This was the first study conducted to determine the influence of home-based treadmill training on seminal quality in adults with type 2 diabetes.
Materials and methodsSixty sedentary adults with type 2 diabetes volunteered for the current study. Thirty were randomly allocated to the intervention group and performed a 14-week, home-based, treadmill training program, 3 sessions per week, consisting of a warm-up (10–15min), 40min treadmill exercise at a work intensity of 55–70% of peak heart rate (increasing by 2.5% each two weeks) measured during a maximal treadmill test, and cooling-down (5–10min). The control group included the age of 30, and BMI matched adults with type 2 diabetes who did not take part in any training program. Seminal quality analysis included semen volume, sperm concentration, motility and normal morphologic features. Furthermore, total antioxidant status (TAS) and glutathione peroxidase (GPX) activity were assessed in seminal plasma. This protocol was approved by an Institutional Ethics Committee.
ResultsThe home-based treadmill training significantly increased sperm concentration as well as percentages of total sperm motility and normal spermatozoa. Furthermore, TAS and GPX activity were increased after the completion of the training program. No significant changes in any of the measured variables were found in the control group.
ConclusionsHome-based treadmill training improved seminal quality in adults with type 2 diabetes. A secondary finding was that seminal antioxidant defense system was significantly increased after being exercised.
El presente estudio se diseñó para determinar la influencia de un programa de entrenamiento domiciliario en la calidad seminal de adultos con diabetes tipo 2.
Material y métodoParticiparon un total de 60 adultos varones con diagnóstico de diabetes tipo 2 distribuidos aleatoriamente en un grupo intervención (n=30) y otro control (n=30). Los participantes incluidos en el grupo de intervención desarrollaron un programa de entrenamiento domiciliario en tapiz rodante de 14 semanas, 3 sesiones/semana de 40min a una intensidad del 55-70% FCmáx (incrementando un 2,5% cada 2 semanas). Los parámetros de calidad seminal ensayados fueron: volumen, concentración y porcentaje de movilidad y morfología normal. Asimismo se estudió el nivel de defensas antioxidantes en plasma seminal. Nuestro protocolo fue aprobado por un comité de ética institucional.
ResultadosTras completar el programa de entrenamiento se observó un incremento significativo de la concentración espermática, así como de los porcentajes de movilidad y de morfología normal. Paralelamente, se observó un incremento del estatus total antioxidante en el plasma seminal. No se observaron cambios significativos en ninguna de las variables ensayadas en el grupo control.
ConclusionesEl programa de entrenamiento mejoró la calidad seminal en pacientes con diabetes tipo 2. Este hallazgo podría explicarse por una mejora de las defensas antioxidantes seminales inducida por el ejercicio.
Previous studies have highlighted the prevalence of diabetes in a population of male partners of infertile couples.1 Echevarria-Sánchez et al.2 found that patients with type 2 diabetes mellitus (T2DM) exhibited a low sperm progressive mobility that might be associated to subfertility. In a more detailed way, the highest percentage of sperm DNA damage because of oxidative stress seen in T2DM patients may be responsible for the poor embryonic development and pregnancy outcome in these individuals.3 In fact, oxidative stress is widely recognized as one of the major causes of male subfertility/infertility both in experimental4 and human studies.5
Fortunately, de Oliveira et al.6 have already demonstrated that a 12-week training program provided important upregulation in antioxidant enzymes and increased nitric oxide bioavailability, which may help minimize oxidative stress and the development of the chronic complications of T2DM. Therefore, this was the first study conducted to determine whether home-based training may improve seminal quality in adults with T2DM. A secondary objective was to assess its influence on antioxidant defense system in seminal plasma.
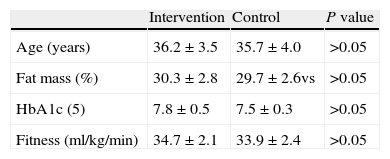
Materials and methodsParticipantsA total of sixty adults with T2DM were recruited from the community for the current study. The characteristics of the participants at baseline are summarized in Table 1. All the subjects met the following inclusion criteria: (1) young adults (25–40 years); (2) diagnosis of T2DM; (3) medical approval for physical activity participation. On the other hand, exclusion criteria were: (1) participation in a training program in the 6 months prior to their participation in the trial; (2) testicular varicocele, genital infection, and/or leukocytospermia; (3) previous surgery (e.g. vasectomy reversal, varicocele removal, etc.); (4) receiving medication and/or antioxidant consumption that may interfere with measured outcomes; (5) toxic habits (smoking and/or alcohol); (6) not completing at least 90% of the training sessions.
Anthropometric, biochemical and fitness status of adults with type 2 diabetes enrolled in the intervention and control groups at baseline.
| Intervention | Control | P value | |
| Age (years) | 36.2±3.5 | 35.7±4.0 | >0.05 |
| Fat mass (%) | 30.3±2.8 | 29.7±2.6vs | >0.05 |
| HbA1c (5) | 7.8±0.5 | 7.5±0.3 | >0.05 |
| Fitness (ml/kg/min) | 34.7±2.1 | 33.9±2.4 | >0.05 |
Note: Results expressed as mean±sd.
Participants were randomly allocated to the intervention (n=30) or control group (n=30) using a concealed method.
Home-based treadmill trainingParticipants in the intervention group performed a 14-week, home-based, treadmill training program, 3 sessions per week, consisting of a warm-up (10–15min), 40min treadmill exercise at a work intensity of 55–70% of peak heart rate (increasing by 2.5% every two weeks) measured during a maximal treadmill test, and cooling-down (5–10min). In order to ensure that the training workload was appropriate, all the participants from the intervention group wore a wireless wearable heart rate monitor (Sport Tester PE3000, Polar Electro, Kempele, Finland). Lastly, the control group included the age of 30, and the BMI matched adults with type 2 diabetes who did not take part in any training program.
Semen quality assessmentSemen was collected after 3 days of sexual abstinence (intercourse or masturbation) by manual masturbation into a sterile container on site and examined within 30min of ejaculation. Seminal assessment included semen volume (ml), sperm concentration (%), sperm motility (%), and normal morphologic features (%). All parameters were carried out according to the World Health Organization (WHO) guidelines.7 It should be pointed out that sperm concentration was determined by hemacytometer (Hauser Scientific Inc., Horsham, PA) whereas motility was assessed by a computer-aided semen analysis (CASA system, Microptic S.L., Spain).
A fraction of each semen sample was used to determine antioxidants and lipoperoxidation levels. Seminal plasma was obtained after centrifugation at 3500rpm for 15minutes and it was loaded in the Eppendorf tubes (3ml) and stored at −80°C until analysis.
Total antioxidant status (TAS) in seminal plasma was determined by colorimetric method using Randox commercial kits on the Hitachi 902 Autoanalyzer. Total SOD activity was determined using pyrogallol as a substrate by the method of Marklund and Marklund.8 One Unit (U) of total SOD and CuZnSOD is defined as the amount of enzyme required to inhibit the rate of pyrogallol auto-oxidation by 50%.
GPX activity was assayed by the subsequent oxidation of NADPH at 240nm with t-butyl-hydro-peroxide as a substrate 21. GPX units (U/g protein) were defined as μmol NADPH oxidized/g protein.9
Physical fitnessParticipants performed a continuous maximal incremental test, using the standard Bruce treadmill protocol, until exhaustion in the laboratory of Sports Medicine. Gas exchange data were collected throughout the test using a breath-by-breath metabolic system. The EKG was continuously recorded using a 12 lead stress analysis system. In this respect, the criterion we used to determine the VO2 max was the maximal O2 value at plateau despite increasing workload (<2ml/kg/min increase in VO2 between progressive stages). Furthermore, it should be pointed out that all participants underwent a pre-training period in the laboratory to be familiarized with the correct use of the treadmill.
Body compositionFat mass percentage was assessed by bioelectrical impedance analysis BIA (MC-180, Tanita Ltd., UK). Participants were requested not to perform moderate or vigorous exercise for 24h prior to testing as well as to abstain from eating or drinking for two hours before testing. Moreover, they were asked to urinate immediately prior to data collection.
Nutritional intake recordTo control the potential confounding effect of diet, participants included in intervention and control groups recorded their nutritional intake for 3 consecutive days (2 weekdays and 1 weekend day). It should be pointed out that participants were instructed about completion of the nutritional protocol. No significant difference was found between the intervention and control groups when assessing mean daily vitamin intake both at baseline (10.4±2.6 vs. 9.8±2.2mg/d vitamin E p=0.411; 83.8±20.4 vs. 80.8±19.7mg/d vitamin C p=0.620) and at the end of the intervention program (10.8±2.5 vs. 10.2±2.0mg/d vitamin E p=0.716; 85.5±21.6 vs. 82.9±20.9mg/d vitamin C p=0.328).
Ethics and statisticsThis research has been conducted in full accordance with ethical principles, including the World Medical Association Declaration of Helsinki (version, 2002). Participants gave their written informed consent prior to study participation. Furthermore, this protocol was approved by an Institutional Ethics Committee.
The results were expressed as a mean (SD). Given the limited sample size, the Shapiro–Wilk test was used to assess whether the data were normally distributed. To compare the mean values, repeated one-way analysis of variance (ANOVA), with post hoc Bonferroni correction to account for multiple tests, were used. Lastly, Pearson's correlation coefficient (r) was used to determine potential associations among tested parameters. The significance of the changes observed was ascertained to be p<0.05.
ResultsThe home-based treadmill training significantly increased VO2 max (34.7±2.1 vs. 38.2±1.9ml/kg/min; p=0.018; d=0.71) suggesting an improvement of physical fitness. Similarly, it significantly reduced fat mass percentage (30.3±2.8 vs. 29.8±2.4%; p=0.0376; d=0.64).
Regarding seminal quality analysis, sperm concentration (p=0.029; d=0.61) and the percentages of total sperm motility (p=0.006; d=1.21) and normal spermatozoa (p=0.018; d=1.10) were significantly improved in the intervention group. These results are listed in Table 2. Furthermore, after the completion of the training program, seminal TAS (p=0.024; d=0.90) and GPX activity (p=0.012; d=1.08) were significantly increased. These results are summarized in Table 3.
Characteristics of the standard seminal fluid evaluation in adults with type 2 diabetes allocated in the intervention and the control group.
| Intervention group | Control group | Cohen's d | |||
| Pre-test | Post-test | Baseline | Final | ||
| Volume | 2.96±0.82 | 3.08±0.86 | 2.90±0.86 | 2.92±0.90 | 0.18 |
| Count | 58.6±5.9 | 62.2±6.3a,b | 57.9±6.3 | 58.2±6.5 | 0.61 |
| Motility | 57.1±5.4 | 63.5±5.8a,b | 56.0±5.7 | 56.3±6.0 | 1.21 |
| Morphology | 46.1±4.6 | 51.2±5.0a,b | 45.8±4.9 | 45.9±4.8 | 1.10 |
Note: Results expressed as mean±sd. Volume: semen volume expressed as ml; Count: Sperm concentration expressed as 106ml−1; sperm motility and normal morphology expressed as percentage (%).
Effects of home-based treadmill training on seminal antioxidant defense system in adults with type 2 diabetes.
| Exercising group | Control group | Cohen's d | |||
| Pre-test | Post-test | Baseline | Final | ||
| TAS | 1.41±0.53 | 1.89±0.46 a,b | 1.32±0.58 | 1.36±0.60 | 0.90 |
| GPX | 4.77±1.66 | 6.23±1.50 a,b | 4.58±1.49 | 4.61±1.55 | 1.08 |
Note: TAS, total antioxidant status expressed as mmol/l; GPX, glutathione peroxidase expressed as 10−3U/g protein.
Lastly, significant correlations were found between seminal antioxidant defenses and seminal quality parameters. In this respect, a positive significant correlation was found between TAS and percentages of sperm motility (r=0.040; p=0.0292) and normal morphology (r=0.037; p=0.0354).
On the other hand, no significant changes in any of the measured variables were found in the control group (Table 2). Furthermore, it should be also pointed out that neither sports-related injuries nor withdrawals from the program were reported during the entire study period.
DiscussionAs was hypothesized, treadmill training improved seminal quality in sedentary adults with T2DM. Similarly, Gaskins et al.10 demonstrated that higher moderate-to-vigorous activity and less TV watching were significantly associated with higher total sperm count and sperm concentration in young healthy men. However, it should be pointed out when designing a training protocol that depending on sport modality and/or intensity, physical activity may impact negatively on sperm quality. In this respect, bicycling ≥5h/wk was associated with lower sperm concentration and motility.11 Similarly, long-term strenuous treadmill exercises (80%VO2 max) have a deleterious effect on reproduction.12
Accumulated evidence indicates that oxidative stress can be a primary cause of male subfertility/infertility.13 In this line, another striking feature of the present study was that treadmill training significantly increased seminal TAS, by a significant improvement of GPX activity. Consistent with previous studies,14 our results also suggested that seminal plasma TAS had a significant positive correlation with percentages of sperm motility and normal morphology.
Regarding body composition, Bener et al.15 reported that patients having a BMI >30 were found to have a three-fold increased risk of infertility. Accordingly, it was important to note that the current treadmill training improved body composition by reducing fat mass percentage in patients with T2DM. This is of particular interest given that Goulis and Tarlatzis16 found the excess adipose tissue resulted in increased conversion of testosterone to estradiol, which may finally impair testicular function.
The current study has some limitations that should be considered. The small sample size may limit the generalization of the results. Furthermore, sexual hormone evaluations were not included. Another major weakness was the relatively short duration of the exercise intervention in that there was no follow-up to determine whether the positive effects induced by treadmill training were maintained. Therefore, there is a clear need for long-term studies to determine whether correction of seminal quality improves the outcomes of live birth and pregnancy rate in this group.
On the other hand, regarding the strengths of the present trail, the excellent adherence rate suggested that the training program was effective and easy to follow-up. This was of particular interest given that it may finally give them the confidence to continue exercising after the trial finishes. In fact, several authors have recommended home-based exercise programs to maintain the beneficial effects obtained during previous supervised training programs.17
In conclusion, a 14-week home-based treadmill training improved seminal quality in young adults with T2DM. A secondary finding was that the seminal antioxidant defense system significantly increased after being exercised.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Rosety-Rodriguez M, Rosety JM, Fornieles G, Rosety MA, Diaz AJ, Rosety I, et al. El entrenamiento en tapiz rodante a domicilio mejora la calidad seminal en adultos con diabetes de tipo 2. Actas Urol Esp. 2014;38:589–593.