The suspension of most elective surgeries during COVID-19 pandemic caused the lengthening of urology surgical waiting lists. The objective of this study is to evaluate the impact of COVID-19 pandemic on urology surgical waiting list in a high-volume hospital.
MethodsAn observational descriptive study was designed. All patients included in the urology surgical waiting list of our high-volume center on May 1st 2020 (46 days after the suspension of elective surgery) were analyzed. Baseline variables, priority on the waiting list, main urological disease, type of scheduled surgery, and waiting time were recorded. Other variables recorded were the presence of a urinary catheter, number of accesses to the emergency department, evidence of COVID-19 infection, number of deaths and their cause. The waiting time for each disease was compared with the time to surgery in 2019.
ResultsA total of 350 patients were included. The mean (SD) time on the waiting list was 97.33 (55.47) days. Priority 1 patients, who normally should undergo surgery within 30 days, were on the waiting list for a mean (SD) time of 60.51 (20.14) days. They were mainly patients with ureteral lithiasis (25.6%), high-risk or muscle-invasive bladder cancer (20.9%) and high-risk prostate cancer (13.9%). The mean waiting time had already significantly exceeded the mean time to surgery in 2019 for radical cystectomy (p = 0.04) and URS (p = 0.003).
ConclusionsThe suspension of most elective surgeries due to COVID-19 had a significant impact on urology surgical waiting list of our high-volume center, especially in priority 1 group.
La suspensión de la mayoría de las cirugías electivas durante la pandemia por COVID-19 ha aumentado las listas de espera de cirugía urológica. El objetivo de este estudio es evaluar el impacto de la pandemia COVID-19 en la lista de espera de cirugía urológica en un hospital de alto volumen.
MétodosSe diseñó un estudio descriptivo observacional. Se analizaron todos los pacientes incluidos en la lista de espera de cirugía urológica de nuestro centro de alto volumen el 1 de mayo de 2020 (46 días después de la suspensión de la cirugía electiva). Se registraron las características basales, prioridad en la lista de espera, enfermedad urológica principal, tipo de cirugía programada y tiempo de espera. Otras variables registradas fueron la presencia de catéter urinario, el número de visitas al servicio de urgencias, evidencia de infección por COVID-19, el número de muertes y su causa. El tiempo de espera de cada enfermedad se comparó con el tiempo de espera para la cirugía en 2019.
ResultadosUn total de 350 pacientes fueron incluidos en el estudio. El tiempo medio (DE) en la lista de espera fue de 97,33 (55,47) días. Los pacientes de prioridad 1, que normalmente deben ser operados en un plazo de 30 días, estuvieron en la lista de espera por un tiempo medio de 60,51 (20,14) días. Eran principalmente pacientes con litiasis ureteral (25,6%), cáncer de vejiga de alto riesgo o músculo-invasivo (20,9%) y cáncer de próstata de alto riesgo (13,9%). El tiempo medio de espera superaba significativamente el tiempo medio (DE) de espera para cistectomía radical (p = 0,04) y URS (p = 0,003) en 2019.
ConclusionesLa suspensión de la mayoría de las cirugías electivas debido a la pandemia por COVID-19 tuvo un impacto significativo en la lista de espera de cirugía urológica de nuestro centro de alto volumen, especialmente en el grupo de prioridad 1.
The coronavirus disease 2019 (COVID-19) pandemic is the major challenge that healthcare systems around the world are currently facing.1 The high contagiousness and consequent rapid spread of disease, along with its tendency to cause severe pneumonia especially in the elderly such as to require hospitalization and access to intensive care unit (ICU), are among the main factors which contributed to the collapse of the healthcare system in hundreds of cities around the world.2
Spain was one of the countries most affected by COVID-19.3 The first patient diagnosed in Spain was recorded on January 31st 2020 in La Gomera island. Since then, the number of COVID-19 patients increased progressively and exponentially, and the virus spread all across Spanish Regions in a fast and relentless way.3 The state of alarm and the national lockdown was imposed on 14th March 2020. The Region of Madrid was the most affected area in Spain, with 66,338 cases and 8847 deaths COVID-19 related on May 19th 2020.
Due to the health emergency, medical and surgical priorities changed dramatically, with a profound impact on hospital organization. Almost all elective activities were suspended to save resources for COVID-19 cases, as a result of the limited availability of healthcare personnel, medical devices, and hospital beds.3–5 It meant the cancellation of a large number of surgeries (oncological and non-oncological) as well as outpatient services.6
The suspension of most elective surgeries caused the lengthening of urology surgical waiting lists with possible repercussions on the health of patients, especially those who were waiting for oncological surgery.7 Once overcome the peak of the COVID-19 outbreak and normal surgical activities slowly resume, a meticulous waiting list prioritization is necessary to limit the impact of waiting times on patient prognosis.3,8
The primary aim of the present study was to evaluate the impact of COVID-19 outbreak on urology surgical waiting list in a high-volume Spanish hospital. The secondary objective was to discuss current recommendations and evidence for a proper surgical waiting lists prioritization in the early post-COVID-19 era.
Materials and methodsStudy designWe designed an observational descriptive study, in which all patients included in the urology surgical waiting list of our centre (Hospital Universitario 12 de Octubre, Madrid, Spain) on May 1st 2020 were analyzed.
Center characteristics and reorganization in the COVID-19 eraOur hospital is a third-level centre, and one of the main hospitals in the Region of Madrid, with 1256 beds and an urban healthcare area with 445,550 inhabitants. Under normal conditions, the Urology Department uses a mean of 15 operating rooms per week for major surgeries, with a mean of 150–200 major urological procedures performed every month.
All elective surgical procedures were suspended on March 16th 2020, therefore the analysis of waiting list was performed 46 days after the suspension of elective surgery. From that date, only the urgent or life-threatening conditions were allowed. Between March 16th and May 1st, 24 urological surgical procedures were performed, all due to the urgency of the cases. Also, all non-essential face-to-face outpatient activity was interrupted and replaced by telephone follow-up (telemedicine),9 to avoid unnecessary visits to the hospital.
Data collection and variablesAll data were collected from the electronic medical system. The baseline variables recorded for each patient were: age, gender, priority on the waiting list, main urological disease, type of scheduled surgery, and waiting time.
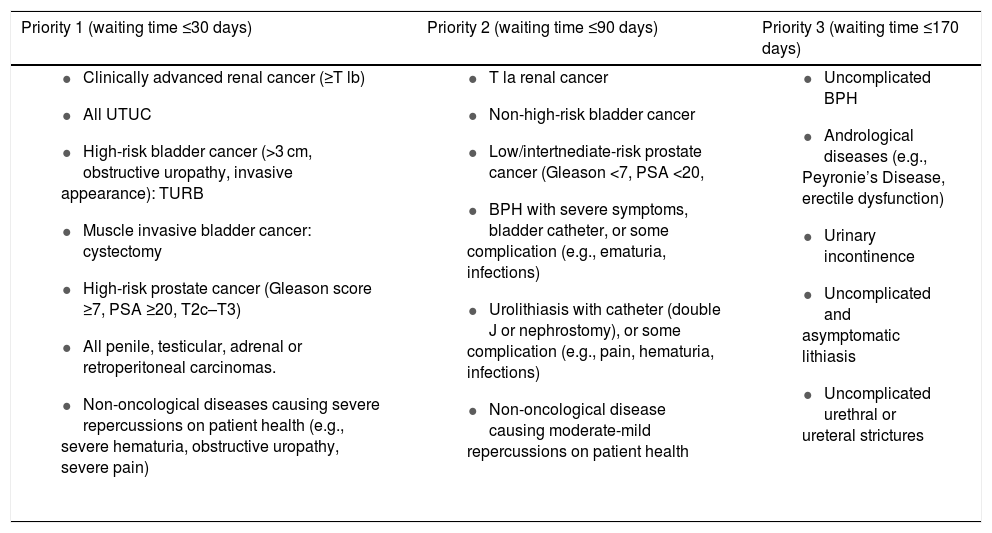
Regarding the priority, at the time of inclusion in the surgical waiting list, the patient was placed in a priority group ranging from 1 to 3. The inclusion criteria and the recommended waiting time for each group were reported in Table 1.
Priority groups: inclusion criteria and recommended waiting times.
| Priority 1 (waiting time ≤30 days) | Priority 2 (waiting time ≤90 days) | Priority 3 (waiting time ≤170 days) |
|---|---|---|
|
|
|
UTUC: upper tract urothelial carcinoma; TURB: transurethral resection of the bladder; BPH: benign prostatic hyperplasia. PSA: prostate specific antigen.
In addition, the following characteristics of each disease were collected:
- -
Bladder and renal cancer: number and size of tumours.
- -
Prostate cancer: Gleason score (GS) and PSA.
- -
Benign prostatic hyperplasia (BPH): size of the prostate.
- -
Urolithiasis: number, size, and location of stones.
Additional variables recorded were: the presence of urinary catheter (bladder or ureteral), number of accesses to the emergency department due to urological diseases, evidence of COVID-19 infection in the medical history, number of deaths and their cause.
We also collected last year (2019) mean surgical times (days from inclusion on the waiting list to surgery) of different procedures.
StatisticsThe statistical analysis was performed with IBM SPSS Statistics® (IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY). The categorical variables were described as frequencies and percentages, while quantitative variables were presented as means and standard deviations (SD). Student’s t-test was used to analyze continuous variables, while Chi-squared test was performed for categorical. ANOVA analysis and Pearson correlation coefficient were used to compare priority groups and to assess the relationships between continuous variables, respectively. A p-value of <0.05 was considered statistically significant.
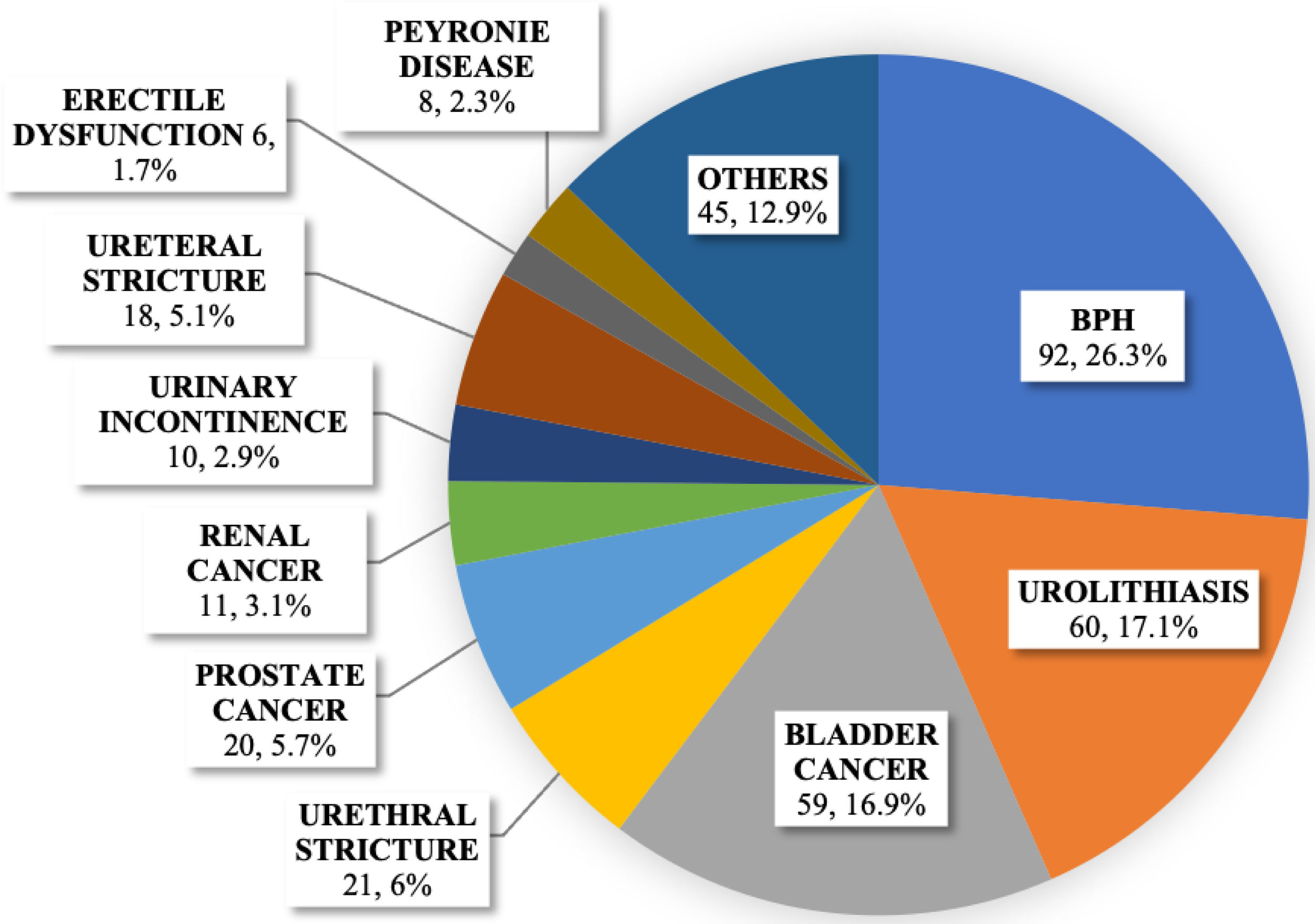
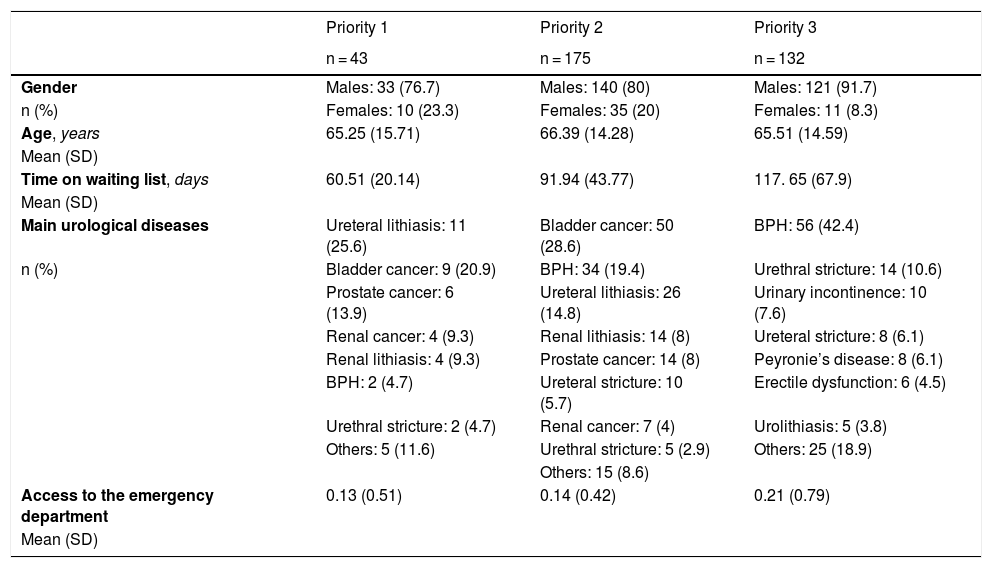
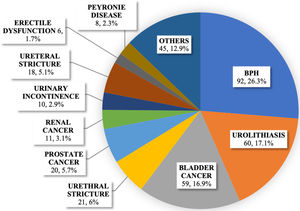
ResultsGlobal seriesA total of 350 patients were included on the surgical waiting list on May 1st 2020. The mean (SD) age was 65.92 (14.62), 294 (84%) subjects were male and 56 (16%) female. Forty-three patients (12.3%) had priority 1, 175 (50%) priority 2, and 132 (37.7%) priority 3. The mean (SD) time on the waiting list was 97.33 (55.47) days. There was a predominance of BPH (26.3%), urolithiasis (17.1%), and bladder cancer (16.9%). The main urological diseases on the waiting list were summarized in Fig. 1.
Analysis of priority groupsOn May 1st 2020, coinciding with the resumption of elective surgery, priority 1 patients who normally should undergo surgery within 30 days, were on the waiting list for a mean (SD) time of 60.51 (20.14) days, more than double the maximum recommended time. Priority 2 patients, who normally should undergo surgery within 90 days, were on the waiting list for a mean (SD) time of 91.94 (43.77) days. Finally, priority 3 patients, who normally should undergo surgery within 170 days, were on the waiting list for a mean (SD) time of 117.65 (67.9) days. The complete analysis of priority groups was reported in Table 2.
Patient characteristics according to the priority group.
| Priority 1 | Priority 2 | Priority 3 | |
|---|---|---|---|
| n = 43 | n = 175 | n = 132 | |
| Gender | Males: 33 (76.7) | Males: 140 (80) | Males: 121 (91.7) |
| n (%) | Females: 10 (23.3) | Females: 35 (20) | Females: 11 (8.3) |
| Age, years | 65.25 (15.71) | 66.39 (14.28) | 65.51 (14.59) |
| Mean (SD) | |||
| Time on waiting list, days | 60.51 (20.14) | 91.94 (43.77) | 117. 65 (67.9) |
| Mean (SD) | |||
| Main urological diseases | Ureteral lithiasis: 11 (25.6) | Bladder cancer: 50 (28.6) | BPH: 56 (42.4) |
| n (%) | Bladder cancer: 9 (20.9) | BPH: 34 (19.4) | Urethral stricture: 14 (10.6) |
| Prostate cancer: 6 (13.9) | Ureteral lithiasis: 26 (14.8) | Urinary incontinence: 10 (7.6) | |
| Renal cancer: 4 (9.3) | Renal lithiasis: 14 (8) | Ureteral stricture: 8 (6.1) | |
| Renal lithiasis: 4 (9.3) | Prostate cancer: 14 (8) | Peyronie’s disease: 8 (6.1) | |
| BPH: 2 (4.7) | Ureteral stricture: 10 (5.7) | Erectile dysfunction: 6 (4.5) | |
| Urethral stricture: 2 (4.7) | Renal cancer: 7 (4) | Urolithiasis: 5 (3.8) | |
| Others: 5 (11.6) | Urethral stricture: 5 (2.9) | Others: 25 (18.9) | |
| Others: 15 (8.6) | |||
| Access to the emergency department | 0.13 (0.51) | 0.14 (0.42) | 0.21 (0.79) |
| Mean (SD) |
BPH: benign prostatic hyperplasia; SD: standard deviation.
Fifty-nine (16.9%) patients were on the waiting list for bladder cancer. Fifty-two (88.1%) subjects were waiting for a transurethral resection of the bladder (TURB) and 7 (11.9%) for a radical cystectomy. The mean (SD) size tumour was 16.2 mm (10.3). Nine (15.3%) patients were in the priority group 1, whereas 50 (84.7%) in the priority group 2. The mean (SD) time on the waiting list was 78.54 (53.70) days.
Renal cancerEleven (3.1%) patients with renal cancer. Six (54.5%) subjects were waiting for a partial nephrectomy and 5 (45.5%) for a radical nephrectomy. The mean (SD) size of the tumour was 36.6 mm (14.0). Four (36.4%) patients were in the priority group 1, whereas 7 (63.6%) in the priority group 2. The mean (SD) time on the waiting list was 68 (21.24) days.
Prostate cancerTwenty (5.7%) patients were on the waiting list for prostate cancer, waiting for a laparoscopic radical prostatectomy. The mean (SD) PSA was 8.1 (4.1) ng/mL. Three (15%) patients had GS 3 + 3 or Gleason-Grade 1 (GG, International-Society-of-Urological-Pathology classification),10 eight (40%) GS 3 + 4 (GG 2), six (30%) GS 4 + 3 (GG 3), and three (15%) GS 4 + 4 (GG 4). Six (30%) patients were in the priority group 1, whereas 14 (70%) in the priority group 2. The mean (SD) time on the waiting list was 70.85 (26.25) days.
BPHNinety-two (26.3%) patients with BPH were on the waiting list. A transurethral resection of the prostate (TURP), was planned in 37 (40.2%) patients (prostate size <70cc) and a holmium laser enucleation of the prostate (HoLEP) in 55 (59.8%) patients (prostate size ≥70cc). The mean (SD) size of the prostate was 72.5cc (40.0). Twenty-two subjects (23.9%) had a bladder catheter. Two (2.2%) patients were in the priority group 1, 34 (36.9%) in the priority group 2, and 56 (60.9%) in the priority group 3. The mean (SD) time on the waiting list was 110.56 (68.25) days.
UrolithiasisSixty (17.1%) patients were on the waiting list for urolithiasis. Twenty (33.3%) subjects had kidney stones, 12 of them (60%) were waiting for a retrograde intrarenal surgery (RIRS) and 8 (40%) for a percutaneous nephrolithotomy (PCNL). Thirty-nine (65%) patients had ureteral lithiasis and were waiting for a ureteroscopy (URS), 1 (1.7%) subject had a bladder lithiasis. Thirty-four (56.7%) patients had a double-J stent. The mean (SD) size of stones was 11.7 mm (9.9). Fifteen (25.0%) subjects were in the priority group 1, 40 (66.7%) in the priority group 2, and 5 (8.3%) in the priority group 3. The mean (SD) time on the waiting list was 93.54 (41.85) days.
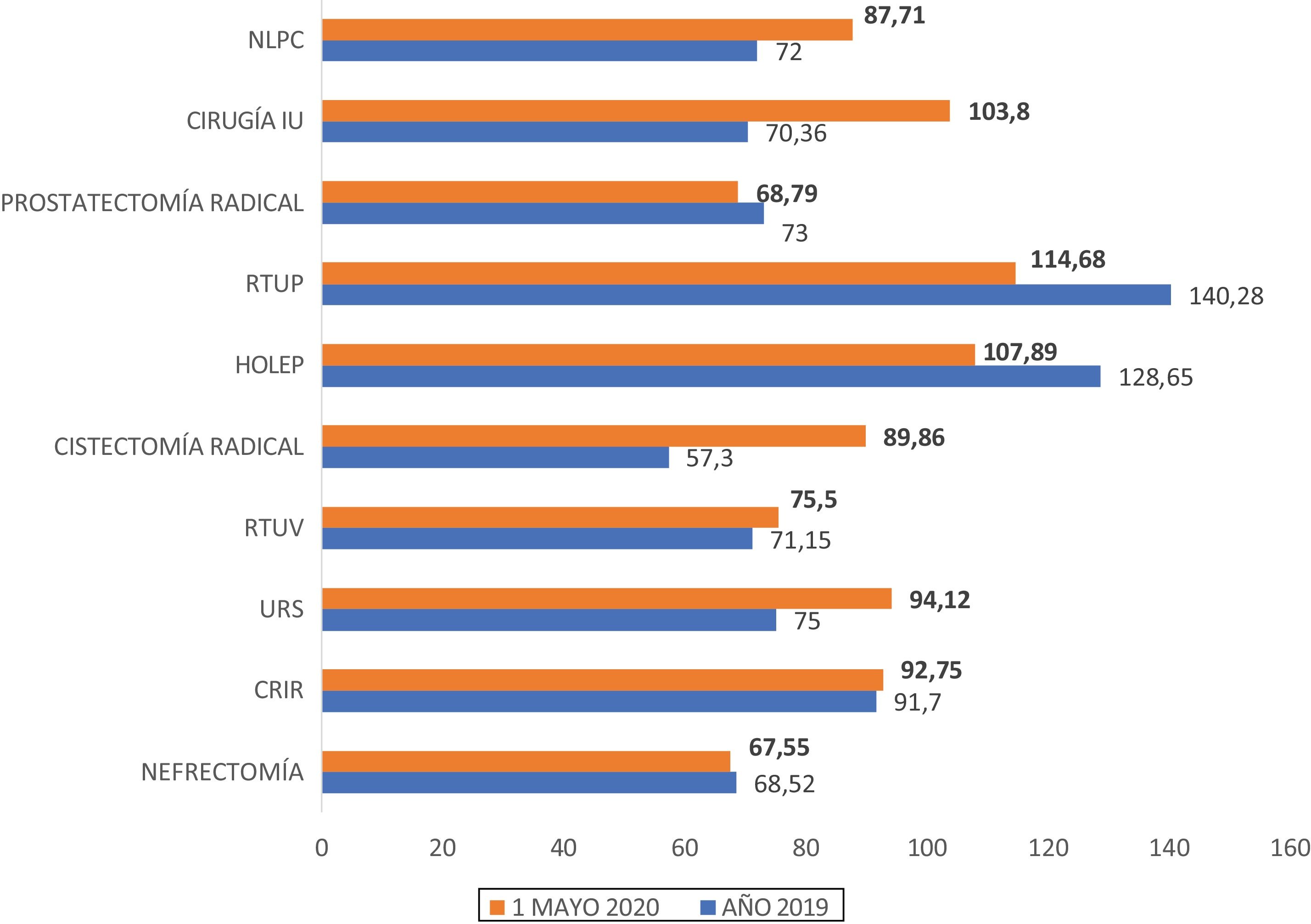
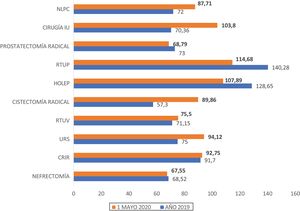
Analysis of waiting timesThe mean waiting times for the surgical treatments on May 1st 2020 (days from inclusion on the waiting list to May 1st 2020) were compared with the mean time to surgery in 2019 (days from inclusion on the waiting list to surgery). The mean waiting time on May 1st 2020 had already exceeded the mean time to surgery in 2019 in TURB (75.50 vs 71.15 days; p = 0.56), radical cystectomy (89.86 vs 57.30 days, p = 0.04), URS (94.12 vs 75.0 days; p = 0.003), PNCL (87.71 vs 72.0 days; p = 0.4), RIRS (92.75 vs 91.70 days; p = 0.66), and urinary incontinence surgery (103.80 vs 70.36 days; p = 0.08). The complete comparison of waiting times was shown in Fig. 2.
Mean waiting time (days) for surgery: May 1st 2020 vs Year 2019.
PCNL: percutaneous nephrolithotomy, UI: urinary incontinence; TURP: transurethral resection of the prostate, HoLEP: holmium laser enucleation of the prostate, TURB: transurethral resection of the bladder, URS: ureteroscopy, RIRS: retrograde intrarrenal surgery.
Patients, since inclusion on the surgical waiting list, went to the emergency department due to their urological condition a mean (SD) of 0.2 (0.6) times.
We found a higher number of emergency room visits in patients with a urinary catheter (p < 0.01). Overall, 29 (8.3%) patients on the waiting list had a bladder catheter and 51 (14.6%) a double J stent. No significant difference was found among the priority groups regarding the access to the emergency department (p = 0.61). Statistically significant correlation with emergency room visits was found for size of the prostate (p = 0.01), but not for stones size (p = 0.9).
Six (1.7%) patients died while on the waiting list, all in April 2020. The cause of death was COVID-19 infection in 3 (50%) patients, and unknown in the other 3 (50%). The mean (SD) age of this subgroup was 86.7 (5.4) years, and the male:female ratio was 1:1. Three (50%) of deceased subjects had a ureteral lithiasis, 1 (16.7%) a bladder cancer, 1 (16.7%) a urethral stricture, and 1 (16.7%) a ureteral stricture.
Lastly, 13 (3.7%) patients had evidence in their medical history of COVID-19 infection diagnosed with a nasopharyngeal swab. The mean (SD) age of these subjects was 69.8 (12.0) years, 9 (69.2%) were male and 4 (30.8 %) female.
DiscussionThe COVID-19 pandemic represented a challenge for healthcare systems around the world.11 The exponential increase in the number of cases resulted into an urgent need to stop most of the medical and surgical activities not directly involved in the treatment of COVID-19 patients in order to save resources for this purpose.8
The suspension of elective surgery, therefore, appears to be a reasonable strategy to safeguard the health of patients. Mortality can reach 20.5% in asymptomatic carriers or people in the incubation period undergoing elective surgery, and surgical procedures would seem to accelerate the progression of COVID-19.12 In addition, it seems that cancer patients are at a higher risk of death for COVID-19 and hospitalization for surgery can obviously be a risk factor for infection.13 On the other hand, there is a real concern about the impact that delayed treatments could have, especially for oncological patients waiting for surgery.5,7,14
A pragmatic approach is needed to cope with this scenario and to find suitable strategies to deal with surgical waiting lists in post-COVID19 era. As the situation is evolving rapidly during the pandemic, protocols and recommendations are constantly being updated and urologists are “learning on the go”.15 The prioritization strategy of surgical patients should be based on an in-depth analysis of the waiting lists as well as on the most up-to-date evidence available.16–18
This study analyzes the impact of COVID-19 on urology surgical waiting lists, providing objective data on the consequences of the suspension of elective surgery. Priority 1 patients who normally should undergo surgery within 30 days, were on the waiting list for a mean time of 60.5 days, more than double the maximum recommended time. They were mainly patients with ureteral lithiasis (25.6%), high-risk or muscle-invasive bladder cancer (20.9%) and high-risk prostate cancer (13.9%). The mean waiting times of priority groups 2 and 3 were just above (91.9 vs. 90 days) and below (117.6 vs. 170 days) the maximum recommended time, at the moment of the analysis respectively. This result can be explained by longer recommended waiting times than in group 1. The mean waiting time on May 1st 2020 was greater than the mean surgical times in 2019 for radical cystectomy, URS, urinary incontinence surgery, PNCL, RIRS and TURB, with statistically significant differences in the first three. In any case, the slow and gradual initial resumption of elective surgical activities and the prioritization of selected patients will likely lead to a further lengthening of waiting times in all groups, with greater repercussions on priority groups 2 and 3.
The EAU Guidelines Office worked to establish a Rapid-Reaction-Group (GORRG), in order to provide a visual guide to manage the health situation related to COVID-19.16,17 In these documents, each urological condition was categorized into four different priority groups to assist diagnostic and therapeutic decision making in urology departments.
American College of Surgeons, created a guidance document with general recommendations to help resumption of elective surgical activity suspended due to the pandemic.18 In particular, it developed a prioritization plan, in which it recommends considering the use of objective priority scoring systems (e.g., Medically-Necessary-Time-Sensitive-Scoring-System [MeNTS]).19
Ficarra et al.,8 categorized urological procedures to treat cancers during COVID-19 pandemic into four groups: non-deferrable; semi-non-deferrable; deferrable; replaceable by other treatments. Similarly, Stensland et al. elaborated a list of surgeries that should be prioritized if COVID-19 causes the cancellation of most elective surgery.3
Surgical waiting list prioritization strategies should be based on scientific evidence. Patients with high-risk urological cancers should be prioritized because delayed treatment could negatively impact their prognosis.3,7 For example, it is well known that delaying radical cystectomy for muscle-invasive bladder cancer by 90 days, increases pN + rate,20 decreases overall and progression-free survival.21
In any case, the analysis of surgical waiting lists in order to prioritize patients should take into account not only the oncological variables but also the patient’s characteristics such as age and comorbidities. One way to evaluate the clinical impact of waiting time is to study the number of emergency department visits due to the urological disease. In our cohort, we found that patients with a urinary catheter went to emergency room significantly more (p < 0.01), despite the urological emergencies in the COVID-19 era had significantly reduced.22,23
The main limitation of our research is the observational descriptive design. Other relevant weaknesses are the monocentric nature of the study and the inability to analyze the long-term prognosis of patients. Besides, a possible bias could derive from the waiting times already accumulated by the patients at the time of data collection.
ConclusionsThe suspension of most of the elective surgeries due to COVID-19 outbreak had a significant impact on urology surgical waiting list. It is essential to apply appropriate prioritization strategies, based on in-depth analysis of surgical waiting lists, to safeguard the health of patients in the post-COVID19 era.
Please cite this article as: García-Rojo E, Manfredi C, Santos-Pérez-de-la-Blanca R, Tejido-Sánchez Á, García-Gómez B, Aliaga-Benítez M, et al. Impacto del brote de COVID-19 en las listas de espera de cirugía urológica y estrategias de priorización en la era post-COVID-19. Actas Urol Esp. 2021;45:207–214.