The COVID-19 outbreak has revolutionized several aspects of urological practice, posing new challenges for the management of both inpatient and outpatient activities.1
To cope with the need of social distancing, and in light of the drastic decrease of outpatient clinics, several new strategies implementing telemedicine in response to the pandemic have been warranted.2
This approach was chosen to protect both health personnel and patients from the risk of contagion; as reported by Ladaria Sureda and Pieras Ayala looking at the Spanish situation,3 face-to-face consultations have been cancelled, going to telephone as the most rapid attempt to apply the principles of telemedicine.
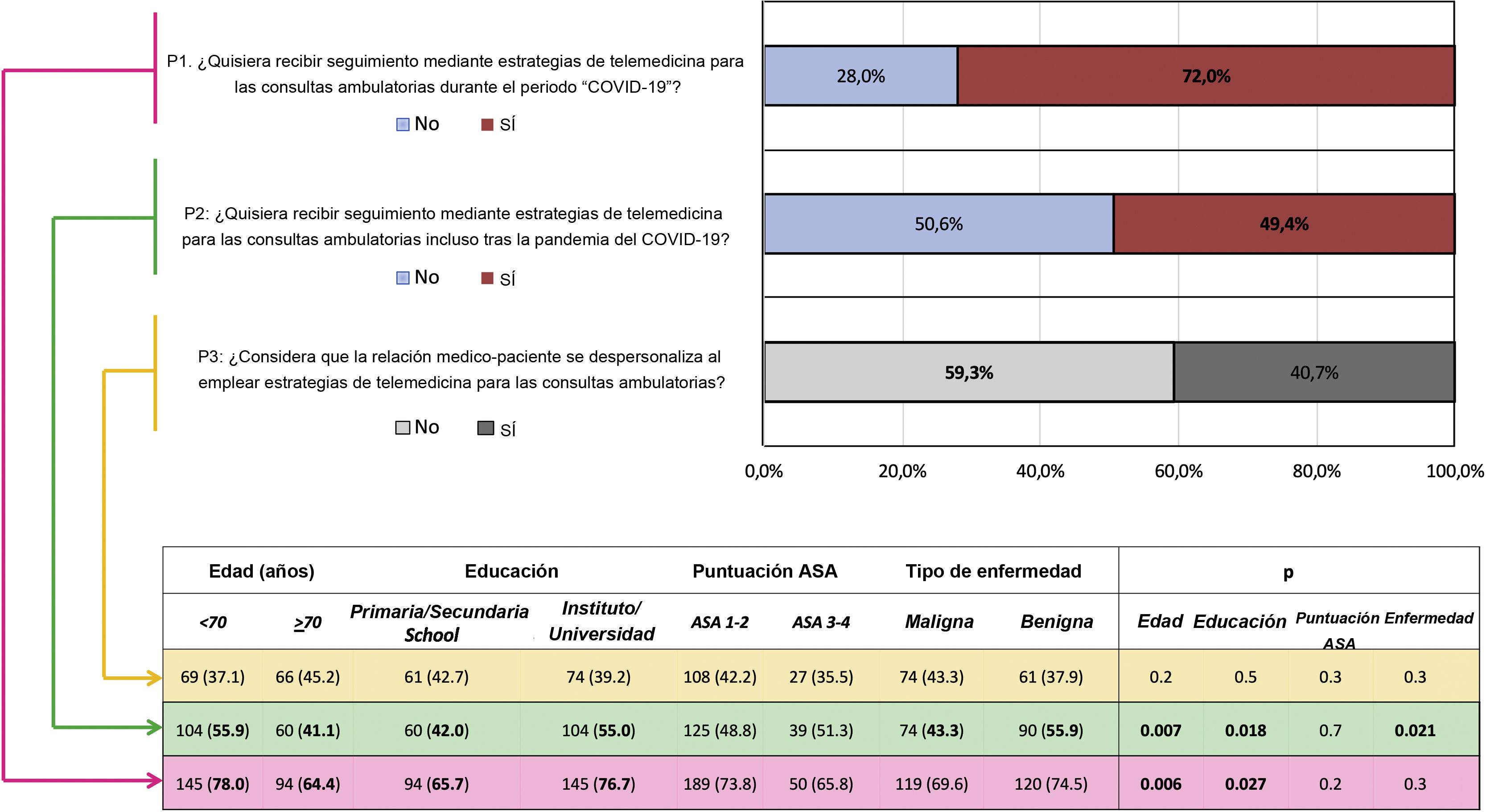
Aiming to evaluate the application of the same strategy in the Italian context, providing patients’ perspectives in this regard, a dedicated questionnaire was administered through structured telephone interviews between 24th and 27th April 2020 to patients who were on the waiting list for elective urological procedures at two Italian Academic referral Centers. Patients were asked the following questions (Q): Would you like to be followed using telemedicine tools (online visits, mobile apps, telephone interviews) for ambulatory visits during (Q1) and after (Q2) the “COVID-19 period”?; Do you feel the doctor-patient relationship “depersonalized” using telemedicine tools for ambulatory visits?(Q3).
Baseline patient characteristics (age, level of education, ASA score and type of disease) and answers were recorded in a dedicated database.
Overall, 332 patients were included in the study. Of these, 51.5% were scheduled for uro-oncologic surgery while 48.5% for benign conditions.
As shown in Fig. 1, 72% of patients reported to appreciate the use of telemedicine for ambulatory visits during the COVID-19 period. Of note, this percentage decreased at 49.4% considering the post-pandemic phase. In line with these findings, 59.3% of them did not perceive the doctor-patient relationship depersonalized using such telehealth tools for ambulatory visits.
Patients’ perspectives on the use of telemedicine for outpatient urological visits. The factors influencing the answers to questions Q1–Q3 are shown in the Table. The potential influence of baseline characteristics on patients’ answers was evaluated by the Pearson Chi-square or Mann-Whitney test, as appropriate. ASA = American Society of Anesthesiologists.
Reading these results in light of the drivers of patients’ answers, it is interesting to notice that younger age and higher education level significantly impacted on the positive opinion of patients regarding telemedicine during the COVID-19 period (P = .006, P = .027). In the post-pandemic phase, also the type of disease influenced the patients’ choice, with patients willing to be followed with telemedicine strategies more often when affected by benign urological conditions than oncologic diseases (P = .021). Finally, none of the baseline patients’ characteristics impacted on their perception about the potential telemedicine-related depersonalization in doctor-patient relationship.
In line with previous reports,1–3 our findings provide a foundation for further implementation of telehealth in the field of Urology not only during emergency scenarios such as the COVID-19 pandemic, but also in the future daily practice.
In a world where the cost-effectiveness of every urological visit is becoming increasingly relevant for both clinicians and policymakers, we should strive to develop as much a possible a value-oriented, patient-centered healthcare. To achieve this goal, reducing waste of human and economic resources, telemedicine strategies should be directed toward all patients for whom “in-person” ambulatory visits may safely spared.
Conflicts of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Amparore D, Campi R, Checcucci E, Piana A, Sica M, Andrea Grosso A, et al. Perspectiva de los pacientes sobre el uso de la telemedicina en las consultas urológicas ambulatorias: aprendiendo de la pandemia del COVID-19. Actas Urol Esp. 2020;44:637–638.