The aim was to determine the impact of COVID-19 pandemic on urolithiasis presentation and management.
MethodsIn this retrospective study, we comparatively evaluated urgent and elective procedures due to urolithiasis during the early eight months of the COVID-19 pandemic (March 1, 2020, to October 31, 2020) compared to the same period a year before, and between waves. The student’s t-test, chi-square test, Mann–Whitney U test and Fisher’s exact test were used to compare the patients’ characteristics and outcomes between the two periods and waves.
ResultsFive hundred and thirty procedures were included. The overall numbers of surgical procedures due to urolithiasis were similar between pre-pandemic and pandemic periods. Regarding elective surgery, our data draw attention to the increased complication rate in the pandemic times, but no statistically significant differences in terms of types of procedures and need for complementary treatments were observed. We noted that patterns of presentation of complicated renal colic were different during COVID-19 pandemic, with a higher number of days after the onset of symptoms and a higher proportion of patients presenting acute kidney injury. Furthermore, a significant increase of creatinine levels at presentation in first wave was detected, and a growth in the number of urgent procedures after the first wave was noted, owing to the delay in urolithiasis treatment and diagnosis.
ConclusionThe COVID-19 pandemic has negatively affected both urgent and elective management of urolithiasis. Lessons about the management of urolithiasis in this context should be learned to avoid fatal complications and improve standards of care.
El objetivo del estudio fue analizar el impacto de la pandemia COVID-19 en la presentación y el manejo de la patología litiásica.
MétodosEstudio retrospectivo comparativo de los procedimientos (urgentes y electivos) por litiasis durante los primeros ocho meses de la pandemia (01/03/2020 al 31/10/2020), comparándose con el mismo período de 2019, y entre olas. Las pruebas utilizadas fueron la prueba exacta de Fisher, t de Student, chi-cuadrado y U de Mann–Whitney.
ResultadosSe analizaron 530 procedimientos. El número total de procedimientos quirúrgicos por patología litiásica fue similar entre los dos períodos. En cuanto a la cirugía electiva, se identificó un aumento en la tasa de complicaciones en el período de pandemia, pero no se observaron diferencias estadísticamente significativas en cuanto a tipos de procedimientos realizados y necesidad de tratamientos complementarios. El patrón de presentación del cólico renoureteral complicado fue diferente durante la pandemia, con mayor número de días desde del inicio de los síntomas hasta la consulta y mayor proporción de pacientes con fracaso renal agudo. Asimismo, se detectó un aumento significativo de los niveles de creatinina en la primera ola, así como un incremento en el número de procedimientos urgentes tras la primera ola debido al retraso en el tratamiento y diagnóstico de la patología litiásica.
ConclusionesLa pandemia COVID-19 ha impactado negativamente en el tratamiento urgente y electivo de la litiasis. Se deben aprender lecciones sobre el manejo de la litiasis en este contexto para evitar complicaciones graves y mejorar los estándares de atención.
Since COVID-19 outbreak in Wuhan, China, in late 2019, this infectious disease has experienced alarming levels of spread and severity. WHO declared COVID-19 a pandemic on March 11, 2020.1,2 The COVID-19 pandemic has become global public health crisis of considerable magnitude and has impacted on standard urology practice. The availability of resources, severity of the disease, consequences of delayed treatment and dynamics of the pandemic are factors that have influenced on the provision of urology care.3
The capacity of healthcare systems to treat surgical patients has markedly decreased in the time of COVID-19 and important efforts have been made to develop guidelines to fairly allocate the scarce medical resources. COVID-19 pandemic in Europe has implied that many elective surgical procedures have been postponed or cancelled. As a consequence, many conditions have worsened by the delay in receiving appropriate treatment.4
Oncological conditions were prioritised over benign conditions, such as urolithiasis, during COVID-19 pandemic, and benign conditions were deferred when feasible and safe. These findings have been confirmed through a multi-national survey promoted by the Société Internationale d’Urologie (SIU).5
Urolithiasis accounts for a considerable portion of the clinical workload for urologists and consumes significant resources.6 COVID-19 pandemic waves are putting a halt on elective surgical management of kidney and ureteral stones. Obstructive uropathy secondary to urolithiasis can result in potentially life-threatening urosepsis and pyonephrosis, or can lead to severe acute kidney injury (AKI), hyperkalemia, or even irreversible kidney damage. In the present article, we review how COVID-19 has impacted on urolithiasis care. We describe how this impacted both in elective and urgent procedures and how it unfolds over 2 waves.
Given the possibility of the pandemic re-emerging or upcoming waves, we should learn some lessons about the management of urolithiasis.7 Drawing on these insights may aid prioritizing elective procedures, facing emergent decompensations and morbidity, and developing strategies for the prevention and treatment of urinary stones during this COVID-19 pandemic period.
Materials and methodsStudy designA retrospective study was conducted. All procedures due to urolithiasis during the early eight months of the COVID-19 pandemic (March 1, 2020 to October 31, 2020) and during the same time in 2019 (March 1, 2019 to October 31, 2019) were reviewed and analysed. We compared either urgent and non-urgent (or elective) procedures before and during the pandemic.
We also evaluated the differences between the 1st and 2nd waves of the virus. All patients admitted between 1st March and 30th June were considered to be in the 1st wave and those admitted from 1st July to 31st October in the 2nd wave.
In the centre where this study was conducted, when the SARS-CoV-2 epidemiological situation improved, an attempt was made to maintain or increase surgical activity, with the prime goal of prioritizing oncological patients and potentially life-threatening conditions like urolithiasis.
VariablesThe variables examined in both groups (elective and urgent procedures) included age, gender, age-adjusted Charlson Comorbidity Index (ACCI), type of procedure (urgent or elective), operative time, hospital stay, date of procedure, number of stones, stone size (mm), radiodensity (Hounsfield units, HU) and complications according to the Clavien–Dindo system. For the urgent surgery group, cause for urinary diversion and days from the onset of symptoms were retrieved. For the elective surgery group, need for further procedures, residual stone fragments (mm), estimated stone size during surgery and days waiting to elective surgery were obtained.
Laboratory data were also collected, such as creatinine (Cr) level, estimated glomerular filtration rate (eGFR), C-reactive protein level (CRP) and white blood cell (WBC) count for patients who underwent urgent procedures.
Furthermore, COVID-19 infections during postoperative period (30 days after procedure) or during waiting time to elective surgery were registered.
Statistical analysisCategorical variables are expressed as frequencies and percentages, and continuous variables are expressed as mean and standard deviation. After testing for normality of distribution, continuous variables were compared using the Student unpaired t-test or the Mann–Whitney U-test, and categorical variables were compared using the chi-squared test or Fisher’s exact test. A p-value of <0.05 was considered to indicate statistical significance. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) version 25.
ResultsThe number of surgical procedures was similar between the two periods. There were 140 and 162 elective surgeries in the pandemic and pre-pandemic eras, respectively. Furthermore, there were 115 and 113 patients who underwent urgent procedures in pandemic and pre-pandemic eras, respectively. Below, we present the results separately: the differences in regard to elective procedures before and during the pandemic period, and similarly regarding urgent procedures.
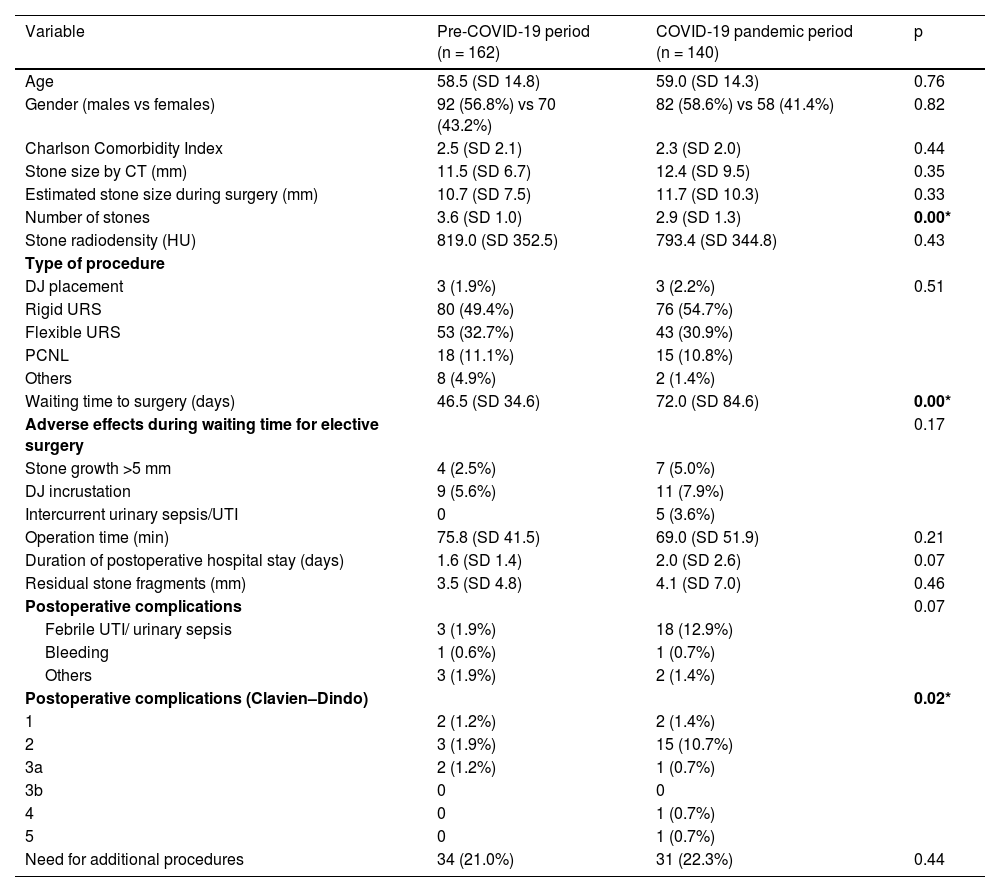
Regarding elective surgery (Table 1), we found no differences in types of procedures, duration of postoperative hospital stay, stone fragments and need for complementary treatments. We identified an increased complication rate in the pandemic times and waiting time to elective surgery.
Characteristics of patients who underwent non-urgent procedures in both pandemic and pre-pandemic periods.
| Variable | Pre-COVID-19 period (n = 162) | COVID-19 pandemic period (n = 140) | p |
|---|---|---|---|
| Age | 58.5 (SD 14.8) | 59.0 (SD 14.3) | 0.76 |
| Gender (males vs females) | 92 (56.8%) vs 70 (43.2%) | 82 (58.6%) vs 58 (41.4%) | 0.82 |
| Charlson Comorbidity Index | 2.5 (SD 2.1) | 2.3 (SD 2.0) | 0.44 |
| Stone size by CT (mm) | 11.5 (SD 6.7) | 12.4 (SD 9.5) | 0.35 |
| Estimated stone size during surgery (mm) | 10.7 (SD 7.5) | 11.7 (SD 10.3) | 0.33 |
| Number of stones | 3.6 (SD 1.0) | 2.9 (SD 1.3) | 0.00* |
| Stone radiodensity (HU) | 819.0 (SD 352.5) | 793.4 (SD 344.8) | 0.43 |
| Type of procedure | |||
| DJ placement | 3 (1.9%) | 3 (2.2%) | 0.51 |
| Rigid URS | 80 (49.4%) | 76 (54.7%) | |
| Flexible URS | 53 (32.7%) | 43 (30.9%) | |
| PCNL | 18 (11.1%) | 15 (10.8%) | |
| Others | 8 (4.9%) | 2 (1.4%) | |
| Waiting time to surgery (days) | 46.5 (SD 34.6) | 72.0 (SD 84.6) | 0.00* |
| Adverse effects during waiting time for elective surgery | 0.17 | ||
| Stone growth >5 mm | 4 (2.5%) | 7 (5.0%) | |
| DJ incrustation | 9 (5.6%) | 11 (7.9%) | |
| Intercurrent urinary sepsis/UTI | 0 | 5 (3.6%) | |
| Operation time (min) | 75.8 (SD 41.5) | 69.0 (SD 51.9) | 0.21 |
| Duration of postoperative hospital stay (days) | 1.6 (SD 1.4) | 2.0 (SD 2.6) | 0.07 |
| Residual stone fragments (mm) | 3.5 (SD 4.8) | 4.1 (SD 7.0) | 0.46 |
| Postoperative complications | 0.07 | ||
| Febrile UTI/ urinary sepsis | 3 (1.9%) | 18 (12.9%) | |
| Bleeding | 1 (0.6%) | 1 (0.7%) | |
| Others | 3 (1.9%) | 2 (1.4%) | |
| Postoperative complications (Clavien–Dindo) | 0.02* | ||
| 1 | 2 (1.2%) | 2 (1.4%) | |
| 2 | 3 (1.9%) | 15 (10.7%) | |
| 3a | 2 (1.2%) | 1 (0.7%) | |
| 3b | 0 | 0 | |
| 4 | 0 | 1 (0.7%) | |
| 5 | 0 | 1 (0.7%) | |
| Need for additional procedures | 34 (21.0%) | 31 (22.3%) | 0.44 |
P-value marked with bold and asterisk (*) indicate a significant difference.
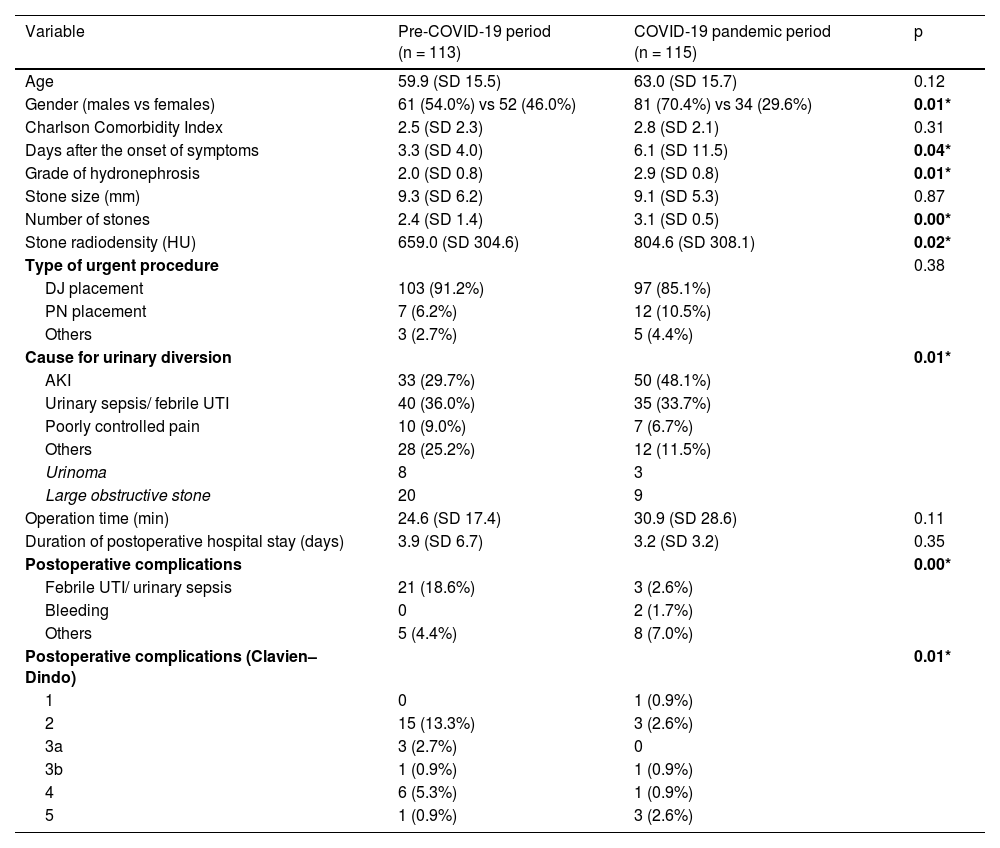
With regard to urgent surgery (Table 2), the overall number of Emergency Department visits was equivalent between the two periods. We detected significant changes in patterns of presentation of renal colic: patient profile (male:female ratio), number of days after the onset of symptoms, stone characteristics and cause for urinary diversion.
Comparison of features of urgent procedures between the two periods.
| Variable | Pre-COVID-19 period (n = 113) | COVID-19 pandemic period (n = 115) | p |
|---|---|---|---|
| Age | 59.9 (SD 15.5) | 63.0 (SD 15.7) | 0.12 |
| Gender (males vs females) | 61 (54.0%) vs 52 (46.0%) | 81 (70.4%) vs 34 (29.6%) | 0.01* |
| Charlson Comorbidity Index | 2.5 (SD 2.3) | 2.8 (SD 2.1) | 0.31 |
| Days after the onset of symptoms | 3.3 (SD 4.0) | 6.1 (SD 11.5) | 0.04* |
| Grade of hydronephrosis | 2.0 (SD 0.8) | 2.9 (SD 0.8) | 0.01* |
| Stone size (mm) | 9.3 (SD 6.2) | 9.1 (SD 5.3) | 0.87 |
| Number of stones | 2.4 (SD 1.4) | 3.1 (SD 0.5) | 0.00* |
| Stone radiodensity (HU) | 659.0 (SD 304.6) | 804.6 (SD 308.1) | 0.02* |
| Type of urgent procedure | 0.38 | ||
| DJ placement | 103 (91.2%) | 97 (85.1%) | |
| PN placement | 7 (6.2%) | 12 (10.5%) | |
| Others | 3 (2.7%) | 5 (4.4%) | |
| Cause for urinary diversion | 0.01* | ||
| AKI | 33 (29.7%) | 50 (48.1%) | |
| Urinary sepsis/ febrile UTI | 40 (36.0%) | 35 (33.7%) | |
| Poorly controlled pain | 10 (9.0%) | 7 (6.7%) | |
| Others | 28 (25.2%) | 12 (11.5%) | |
| Urinoma | 8 | 3 | |
| Large obstructive stone | 20 | 9 | |
| Operation time (min) | 24.6 (SD 17.4) | 30.9 (SD 28.6) | 0.11 |
| Duration of postoperative hospital stay (days) | 3.9 (SD 6.7) | 3.2 (SD 3.2) | 0.35 |
| Postoperative complications | 0.00* | ||
| Febrile UTI/ urinary sepsis | 21 (18.6%) | 3 (2.6%) | |
| Bleeding | 0 | 2 (1.7%) | |
| Others | 5 (4.4%) | 8 (7.0%) | |
| Postoperative complications (Clavien–Dindo) | 0.01* | ||
| 1 | 0 | 1 (0.9%) | |
| 2 | 15 (13.3%) | 3 (2.6%) | |
| 3a | 3 (2.7%) | 0 | |
| 3b | 1 (0.9%) | 1 (0.9%) | |
| 4 | 6 (5.3%) | 1 (0.9%) | |
| 5 | 1 (0.9%) | 3 (2.6%) |
P-value marked with bold and asterisk (*) indicate a significant difference.
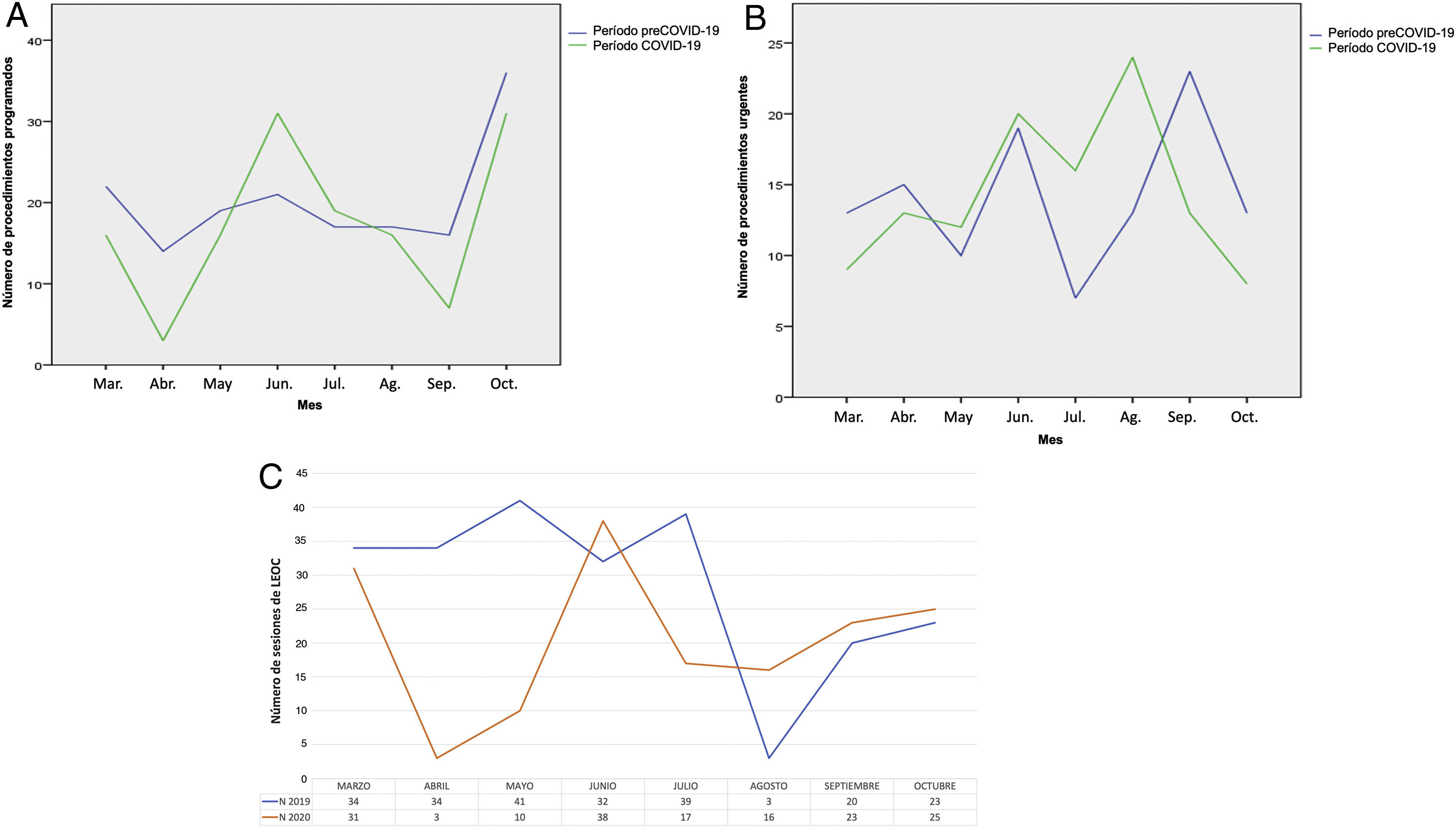
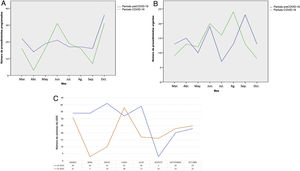
The line charts display the evolution of number of procedures (Fig. 1A: elective, 1B: urgent) during the pandemic period. Table 3 shows laboratory findings in patients who presented with complicated renal colic.
Laboratory findings in patients who presented with complicated renal colic in pandemic and pre-pandemic eras.
| Variable | Pre-COVID-19 period | COVID-19 pandemic period | p |
|---|---|---|---|
| WBC count (/mm3) | 11273.0 (SD 4839.3) | 12600.9 (SD 6569.8) | 0.08 |
| CRP level (mg/L) | 73.2 (SD 86.0) | 85.9 (SD 94.8) | 0.31 |
| Creatinine level (mg/dL) | 1.5 (SD 1.0) | 1.7 (SD 0.7) | 0.07 |
| eGFR by MDRD-4 IDMS (mL/min) | 56.7 (SD 26.1) | 45.4 (SD 20.0) | 0.00* |
P-value marked with bold and asterisk (*) indicate a significant difference.
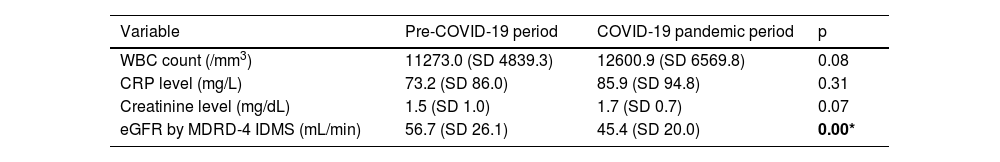
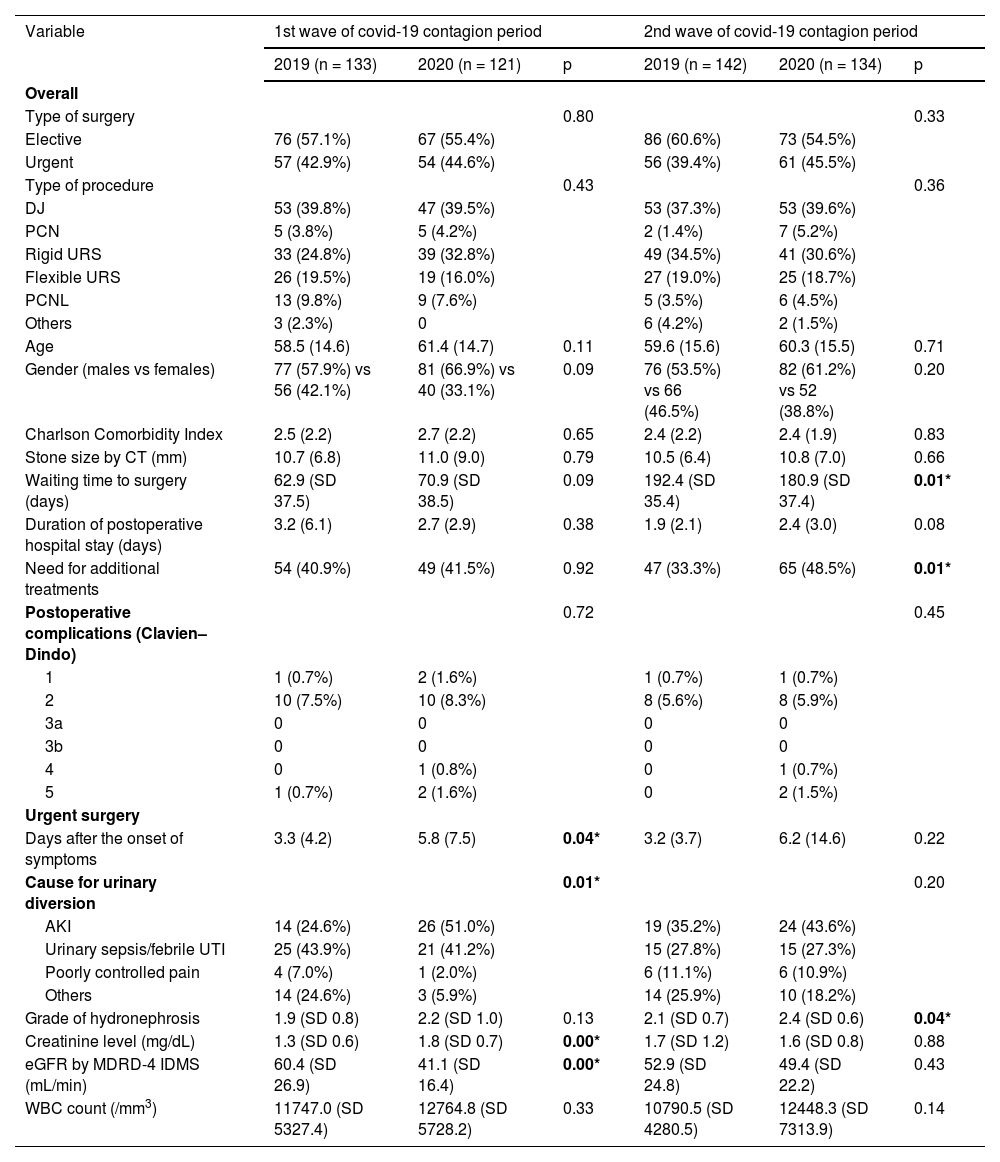
Table 4 contains data broken down into two periods according to pandemic dynamics: 1st and 2nd wave.
Characteristics of patients who underwent urolithiasis procedures in both pandemic and pre-pandemic periods.
| Variable | 1st wave of covid-19 contagion period | 2nd wave of covid-19 contagion period | ||||
|---|---|---|---|---|---|---|
| 2019 (n = 133) | 2020 (n = 121) | p | 2019 (n = 142) | 2020 (n = 134) | p | |
| Overall | ||||||
| Type of surgery | 0.80 | 0.33 | ||||
| Elective | 76 (57.1%) | 67 (55.4%) | 86 (60.6%) | 73 (54.5%) | ||
| Urgent | 57 (42.9%) | 54 (44.6%) | 56 (39.4%) | 61 (45.5%) | ||
| Type of procedure | 0.43 | 0.36 | ||||
| DJ | 53 (39.8%) | 47 (39.5%) | 53 (37.3%) | 53 (39.6%) | ||
| PCN | 5 (3.8%) | 5 (4.2%) | 2 (1.4%) | 7 (5.2%) | ||
| Rigid URS | 33 (24.8%) | 39 (32.8%) | 49 (34.5%) | 41 (30.6%) | ||
| Flexible URS | 26 (19.5%) | 19 (16.0%) | 27 (19.0%) | 25 (18.7%) | ||
| PCNL | 13 (9.8%) | 9 (7.6%) | 5 (3.5%) | 6 (4.5%) | ||
| Others | 3 (2.3%) | 0 | 6 (4.2%) | 2 (1.5%) | ||
| Age | 58.5 (14.6) | 61.4 (14.7) | 0.11 | 59.6 (15.6) | 60.3 (15.5) | 0.71 |
| Gender (males vs females) | 77 (57.9%) vs 56 (42.1%) | 81 (66.9%) vs 40 (33.1%) | 0.09 | 76 (53.5%) vs 66 (46.5%) | 82 (61.2%) vs 52 (38.8%) | 0.20 |
| Charlson Comorbidity Index | 2.5 (2.2) | 2.7 (2.2) | 0.65 | 2.4 (2.2) | 2.4 (1.9) | 0.83 |
| Stone size by CT (mm) | 10.7 (6.8) | 11.0 (9.0) | 0.79 | 10.5 (6.4) | 10.8 (7.0) | 0.66 |
| Waiting time to surgery (days) | 62.9 (SD 37.5) | 70.9 (SD 38.5) | 0.09 | 192.4 (SD 35.4) | 180.9 (SD 37.4) | 0.01* |
| Duration of postoperative hospital stay (days) | 3.2 (6.1) | 2.7 (2.9) | 0.38 | 1.9 (2.1) | 2.4 (3.0) | 0.08 |
| Need for additional treatments | 54 (40.9%) | 49 (41.5%) | 0.92 | 47 (33.3%) | 65 (48.5%) | 0.01* |
| Postoperative complications (Clavien–Dindo) | 0.72 | 0.45 | ||||
| 1 | 1 (0.7%) | 2 (1.6%) | 1 (0.7%) | 1 (0.7%) | ||
| 2 | 10 (7.5%) | 10 (8.3%) | 8 (5.6%) | 8 (5.9%) | ||
| 3a | 0 | 0 | 0 | 0 | ||
| 3b | 0 | 0 | 0 | 0 | ||
| 4 | 0 | 1 (0.8%) | 0 | 1 (0.7%) | ||
| 5 | 1 (0.7%) | 2 (1.6%) | 0 | 2 (1.5%) | ||
| Urgent surgery | ||||||
| Days after the onset of symptoms | 3.3 (4.2) | 5.8 (7.5) | 0.04* | 3.2 (3.7) | 6.2 (14.6) | 0.22 |
| Cause for urinary diversion | 0.01* | 0.20 | ||||
| AKI | 14 (24.6%) | 26 (51.0%) | 19 (35.2%) | 24 (43.6%) | ||
| Urinary sepsis/febrile UTI | 25 (43.9%) | 21 (41.2%) | 15 (27.8%) | 15 (27.3%) | ||
| Poorly controlled pain | 4 (7.0%) | 1 (2.0%) | 6 (11.1%) | 6 (10.9%) | ||
| Others | 14 (24.6%) | 3 (5.9%) | 14 (25.9%) | 10 (18.2%) | ||
| Grade of hydronephrosis | 1.9 (SD 0.8) | 2.2 (SD 1.0) | 0.13 | 2.1 (SD 0.7) | 2.4 (SD 0.6) | 0.04* |
| Creatinine level (mg/dL) | 1.3 (SD 0.6) | 1.8 (SD 0.7) | 0.00* | 1.7 (SD 1.2) | 1.6 (SD 0.8) | 0.88 |
| eGFR by MDRD-4 IDMS (mL/min) | 60.4 (SD 26.9) | 41.1 (SD 16.4) | 0.00* | 52.9 (SD 24.8) | 49.4 (SD 22.2) | 0.43 |
| WBC count (/mm3) | 11747.0 (SD 5327.4) | 12764.8 (SD 5728.2) | 0.33 | 10790.5 (SD 4280.5) | 12448.3 (SD 7313.9) | 0.14 |
P-value marked with bold and asterisk (*) indicate a significant difference.
The number of ESWL sessions has markedly decreased in April and May, as well as July and August, because the growing number of admissions/hospital occupations due to COVID-19 at our institution (Fig. 1C).
Regarding the rate of infection by COVID-19 in surgical patients, we detected a total of 2 cases (0.2%). This included 2 patients in the urgent surgery group who had the infection in the moment of the surgery. None of the elective patients was infected in the moment of surgery or within the 30 days after the procedure. Only one patient had a delay in surgery because of intercurrent COVID-19 infection.
DiscussionSpain was one of the most affected countries in Europe during the 1st wave of COVID-19, and it was also hit hard again by a 2nd wave of COVID-19 infections.8 Our institution is located in Madrid, one of the most affected cities. This city was heavily affected by COVID-19 during March-June 2020 (1st wave).9 This can explain the dynamics of surgical activity and delay in surgeries at our institution and can be extrapolated to countries and cities with similar COVID-19 incidence in current or potential scenarios.
The influence of the pandemic in the urolithiasis management is a relevant issue that must be addressed from an overall perspective, including all aspects of this prevalent disease (urgent and elective management). We need to enhance our understanding of the urolithiasis presentation and management during pandemic times to avoid fatal consequences.
It has been recommended that urologists should closely follow up kidney stone patients and prioritize those who need urgent care.10 Because elective surgeries were temporarily suspended, many procedures had backlogged. In this scenario, urologists had been advised to put the emphasis on the prioritization of patients, maximum efficiency in treatments and the implementation of telemedicine.11 One remarkable aspect in this context is the effort for the identification of high-priority patients. For example, Chen et al. developed a 28-item triage system and proposed a theoretical framework based on obstruction, infection, kidney dysfunction, and other symptoms.12
Medical expulsive therapy (MET) and chemolysis became crucial as a potential way of avoiding surgical interventions. Regarding acute treatment of renal colic, renal decompression in case of analgesic refractory colic pain, concomitant uremia, anuria or threatening urosepsis remains as an urgent procedure.13
Proietti et al. advised to avoid percutaneous nephrostomy in case of need of urgent urinary diversion because of the high risk of dislodgement and delay to subsequent surgical lithotripsy, although there is no consensus. Furthermore, based on their recommendations, whenever possible, the ureteral stent or nephrostomy tube should be placed under local anesthesia to spare ventilators. On the other hand, stent indwelling should be a factor considered in grading the patient priority, due to the fact that the majority of ureteral stents can be left in place for up to 6–12 months. Currently, even though the evidence is insufficient to support antibiotic prophylaxis for patients with indwelling stents, given the likely delays in surgery in the pandemic context, some pulse antibiotic therapy could be considered to reduce the risk of urosepsis.14 These recommendations match well with our real-world data. 11/140 (7.9%) patients undergoing elective surgery during pandemic times had double J incrustation and 5/140 (3.6%) patients presented an intercurrent urinary sepsis during waiting time to surgery, although there were no statistically significant differences between pre- and pandemic periods. Indwelling double J stent removal or exchange was a controversial issue, because some endo-urologists recommend removing, while others recommend postponing.15
It has been proposed that the recent COVID-19 outbreak could lead to a further increase in ESWL use as it avoids a general anesthesia and its potential complications in patients with COVID-19 infection.16 However, the overall number of ESWL sessions in our department decreased during the March-October 2020 period, compared to the same period in 2019 (226 in 2019 vs 163 in 2020), because of the reduction of the number of inpatient beds available. Moreover, anesthesia personnel were totally involved in intensive care unit patients care. Nevertheless, this treatment option is a good alternative that should be considered in pandemic context.
Since the COVID-19 outbreak in March, the numbers of cases dramatically grew and hospital systems were collapsed leading to a delay in surgical treatment of many patients. Nevertheless, we found similar stone characteristics in terms of radiodensity (819.0 -SD 352.5- vs 793.4 -SD 344.8) and stone size by CT (11.5 -SD 6.7- in 2019 vs 12.4 -SD 9.5) with respect to 2019 in the elective surgery group. Mean duration in waiting list was 46.5 (SD 34.6) days in the period of study in 2019 and 72.0 (SD 84.6) days in the same period of 2020. Despite that, types of procedures, operation time, duration of postoperative hospital stay, residual stone fragments and the need for additional treatments were similar to the pre-pandemic period. These data confirmed that there was no an increase of stone burden due to deferral of non-urgent urolithiasis procedures. However, the rate of complications after elective procedures was higher and more serious in the COVID-19 period, especially due to a growth of cases of febrile UTI or urinary sepsis.
According to a non-systematic review of the published recommendations regarding urolithiasis treatment conducted by Abdel et al., during COVID-19 pandemic most of the endo-urologists changed their elective surgical treatment approaches.15 As shown in Fig. 1, after the drop of elective surgeries in April, a rebound was observed in May and June. In contrast to the decreasing number of emergency visits and admissions for stone disease reported by other authors, in our centre the number of urgent procedures for urolithiasis was similar to 2019.
The literature review of Abdel et al. revealed that patients tend to have higher creatinine levels, leukocytosis, increased hydronephrosis grades (grades 3 and 4), and higher incidence of complications compared to non-COVID-19 period.15 Our study corroborates these previous data (see Table 3), except for the differences in CRP and WBC count. We identified a higher number of stage 5 complications in the postoperative period of urgent procedures during COVID times. In particular, 3 (2.6%) patients died due to urinary sepsis in 2020 (versus 1 patient in 2019).
Gul et al. investigated the ureteral stone presentations in a high-volume hospital during the COVID-19 restriction order times. They collected data of 149 patients who were hospitalized due to ureteral stone both during the COVID-19 pandemic restriction period and the same period of the previous year were analysed retrospectively. The mean age and the stone characteristics of the two groups did not differ significantly. WBC counts (12.5 ± 6.5 vs 8.2 ± 4.2) and serum creatinine levels (1.9 ± 1.9 vs 1.2 ± 0.6) were significantly higher in the COVID-19 group. According to the priority classification recommendations of the European Urology Guidelines Office Rapid Reaction Group for urolithiasis applicable during the COVID-19 pandemic, a significant difference was observed between the two periods. In particular, the rate of emergency cases was found more than threefold in the COVID-19 period. The rate of complicated ureteral stone disease significantly increased during the COVID-19 restrictions period.17 Our results showed that the AKI was the main cause for urinary diversion due to urolithiasis (48.1%) in the COVID-period group, meanwhile in the pre-COVID group it was infection (36.0%). However, the number of UTI/urosepsis between the two groups was equal. Our findings share similarities with Metzler et al. These authors pointed out that a higher proportion of COVID-era patients had evidence of AKI based on RIFLE classification (4.7% vs 2.6%) potentially suggestive of a delay in presentation.18 The increase of serum levels of creatinine in patients admitted due to renal colic was also reported by Flammia et al.19.
Liu et al. conducted a study including 376 patients with ureteral stones between 24 January to 24 March 2020 during the COVID-19 outbreak in Beijing and 343 patients during the same period in 2019. Compared with the same period in 2019, the number of patients with ureteral stones was less in Period 1, i.e. 24 January to 24 February, (137 vs 163) but had a rebound phenomenon in Period 2, i.e. 25 February to 24 March, (239 vs 180). The onset time increased in Period 1.20 Our results supported the latter; the mean days to admission after the onset of symptoms was statistically significantly higher in the COVID period (3.3 -SD 4.0- vs 6.1 -SD 11.5-). Liu et al. also noted that the percentage of patients who underwent endoscopy surgery in outbreak period showed no significant difference compared with that in 2019. This is in good agreement with our data.
A retrospective study including 397 patients from 3 institutions from Spain and Italy was performed by Carrion et al. Their results suggest that there were no statistically significant differences between patients presenting after and prior to the national lockdown date in delay in presentation, in serum creatinine level, CRP, WBC count, fever, flank pain, oliguria, hydronephrosis grade and the length of the hospital stay.21 We only found similarity with these authors in the mean hospital stay between the two periods at our institution.
Figures showed an increase of urgent procedures in the period June-August, after the 1st wave, in our centre, maybe because of the delay in urolithiasis treatment and diagnosis (such as imaging or metabolic studies). Furthermore, a resurgence of elective surgeries was observed in May and June. These observations demonstrate the extraordinary adaptation of urologists to the COVID-19 pandemic times. An Italian multicenter analysis of emergency admissions and treatment of upper tract urolithiasis during the lockdown and reopening phases of the COVID-19 pandemic included a total of 516 patients and demonstrated that the number of admissions decreased significantly, by 51% during lockdown compared to 2019 (78 vs 160 admissions). The number of admissions in the reopening phase (May-June 2020) was in line with that in 2019 (n = 138). However, the frequency of hospitalizations, acute obstructive pyelonephritis and complications was significantly higher during lockdown compared to 2019.22 In contrast, our work revealed that the whole number of elective and urgent surgical procedures were similar.
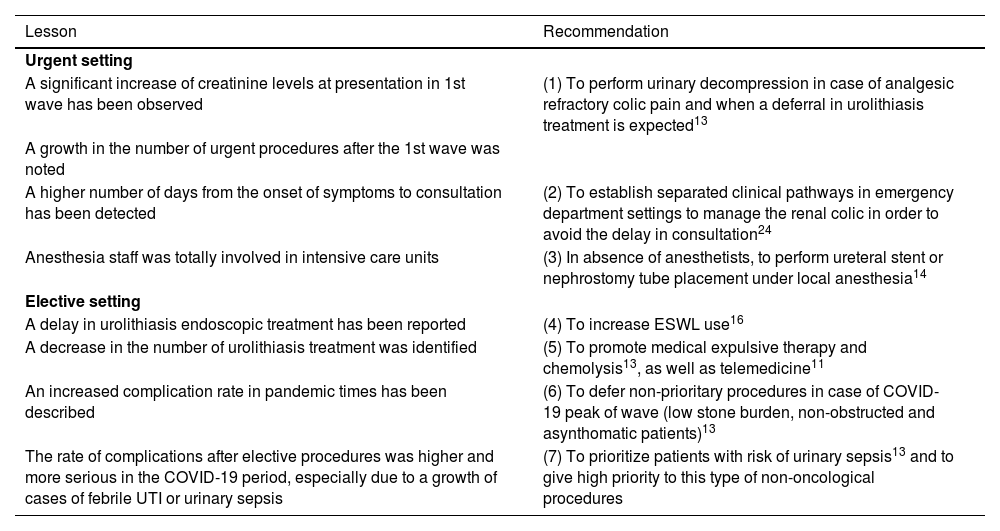
Numerous lessons (summarized in Table 5) have been learned regarding urolithiasis management in these hard times of COVID-19 pandemic. It is crucial to scan the post-coronavirus horizon and analyse the possibilities to avoid complications of urolithiasis in upcoming scenarios and improve the standards of care. Delayed evaluation or treatment for urolithiasis during the COVID-19 pandemic provided a unique opportunity to reassess many well-established stone management strategies.23
Lessons learned from COVID-19 outbreak regarding urolithiasis management and recommendations.
| Lesson | Recommendation |
|---|---|
| Urgent setting | |
| A significant increase of creatinine levels at presentation in 1st wave has been observed | (1) To perform urinary decompression in case of analgesic refractory colic pain and when a deferral in urolithiasis treatment is expected13 |
| A growth in the number of urgent procedures after the 1st wave was noted | |
| A higher number of days from the onset of symptoms to consultation has been detected | (2) To establish separated clinical pathways in emergency department settings to manage the renal colic in order to avoid the delay in consultation24 |
| Anesthesia staff was totally involved in intensive care units | (3) In absence of anesthetists, to perform ureteral stent or nephrostomy tube placement under local anesthesia14 |
| Elective setting | |
| A delay in urolithiasis endoscopic treatment has been reported | (4) To increase ESWL use16 |
| A decrease in the number of urolithiasis treatment was identified | (5) To promote medical expulsive therapy and chemolysis13, as well as telemedicine11 |
| An increased complication rate in pandemic times has been described | (6) To defer non-prioritary procedures in case of COVID-19 peak of wave (low stone burden, non-obstructed and asynthomatic patients)13 |
| The rate of complications after elective procedures was higher and more serious in the COVID-19 period, especially due to a growth of cases of febrile UTI or urinary sepsis | (7) To prioritize patients with risk of urinary sepsis13 and to give high priority to this type of non-oncological procedures |
Many patients with urolithiasis could require management during the COVID-19 pandemic and this is likely to limit surgical procedures to those requiring urgent decompression in the context of obstruction and/or infection.25 MET and chemolysis are two useful management strategies for these patients who do not need for urgent and non-delayable procedures. Additionally, telemedicine represents the cornerstone of urolithiasis management in pandemic times and can effectively reduce the need for visits to outpatient department.
The aim of MET is to facilitate spontaneous passage of ureteral stones. Due to the high likelihood of spontaneous passage of stones lower than 6 mm, MET is less likely to increase the stone-free rate (SFR) but reduces pain episodes.26 Indeed, several trials have established a stone size limit of 3–5 mm, with or without further restriction to patients with distal ureteric stones at diagnosis, to start MET. This subgroup of patients has a spontaneous passage rate of approximately 70% and can most likely benefit from MET.27 This is a strategy to consider in patients during COVID-19 pandemic.
Some recommendations were promoted by different urological associations regarding MET. For example, according the European Association of Urology (EAU), MET can reduce frequency of colic episodes and increase stone expulsion rate after SWL. Furthermore, it appears to be effective in the treatment of patients with ureteric stones amenable to conservative management (mainly those with lower ureteric stones <5 mm). NICE and American Urological Association (AUA) guidelines recommended that MET should be considered in adults, children and young people with distal ureteric stones <10 mm.25 On the other hand, chemolysis represents a good management modality in patients with uric acid stones. The drawback of this approach is the need of dipstick monitoring of urine pH by patients.26
COVID-19 pandemic has caused increased interest in the application of telemedicine in order to minimise the risk of contagion. Connor et al. evaluated the performance of a virtual clinic to assess patients with uncomplicated acute ureteric colic. Thanks to this service, 16% of patients were discharged and only 17% underwent an intervention.28 Regarding the early postoperative evaluation of surgically treated patients, according to Aydogdu et al., telemedicine was associated with high patient and surgeon satisfaction.29 These data support the implementation of telehealth interventions as a feasible and effective strategy in the field of urinary stone disease. In the outpatient setting, in the peak of COVID-19, complementary studies should only be requested if they really have a prognostic or therapeutic significance. Only patients who have to be included in surgical waiting list, or when an assessment of their condition and physical characteristics is necessary, would need in-person care.11
These recommendations were widely implemented in several countries around the world. Jiang et al. retrospectively analysed kidney stone-related discussions on a large social media platform.30 Two remarkable findings of this study during COVID-19 were: (1) opioid-related discussions increased, and (2) MET proliferated beyond its guideline-based indication. The AUA guideline advises urology consultation for procedural intervention for ureteral stones ≥10 mm to avoid upper urinary tract damage that may occur otherwise. Contrary to this recommendation, this study found that the percentage of participants preferring noninvasive management for stones ≥10 mm more than doubled. From pre-COVID-19 to COVID-19, a prominent increase of observation or MET strategies was noted (25% pre vs. 60% during COVID-19).30
This study represents a descriptive analysis from a global perspective of the influence of the pandemic on presentation patterns of urolithiasis and outcomes of elective procedures in this context and between waves. Our study highlighted the detrimental effect of COVID-19 pandemic on the urolithiasis disease.
ConclusionsThe COVID-19 pandemic has impacted on urgent and elective management of urolithiasis, even though an important effort was made to preserve the surgical activity. COVID-19 pandemic represents a challenge for urologists and therefore, lessons should be learned in order to avoid fatal complications.
The authors would like to thank all our colleagues of the Urology Department, who worked tirelessly during the difficult times of the COVID-19 pandemic.