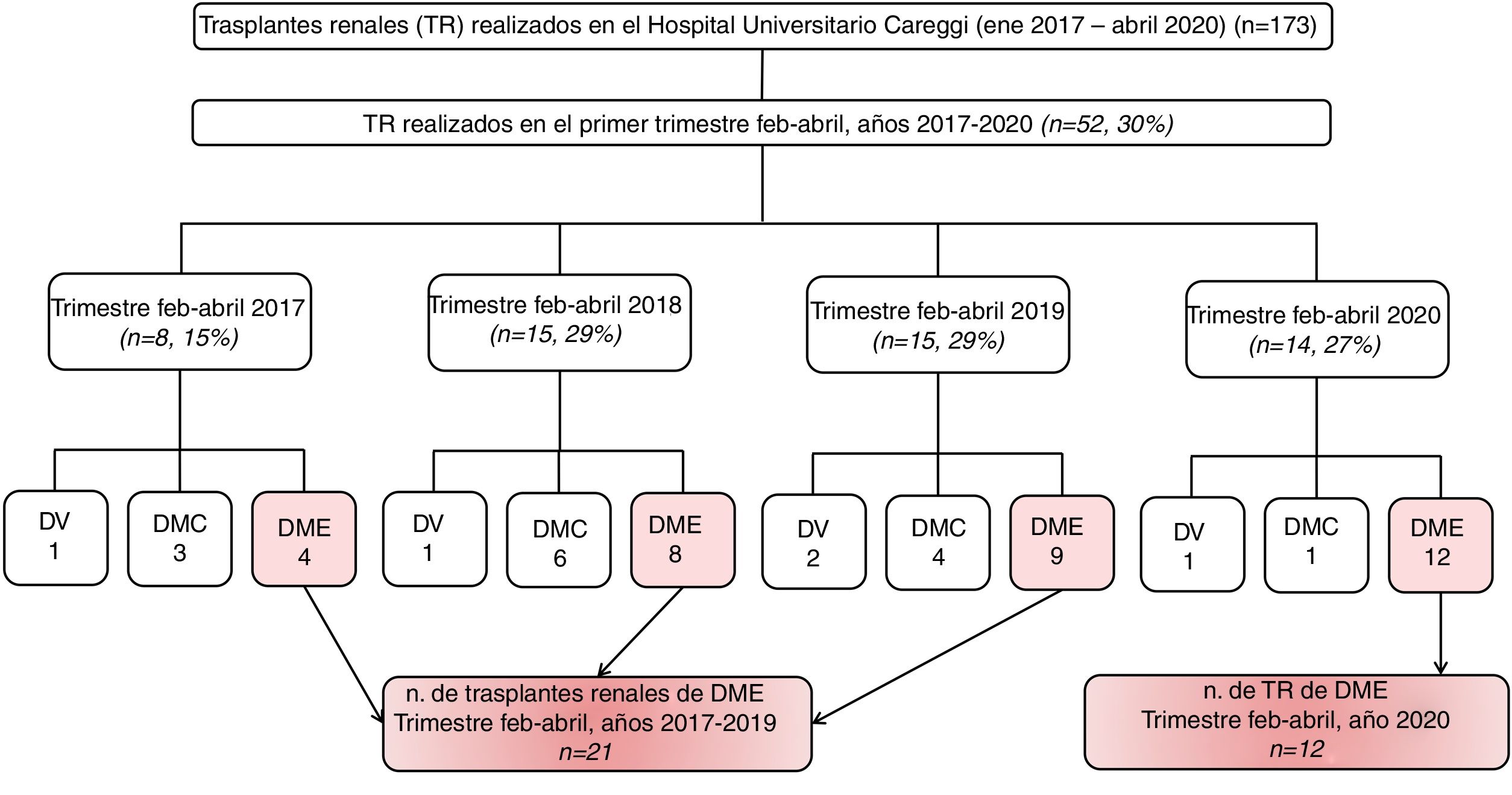
To provide insights in this regard, herein we report our experience of KT from donors after brain death (DBD) during the trimester February-April 2020 (COVID-19 period), comparing its outcomes with those of KT performed in the same timeframe in the years 2017–2019 (no-COVID period) (Fig. 1).
Flowchart showing the number of kidney transplantations (KT) performed at Careggi University Hospital in the period Jan 2017–Apr 2020 (n=173) and of KTs from donors after brain death (DBD) in the Trimester Feb-Apr of the year 2020 (n=12, COVID period) vs. the years 2017–2019 (n=21, no-COVID period), representing the analytic cohort. LD=living donor; DBD=donors after brain death; DCD=donors after circulatory death; KT=kidney transplantation.
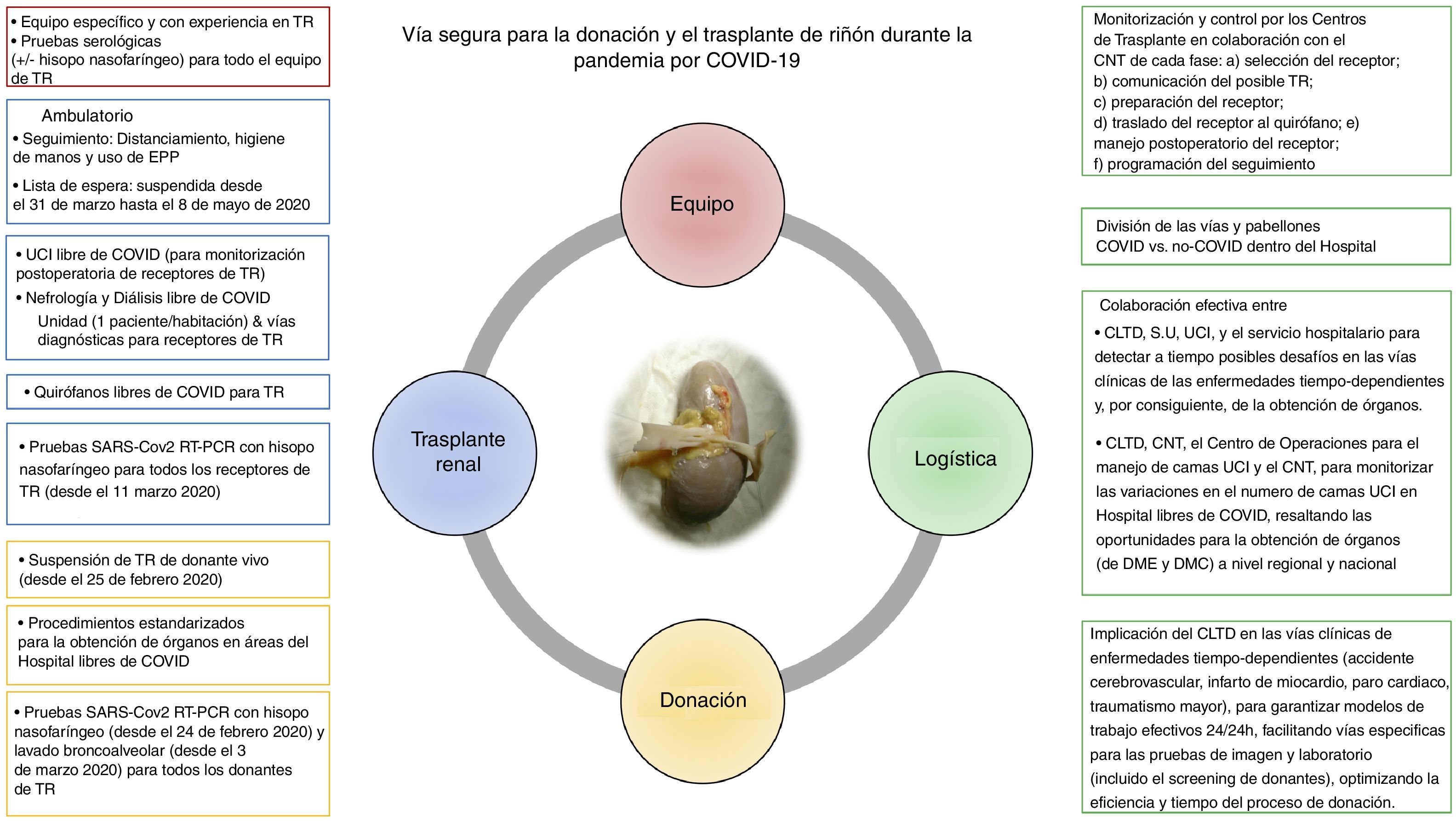
At our Center, located in one of the Italian Regions that have been hit the most by COVID-19, a series of logistical and clinical measures were implemented early after the spread of the epidemic aiming to prevent transmission of the disease to KT recipients (Fig. 2).
Overview of the pathway for donation and kidney transplantation at Careggi University Hospital in Florence, Italy, during the COVID-19 pandemic. The first priority of such dedicated pathways was to ensure the safety of kidney transplantation recipients, reducing the risk of donor-derived COVID-19. A&E=Accident & Emergency; CNT=Centro Nazionale Trapianti (Italian Transplant Authority); DBD=donors after brain death; DCD=donors after circulatory death; LTDC=local transplant and donation coordinator; KT=kidney transplantation; ICU=intensive care unit; O.R.=operating room; PPE=personal protection equipment; RTC=Regional Transplant Center.
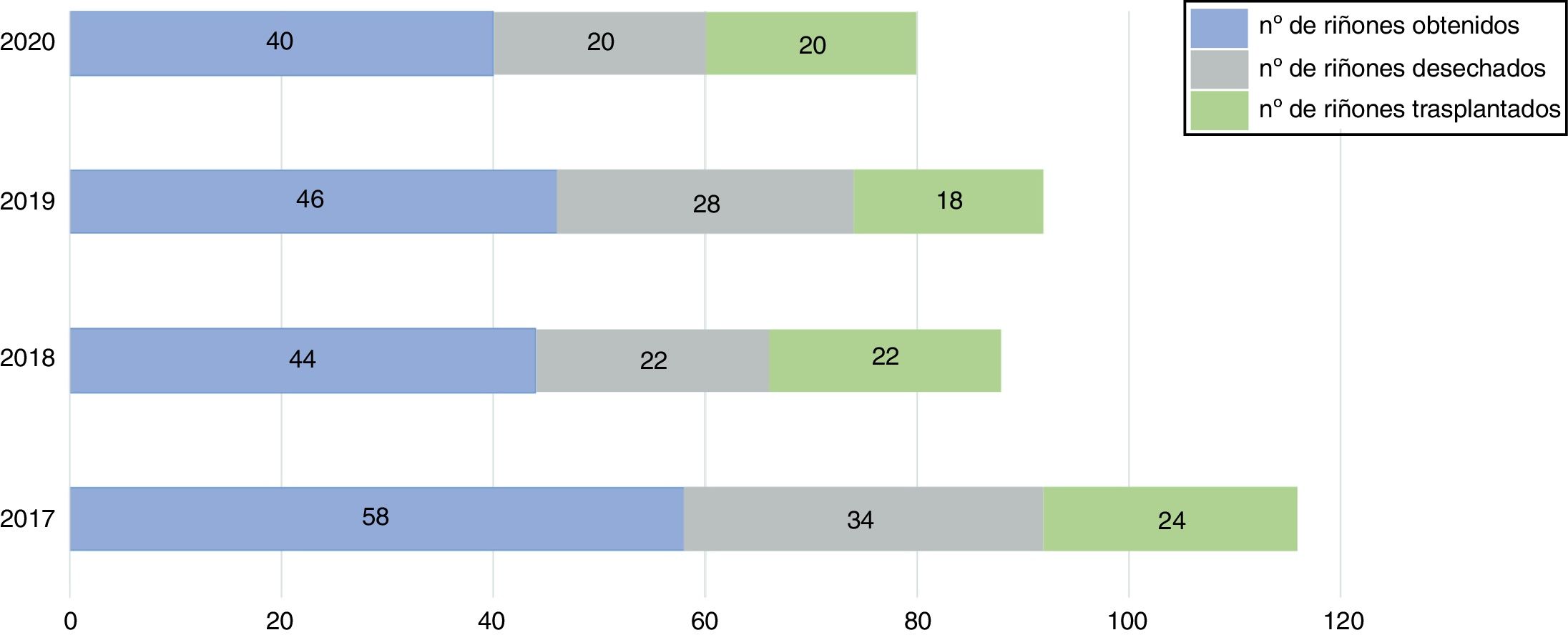
Overall, the kidney procurement and transplantation activities did not change significantly during the COVID-19 period (Fig. 3).
Overview of the kidney procurement activity at Careggi University Hospital (Trimester Feb–Apr, years 2017–2020). In the trimester Feb–Apr 2020 (COVID period), kidney procurement was performed by our local transplant team in the whole Florence area. In addition, in April we accepted for kidney transplantation 2 kidneys from another North-Italian Region that experienced severe logistical challenges in allocation of the graft in that period. Tuscany had officially declared that transplant activity should have been maintained active during the pandemic, being an “urgent procedure” (deliberation n. 572, May 4th 2020, Regional Council of Tuscany, available at: https://www.regione.toscana.it). In particular, transplant centers were asked to ensure the historical proportionality between offered organs (from both regional and extra regional procurement centers) and transplanted organs, respecting the safety principles released by the Regional Transplant Center and the Italian Transplant Authority.
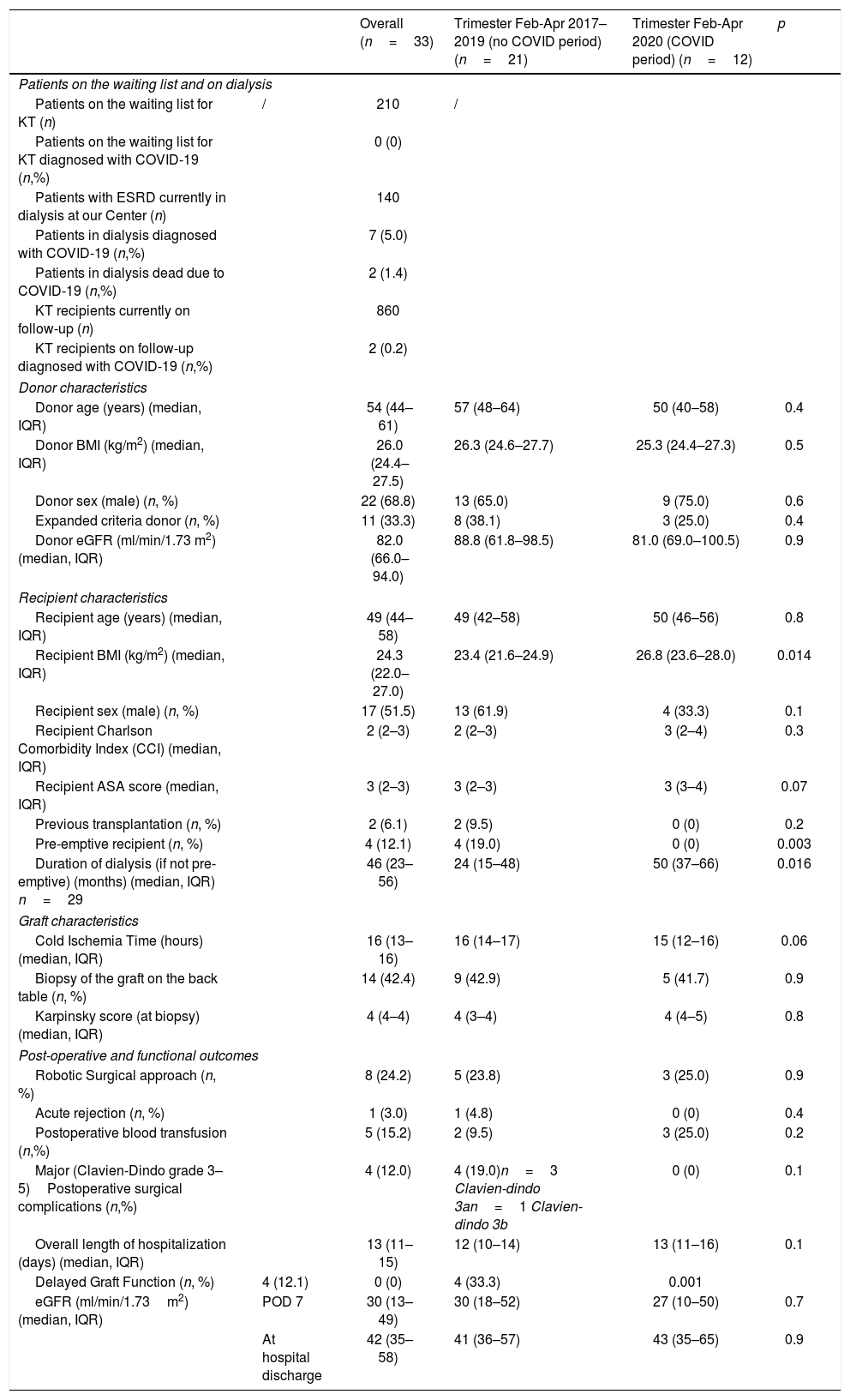
Thirty-three KTs were included in the analytic cohort (12 in COVID vs. 21 in the no-COVID period) (Table 1). While the donors’ profile was similar between the two groups, we observed that recipients in the trimester Feb-Apr 2020 were less frequently pre-emptive (0% vs. 19%, p=0.003) and had longer median dialysis periods before KT (50 vs. 24 months, p=0.016). The proportion of robotic KTs was similar in the two groups (23.8% vs. 25%). Moreover, cold ischemia time, as well as intra/post-operative outcomes and median length of hospitalization, did not differ between the two study periods. While a higher rate of delayed graft function was recorded in patients undergoing KT during the COVID-19 period, median estimated glomerular filtration rate (eGFR) at hospital discharge was similar between the study groups (43 vs. 41ml/min/1.73m2, p=0.9).
Characteristics related to donor, recipient and graft, and postoperative functional outcomes related to the patients included in our study.
| Overall (n=33) | Trimester Feb-Apr 2017–2019 (no COVID period) (n=21) | Trimester Feb-Apr 2020 (COVID period) (n=12) | p | ||
|---|---|---|---|---|---|
| Patients on the waiting list and on dialysis | |||||
| Patients on the waiting list for KT (n) | / | 210 | / | ||
| Patients on the waiting list for KT diagnosed with COVID-19 (n,%) | 0 (0) | ||||
| Patients with ESRD currently in dialysis at our Center (n) | 140 | ||||
| Patients in dialysis diagnosed with COVID-19 (n,%) | 7 (5.0) | ||||
| Patients in dialysis dead due to COVID-19 (n,%) | 2 (1.4) | ||||
| KT recipients currently on follow-up (n) | 860 | ||||
| KT recipients on follow-up diagnosed with COVID-19 (n,%) | 2 (0.2) | ||||
| Donor characteristics | |||||
| Donor age (years) (median, IQR) | 54 (44–61) | 57 (48–64) | 50 (40–58) | 0.4 | |
| Donor BMI (kg/m2) (median, IQR) | 26.0 (24.4–27.5) | 26.3 (24.6–27.7) | 25.3 (24.4–27.3) | 0.5 | |
| Donor sex (male) (n, %) | 22 (68.8) | 13 (65.0) | 9 (75.0) | 0.6 | |
| Expanded criteria donor (n, %) | 11 (33.3) | 8 (38.1) | 3 (25.0) | 0.4 | |
| Donor eGFR (ml/min/1.73 m2) (median, IQR) | 82.0 (66.0–94.0) | 88.8 (61.8–98.5) | 81.0 (69.0–100.5) | 0.9 | |
| Recipient characteristics | |||||
| Recipient age (years) (median, IQR) | 49 (44–58) | 49 (42–58) | 50 (46–56) | 0.8 | |
| Recipient BMI (kg/m2) (median, IQR) | 24.3 (22.0–27.0) | 23.4 (21.6–24.9) | 26.8 (23.6–28.0) | 0.014 | |
| Recipient sex (male) (n, %) | 17 (51.5) | 13 (61.9) | 4 (33.3) | 0.1 | |
| Recipient Charlson Comorbidity Index (CCI) (median, IQR) | 2 (2–3) | 2 (2–3) | 3 (2–4) | 0.3 | |
| Recipient ASA score (median, IQR) | 3 (2–3) | 3 (2–3) | 3 (3–4) | 0.07 | |
| Previous transplantation (n, %) | 2 (6.1) | 2 (9.5) | 0 (0) | 0.2 | |
| Pre-emptive recipient (n, %) | 4 (12.1) | 4 (19.0) | 0 (0) | 0.003 | |
| Duration of dialysis (if not pre-emptive) (months) (median, IQR) n=29 | 46 (23–56) | 24 (15–48) | 50 (37–66) | 0.016 | |
| Graft characteristics | |||||
| Cold Ischemia Time (hours) (median, IQR) | 16 (13–16) | 16 (14–17) | 15 (12–16) | 0.06 | |
| Biopsy of the graft on the back table (n, %) | 14 (42.4) | 9 (42.9) | 5 (41.7) | 0.9 | |
| Karpinsky score (at biopsy) (median, IQR) | 4 (4–4) | 4 (3–4) | 4 (4–5) | 0.8 | |
| Post-operative and functional outcomes | |||||
| Robotic Surgical approach (n, %) | 8 (24.2) | 5 (23.8) | 3 (25.0) | 0.9 | |
| Acute rejection (n, %) | 1 (3.0) | 1 (4.8) | 0 (0) | 0.4 | |
| Postoperative blood transfusion (n,%) | 5 (15.2) | 2 (9.5) | 3 (25.0) | 0.2 | |
| Major (Clavien-Dindo grade 3–5)Postoperative surgical complications (n,%) | 4 (12.0) | 4 (19.0)n=3 Clavien-dindo 3an=1 Clavien-dindo 3b | 0 (0) | 0.1 | |
| Overall length of hospitalization (days) (median, IQR) | 13 (11–15) | 12 (10–14) | 13 (11–16) | 0.1 | |
| Delayed Graft Function (n, %) | 4 (12.1) | 0 (0) | 4 (33.3) | 0.001 | |
| eGFR (ml/min/1.73m2) (median, IQR) | POD 7 | 30 (13–49) | 30 (18–52) | 27 (10–50) | 0.7 |
| At hospital discharge | 42 (35–58) | 41 (36–57) | 43 (35–65) | 0.9 | |
None of the 12 recipients undergoing KT in 2020 was diagnosed with COVID-19 during the postoperative course, as none of the 210 patients currently in the waiting list for KT at our Center. At last, to date, we recorded 7 COVID-19 cases among the 140 patients in dialysis (with 2 disease-related deaths) and 2 cases among the 860 KT recipients in the outpatient setting.
Although the challenges caused by the COVID-19 pandemic may jeopardize the KT activity, our experience supports the feasibility and safety of KT from DBDs even during such emergency periods, provided both human and logistical resources allowing to achieve a timely and effective pathway for donation and transplantation.
Please cite this article as: Li Marzi V, Campi R, Pecoraro A, Peris A, Serni S. Viabilidad y seguridad del trasplante renal de donante fallecido durante la pandemia por COVID-19: perspectivas de un hospital universitario italiano. Actas Urol Esp. 2020;44:708–712.