The "Coronavirus Disease 2019" (COVID-19) has caused a pandemic of global impact that forced social-political measures to be taken, such as the declaration of the state of alarm in Spain. At the same time, the reorganization of the pediatric medical-surgical activities and infrastructures was carried out, with the consequent suspension of the non-urgent surgical activity of Pediatric Urology. We analyzed the impact of the COVID-19 pandemic on surgical activity in a Pediatric Urology division, as well as surgical complications according to the Clavien-Dindo classification.
Materials and methodsA systematic review of epidemiological, clinical and surgical data was carried out, including complications and readmissions of all patients operated on in the division of Pediatric Urology within the duration of the state of alarm. Five time periods have been created according to the de-escalation phases.
ResultsForty-nine surgical procedures were carried out on 45 patients (8 prior to the implementation of the de-escalation phases). High priority pathologies were the most frequent in the first phases, being the ureteropelvic junction (UPJ) obstruction the most prevalent. Four complications were recorded (8.8%), none of them were respiratory.
ConclusionsThe EAU recommendations for the resumption of surgical activity have allowed a correct, safe and gradual transition to the routine surgical activity in Pediatric Urology. The Clavien-Dindo classification is useful and valid for application in this division. No respiratory complications have been reported that could be attributable to the pandemic situation.
El “Coronavirus Disease 2019” (COVID-19) ha ocasionado una pandemia de repercusión mundial que obligó a tomar medidas social-políticas como la declaración del estado de alarma en España. Paralelamente se llevo a cabo la restructuración de las actividades e infraestructuras medico-quirúrgicas pediátricas, con la consecuente suspensión de la actividad quirúrgica no urgente de Urología Pediátrica. Analizamos la repercusión de la pandemia COVID-19 sobre la actividad quirúrgica en una sección de Urología Pediátrica, así como las complicaciones quirúrgicas según la clasificación de Clavien- Dindo.
Materiales y métodosSe procedió a la revisión sistemática de los datos epidemiológicos, clínicos y quirúrgicos, incluyendo las complicaciones y reingresos de todos los pacientes intervenidos en la sección de Urología Pediátrica desde la declaración del estado de alarma hasta el levantamiento del mismo. Para su estudio se procedió a la división en cinco bloques temporales acorde a las fases de desescalada.
ResultadosSe realizaron 49 intervenciones quirúrgicas en 45 pacientes (8 previos a la implantación de las fases de desescalada). La patología con prioridad alta fue la más frecuente en las primeras fases, siendo la estenosis de la unión pieloureteral (EPU) la más prevalente. Se registraron cuatro complicaciones (8,8%), ninguna de ellas de origen respiratorio.
ConclusionesLas recomendaciones de la EAU para la reanudación de la actividad quirúrgica han permitido una correcta, segura y gradual transición al ritmo quirúrgico habitual en Urología Pediátrica. La clasificación de Clavien- Dindo es útil y válida para su aplicación en está sección. No se han registrados complicaciones respiratorias que pudiesen ser atribuibles a la situación pandémica.
Since December 2019, the outbreak of infectious pneumonia known as coronavirus disease 2019 (COVID-19), caused by the SARS-CoV-2 virus, has spread, causing a pandemic with global repercussions.1 In Spain, which is among European worst affected countries by COVID-19,2 the diagnosed cases increased over five hundred confirmed cases,3 causing the declaration of a state of alarm for the management of the health crisis situation (Royal Decree 463/2020 of March 14th). The affected population included children, who presented less severe clinical pictures, with the most frequent symptoms being fever, cough and rhinorrhea, in the context of upper respiratory infections and pneumonia.3,4
In parallel to the socio-political measures taken with the declaration of the state of alarm, the need to dedicate economic and healthcare resources to adult COVID-19 patients, who were more affected by this pathology than pediatric patients, led to the restructuring of medical-related activities and pediatric surgical procedures, suspending Pediatric Urology non-urgent or elective surgical activity.5 In this scenario, the European Association of Urology (EAU) and the European Society of Pediatric Urology (ESPU) described some recommendations detailing which pediatric urological pathologies should be postponed given the current situation, and which should resume treatment as soon as possible due to their potential clinical repercussion.6,7
Similarly, with the improved situation and the decreasing trend in the number of daily infections and deaths, commercial activity progressively resumed, and isolation restrictions ceased. These de-escalation measures were staged into phases according to each Spanish Autonomous Community (AC) and their number of COVID-19 registered cases. Similarly, children's surgical activity was resumed, adapting the previously established surgical priorities; the EAU/ESPU proposed these to be analogous to the ones previously established.6,7
The Clavien-Dindo classification for surgical complications8 arose from the need to avoid subjectivity when describing complications or deviations in the normal course of the postoperative period. This classification, proposed for the adult population in 2004 and subsequently applied to pediatric patients,9 allows an objective and comparative description of complications based on the treatment required for their management.
The objective of this study was to analyze the impact of the COVID-19 pandemic on the surgical activity of the Pediatric Urology section in a Spanish tertiary hospital since the declaration of the state of alarm, by evaluating the pathologies treated and the prioritization criteria. In the same way, the aim is to study the surgical complications recorded in these patients based on the Clavien-Dindo classification.
Material and methodsStudy designWe conducted a retrospective observational study recording the surgical activity performed by the Pediatric Urology section since the declaration of the state of alarm (Royal Decree 463/2020 of March 14th) until its lifting, on 06/21/2020 (Royal Decree 21/2020 of June 9).
The time period was divided into five phases or time blocks, according to the socio-political measures and the de-escalation phases adopted in Madrid, AC of this hospital. These phases were implemented asymmetrically based on epidemiological data, mobility, and social and economic impact of each AC in Spain. These were established as follows:
- -
Previous phase - Period from the declaration of the state of alarm until the start of the de-escalation measures. From 03/14/2020 to 05/04/2020.
- -
Phase 0 or preparation. From 04/05/2020 to 18/05/2020.
- -
Phase 0 with relief measures (or 0.5). From 05/18/2020 to 05/25/2020.
- -
Phase 1 or initial. From 05/25/2020 to 08/06/2020.
- -
Phase 2 or intermediate. From 08/06/2020 to 21/06/2020.
All patients under 16 years old undergoing surgery for urological pathology, followed or evaluated by the Pediatric Urology section were included after being tested with SARS-CoV-2 PCR. Written consent of parents or legal guardians was required for the performance of the intervention. Patients without parental or legal guardians consent prior to surgical intervention were excluded.
DataWe carried out a systematic review of the epidemiological, clinical and surgical data of the patients by reviewing the electronic health record, including the characteristics of the complications, their treatment and readmissions within the first 30 days after surgery. Likewise, patients were examined for fever or the onset of infectious upper tract symptoms at the first postoperative visit 7–14 days after surgery.
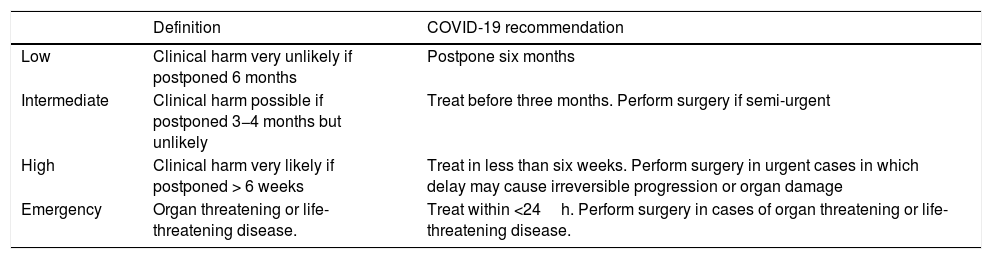
The criteria for the prioritization of surgical procedures were the recommendations indicated by the EAU/ESPU,6,7 differentiating four groups based on the clinical harm entailed by treatment delay (Table 1).
Summary of the recommendations from the EAU/ESPU Pediatric Urology Guidelines Panel applicable during the COVID-19 pandemic.
| Definition | COVID-19 recommendation | |
|---|---|---|
| Low | Clinical harm very unlikely if postponed 6 months | Postpone six months |
| Intermediate | Clinical harm possible if postponed 3−4 months but unlikely | Treat before three months. Perform surgery if semi-urgent |
| High | Clinical harm very likely if postponed > 6 weeks | Treat in less than six weeks. Perform surgery in urgent cases in which delay may cause irreversible progression or organ damage |
| Emergency | Organ threatening or life-threatening disease. | Treat within <24h. Perform surgery in cases of organ threatening or life-threatening disease. |
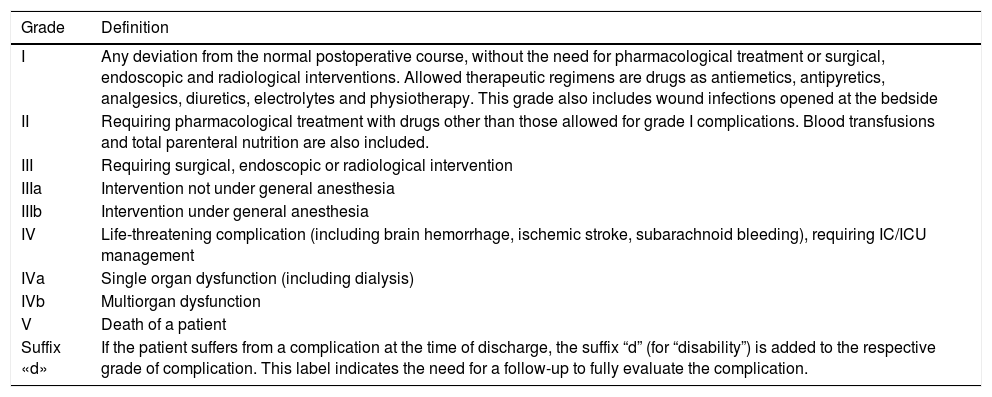
Complications were identified and graded according to the Clavien-Dindo classification, according to the therapy used to treat the complication.8 It encompasses complications in seven grades, as shown in Table 2.
Clavien-Dindo classification of surgical complications.
| Grade | Definition |
|---|---|
| I | Any deviation from the normal postoperative course, without the need for pharmacological treatment or surgical, endoscopic and radiological interventions. Allowed therapeutic regimens are drugs as antiemetics, antipyretics, analgesics, diuretics, electrolytes and physiotherapy. This grade also includes wound infections opened at the bedside |
| II | Requiring pharmacological treatment with drugs other than those allowed for grade I complications. Blood transfusions and total parenteral nutrition are also included. |
| III | Requiring surgical, endoscopic or radiological intervention |
| IIIa | Intervention not under general anesthesia |
| IIIb | Intervention under general anesthesia |
| IV | Life-threatening complication (including brain hemorrhage, ischemic stroke, subarachnoid bleeding), requiring IC/ICU management |
| IVa | Single organ dysfunction (including dialysis) |
| IVb | Multiorgan dysfunction |
| V | Death of a patient |
| Suffix «d» | If the patient suffers from a complication at the time of discharge, the suffix “d” (for “disability”) is added to the respective grade of complication. This label indicates the need for a follow-up to fully evaluate the complication. |
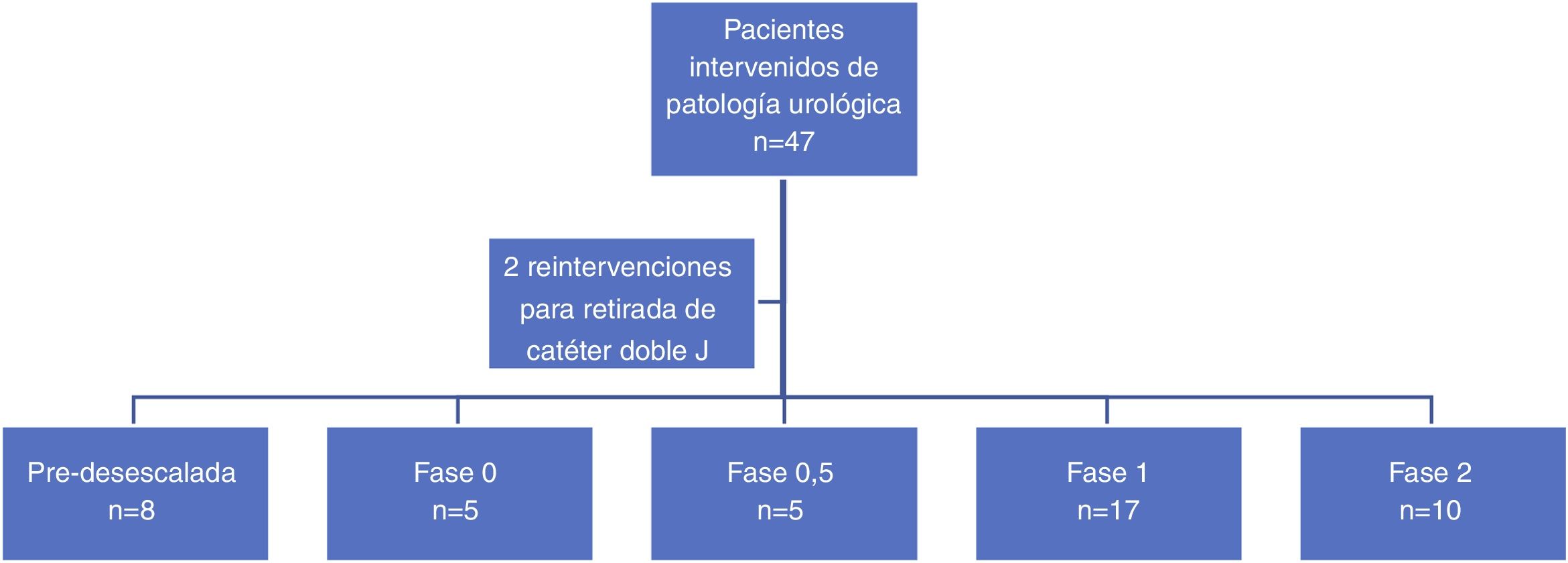
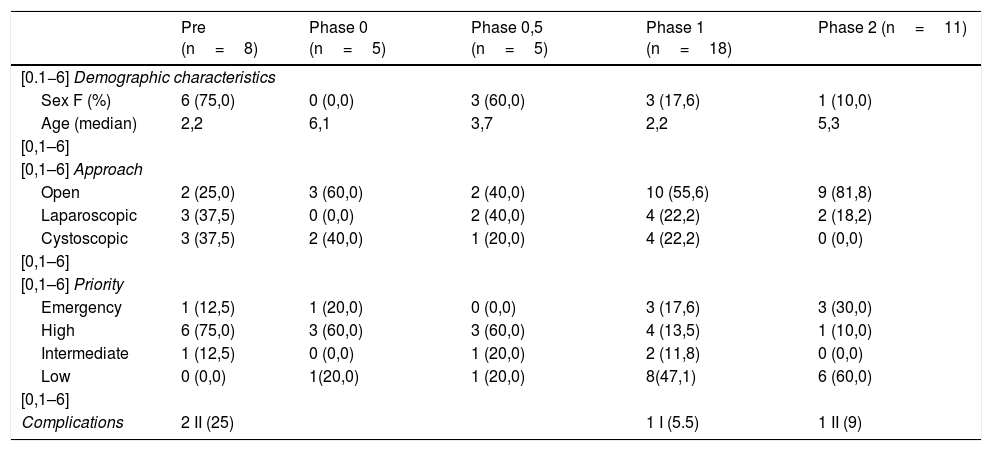
A total of 49 surgeries were performed in 45 patients (13 female patients) in the period of time analyzed (03/13/2020–06/01/2020). Two patients underwent two different procedures in the same surgical act, while two other patients required reoperation within the study period for the removal of the double J placed in the first procedure, being excluded from the comparative analysis. Eight patients underwent surgery before the implementation of the de-escalation phases, and 37 were treated in phases 0–2 of the plan for the transition towards a new normalcy, distributed as shown in Fig. 1.
No patients were excluded for being SARS-CoV-2 positive on PCR, despite the fact that five were considered as such, and the appropriate personal safety measures were taken, given the urgency of surgical intervention (testicular torsion).
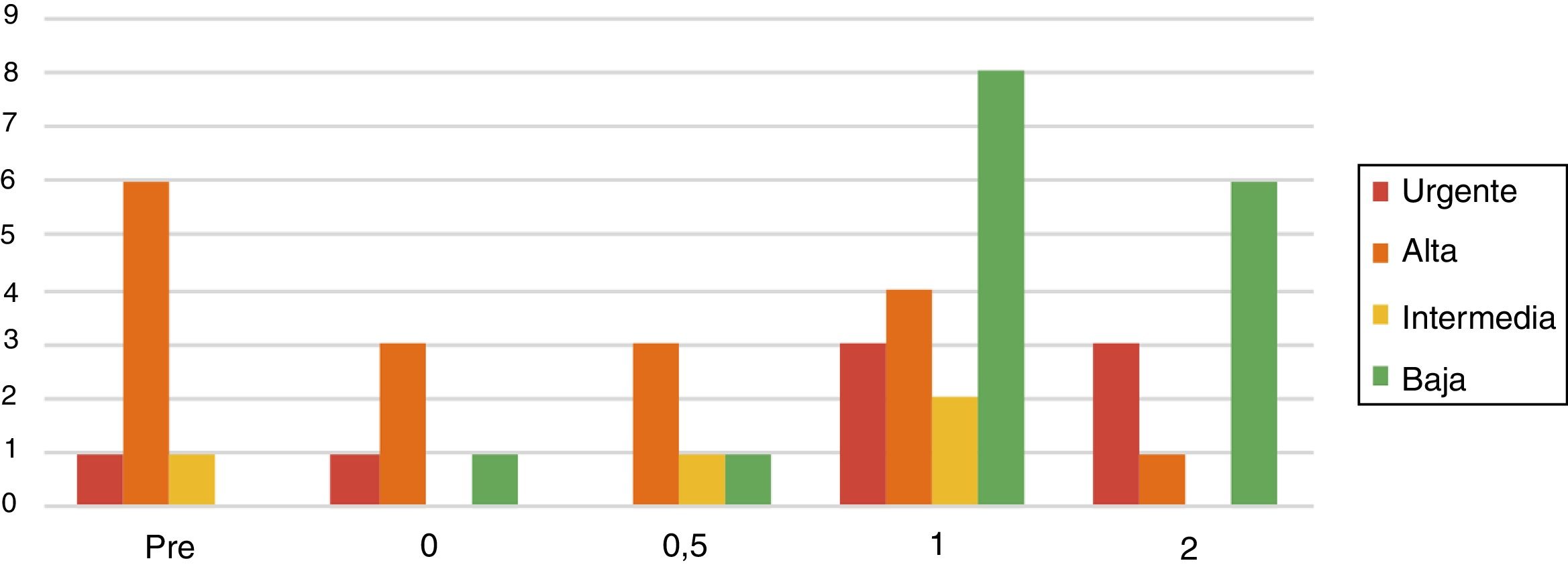
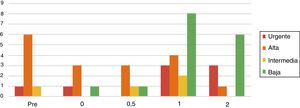
PriorityA larger percentage of high priority surgical interventions was seen across the first three phases of de-escalation analyzed (pre-de-escalation, phase 0 and phase 0.5), which decreased gradually. Conversely, the rate of low priority interventions increased as the de-escalation phases progressed. The phases with the highest proportion of urgent interventions were 1 and 2, with three urgent interventions in each of them (Table 3 and Fig. 2).
Descriptive analysis of the sample in relation to each subgroup of the de-escalation phase. Data are described as absolute frequencies and percentage, respectively.
| Pre (n=8) | Phase 0 (n=5) | Phase 0,5 (n=5) | Phase 1 (n=18) | Phase 2 (n=11) | |
|---|---|---|---|---|---|
| [0.1−6] Demographic characteristics | |||||
| Sex F (%) | 6 (75,0) | 0 (0,0) | 3 (60,0) | 3 (17,6) | 1 (10,0) |
| Age (median) | 2,2 | 6,1 | 3,7 | 2,2 | 5,3 |
| [0,1–6] | |||||
| [0,1–6] Approach | |||||
| Open | 2 (25,0) | 3 (60,0) | 2 (40,0) | 10 (55,6) | 9 (81,8) |
| Laparoscopic | 3 (37,5) | 0 (0,0) | 2 (40,0) | 4 (22,2) | 2 (18,2) |
| Cystoscopic | 3 (37,5) | 2 (40,0) | 1 (20,0) | 4 (22,2) | 0 (0,0) |
| [0,1–6] | |||||
| [0,1–6] Priority | |||||
| Emergency | 1 (12,5) | 1 (20,0) | 0 (0,0) | 3 (17,6) | 3 (30,0) |
| High | 6 (75,0) | 3 (60,0) | 3 (60,0) | 4 (13,5) | 1 (10,0) |
| Intermediate | 1 (12,5) | 0 (0,0) | 1 (20,0) | 2 (11,8) | 0 (0,0) |
| Low | 0 (0,0) | 1(20,0) | 1 (20,0) | 8(47,1) | 6 (60,0) |
| [0,1–6] | |||||
| Complications | 2 II (25) | 1 I (5.5) | 1 II (9) | ||
F: female.
The pathology requiring surgical treatment with more frequency during the time period evaluated was ureteropelvic junction (UPJ) stenosis, reported in 10 patients. The other pathologies are collected in the Appendix (see additional material).
We highlight two patients for their complexity. A patient with Prune belly syndrome, previously followed in his country of origin with creation of a right ureterostomy. He did not provide reports describing his renoureteral anatomy or prior diagnostic-therapeutic procedures and was diagnosed with cryptorchidism. Prior to the laparoscopic approach to perform the first stage of Fowler-Stephens technique, an exploratory cystoscopy was performed, showing an image compatible with previously unsuspected posterior urethral valves, which were resected during the same surgical procedure. Another patient was an 11-year-old boy who had an embryonal vesicoprostatic rhabdomyosarcoma in his personal history. He had undergone surgery twice, at six and nine months old, subsequently receiving adjuvant radiotherapy, and under general surgery surveillance due to the development of a complicated rectourethral fistula with recurrent urinary tract infections. Cystoscopy revealed the fistula with fecaliths passing from the rectum to the urethra which were subsequently removed, favoring the resolution of the episodes without new symptoms until the date of the review.
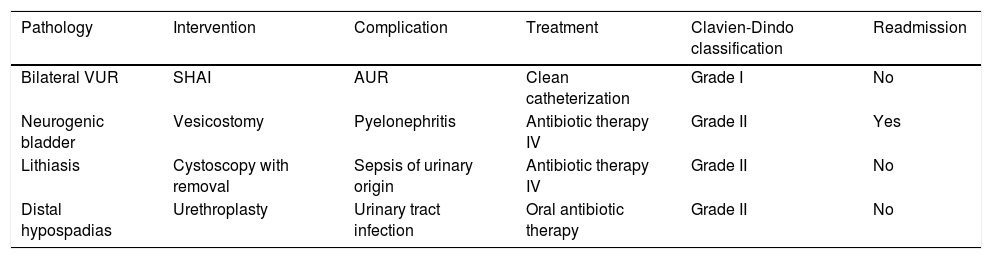
ComplicationsFour complications (8.8%) were recorded, one grade I complication and three grade II complications, according to the Clavien-Dindo classification (Table 4).
Description of the complications recorded, treatment performed and grade, according to the Clavien-Dindo classification.
| Pathology | Intervention | Complication | Treatment | Clavien-Dindo classification | Readmission |
|---|---|---|---|---|---|
| Bilateral VUR | SHAI | AUR | Clean catheterization | Grade I | No |
| Neurogenic bladder | Vesicostomy | Pyelonephritis | Antibiotic therapy IV | Grade II | Yes |
| Lithiasis | Cystoscopy with removal | Sepsis of urinary origin | Antibiotic therapy IV | Grade II | No |
| Distal hypospadias | Urethroplasty | Urinary tract infection | Oral antibiotic therapy | Grade II | No |
VUR: Vesicoureteral reflux; SHAI: Subureteral hyaluronic acid injection; AUR: Acute urine retention; IV: Intravenous.
No respiratory complications or fever of unknown origin were recorded in the postoperative period of the 45 patients.
DiscussionOur study analyzes the impact of the COVID-19 pandemic on the surgical activity in a Pediatric Urology section in a Spanish tertiary hospital, since the declaration of the state of alarm. It describes the successive phases and the gradual resumption of surgical activity, following the indications for urological pathologies to the limited number of surgical hours available. Given the pandemic scenario, it has been demonstrated that surgical activity could be resumed without increasing the risk of respiratory complications following the recommendations of the EAU.
When analyzing the priority of the pathologies requiring surgical intervention, and taking into account that we have followed the EAU recommendations regarding delay of pathologies based on the potential clinical harm that it would entail in the patient, it is not surprising that the period with a larger percentage of high priority procedures was the first one, or the pre-de-escalation phase. There are certain surgical interventions of lower priority that stand out in earlier phases; this can be due to the fact that these procedures had shorter operative time and could be incorporated to the daily surgical activity, prioritizing waiting times for inclusion on the waiting list.
It also interesting that pathologies with high priority (emergency), although without analyzing its statistical significance, were more prevalent in later stages. In this sense, we wanted to highlight the adverse outcome suffered by two thirds of the patients who underwent orchiectomy due to poor appearance of the affected testicle. This is consistent with previous studies that describe more advanced clinical conditions in pediatric patients, probably related to delayed consultation due to fear of COVID-1910 infection. The importance of prompt visits to ER departments in case of diseases of high prevalence and clinical repercussions, such as testicular torsion, should be highlighted, and social awareness in this regard must be increased.
After analyzing the complications, the results show a rate of 8.8%, but no type III or IV complications were registered. These would include those conditions that require surgical intervention or admission to the ICU and, therefore, could be considered as major or very serious complications. Complications of respiratory origin have not been described in our patients; but there were complications of an infectious origin that affected only the urinary tract, with no apparent relationship with the pandemic.
ConclusionsThe COVID-19 infection has implied changes in the pediatric surgical activity in many aspects, having had to adapt the physical, human and material resources to the emergency situation. In Pediatric Urology, the recommendations of the EAU/ESPU for the readjustment of surgical activity have allowed a correct and gradual transition to recovering the department's usual pace.
The Clavien-Dindo classification of surgical complications is useful and valid for application in Pediatric Urology. No respiratory complications, whether infectious or not, have been described in the pediatric population treated during the period of study, without this necessarily showing a null rate of infection.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Merino-Mateo L, Tordable Ojeda C, Cabezalí Barbancho D, Gómez Fraile A. Repercusión de la pandemia COVID-19 sobre la actividad quirúrgica de Urología Pediátrica: análisis de las complicaciones posquirúrgicas según la clasificación de Clavien-Dindo. Actas Urol Esp. 2020;44:659–664.