To analyze the results of retrograde intrarenal surgery (RIRS) in patients with ≥2cm stones treated in our center.
Material and methodsA retrospective review of 106 patients with renal calculi underwent RIRS ≥2cm (period January 2009–December 2011). The procedures were performed under general anesthesia as a source of fragmentation using the holmium laser (30W Litho Quantasystem) and flexible ureteroscopes (X2 Flex Storz, Olympus P5) through ureteral access sheaths.
It discusses demographic variables (age, medical history, antiplatelet or anticoagulant treatment, treatment of urolithiasis, BMI, ASA), treated stones variables (size, number, Hounsfield units, biochemical composition) and intra- and postoperative variables (operative time, number of pulses, hospital stay, complications) with the completion of a descriptive analysis of the same.
To define our results we consider success to the complete absence of fragments or residual <5mm posterior imaging tests.
ResultsThe mean stone size was 2.46cm treated, being the only stone in 87.7% of cases. The most frequent location was the renal pelvis stones (44%) followed by the lower calyx (39%). The postoperative complication rate was 6.7%, with all of little relevance. The success rate with a single procedure was 79.4–94.1% with retreatment.
ConclusionRIRS is a valid alternative for the treatment of kidney stones ≥2cm for its high success rate and few complications if performed in specialized centers.
Analizar los resultados de la cirugía retrógrada intrarrenal (CRIR) en pacientes con litiasis ≥2cm tratados en nuestro centro.
Material y métodosRevisión retrospectiva de 106 pacientes con litiasis renales ≥2cm sometidos a RIRS (período comprendido entre enero de 2009 y diciembre de 2011). Los procedimientos se realizaron bajo anestesia general utilizando como fuente de fragmentación el láser Holmium (Litho 30W Quantasystem) y ureteroscopios flexibles (Storz Flex X2, Olympus P5) a través de vainas de acceso ureteral.
Se analizan variables demográficas (edad, antecedentes patológicos, tratamientos antiagregantes o anticoagulantes, tratamiento de litiasis, IMC, ASA), variables de litiasis tratada (tamaño, número, unidades Hounsfield, composición bioquímica) y variables intra y postoperatorias (tiempo quirúrgico, número de pulsos, estancia hospitalaria, complicaciones) con la realización de un análisis descriptivo de las mismas.
Para definir nuestros resultados consideramos éxito la ausencia completa de restos litiásicos o residuales <5mm en las pruebas de imagen posteriores.
ResultadosLa media de tamaño de las litiasis tratadas fue de 2,46cm, siendo la litiasis única en el 87,7% de los casos. La localización más frecuente de la litiasis fue la pelvis renal (44%) seguida del cáliz inferior (39%). La tasa de complicaciones postoperatoria fue del 6,7%, siendo todas de escasa relevancia. El porcentaje de éxito con un único procedimiento fue de un 79,4%, alcanzando el 94,1% con retratamiento.
ConclusiónLa CRIR es una alternativa válida para el tratamiento de litiasis renales ≥2cm por su alta tasa de éxito y escasas complicaciones si se realiza en centros especializados.
Percutaneous nephrolithotomy (PCNL) has until recently been the first-line treatment of kidney stones measuring more than 2cm.1,2 Although PCNL has high rates of kidney stone clearance, the technique has a morbidity and mortality to consider, which can prolong the need for hospitalization.3–5 Recent studies have shown that retrograde intrarenal surgery (RIRS) can be an effective and safer alternative in the treatment of kidney stones of considerable size.6–8
Technological progress, both in the design of new flexible ureteroscopes (thinner and with better vision) and in the extensive variety of endourological materials (ureteral access sheaths, basket extraction, guidewires), coupled with the greater experience of certain surgeons have contributed to the dissemination of RIRS. Thus, the kidney stone clearance rates for patients with kidney stones treated with RIRS have improved, greatly approaching the success rates of PCNL, with less associated morbidity.9,10 The latest review of the clinical guidelines of the European Association of Urology considers endourology as the treatment of choice for kidney stones measuring more than 2cm, with centers with experience in these types of treatments being able to opt between PCNL or CRIR.11
RIRS can be considered a safe alternative to PCNL in cases with significant comorbidity (anticoagulation, cardiopulmonary diseases, advanced age)12 and in individuals with additional adverse anatomical factors (obesity, renal malformations).13
Material and methodsThis was an analytical, descriptive, retrospective study that included 106 patients with the diagnosis of lithiasis ≥2cm, who underwent RIRS in the Hospital of Ribera. The surgical procedure was performed by a single surgeon (JLP) between January 2009 and December 2011.
PatientsAll patients were preoperatively evaluated with urine cultures, preoperative laboratory tests (hemogram, general blood biochemistry, basic coagulation) and computed axial tomography (CT) with volumetric reconstruction for the study of the kidney stone and its relationship with the urinary pathway.
We assessed demographic variables (age, associated comorbidities, renal malformations, previous treatment for lithiasis, anesthetic-surgical risk (ASA), BMI, antiplatelet–anticoagulation), kidney stone variables (location, size, hardness in Hounsfield units [HU], biochemical analysis and number of treated kidney stones) and perioperative and postoperative variables (previously implanted double J stents, surgical time, complications, hospital stay and readmissions).
Surgical techniqueAll procedures were performed with 2 flexible ureteroscope models (URF; Karl Storz Flex X2®, Olympus URF-P5®). All procedures used a safety guide (mixed or nitinol) (Sensor 0.035 straight tip; Boston Scientific®, Hi-wire 0.035; Cook Medical®). Prior to the flexible ureteroscope, an examination of the ureter was performed with a semirigid ureteroscope. This procedure had two purposes: to examine the ureteral anatomy and to detect abnormalities (lack of ureteral distensibility, loops or kinks), which could impede the passage of the sheath and dilation of the intramural ureter, which in turn facilitates the passage of this sheath. Access to the interior of the kidney using the URF was performed for all cases with ureteral access sheaths of various calibers; 12–14F (Re-Trace; Coloplast®) for cases with easy passage of the sheath or previously implanted double-J stents; and 11–13 (Navigator; Boston Scientific®) or 9.5–11F (Flexor; Cook Medical®) for cases with less accommodating ureters. The source for the Holmium laser fragmentation was 30W Litho (Quantasystem®) with 270 or 400μm fibers depending on the active deflection requirements of the URF. We only used nitinol baskets for cases in which obtaining a sample of the kidney stone for biochemical study was imperative and in those cases in which, after reducing the size of the kidney stone, the residues were moved to a more comfortable position to complete its fragmentation (kidney stones located in lower calyx).
Postoperative follow-upWe classified the postoperative complications according to the Clavien classification system. For the postoperative evaluation of the results of the procedure, a simple radiodiagnosis was performed for cases of lithiasis 4–6 weeks after the surgery as well as renal ultrasonography at 3 months. For cases of radiolucent lithiasis or large residual stone burden after surgery, we performed unenhanced CT scans 6 weeks after the surgery.
The surgery (RIRS) was considered a success if there was no residual lithiasis or if the residues measured in the control test had diameters less than 5mm.
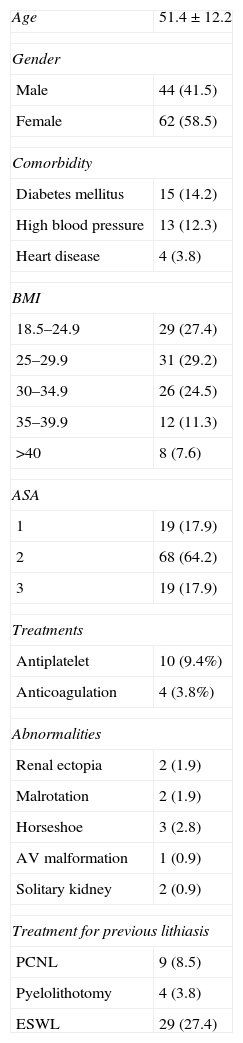
ResultsWe report the results of 106 cases of RIRS for kidney stones measuring ≥2cm. The patients’ mean age was 51.5 years (23–78). Around 43.4% of the patients had some degree of obesity. There was a history of previous treatments for lithiasis in 11.3% of the cases (8.5% extracorporeal shock wave lithotripsy and 2.8% PCNL), which had not resolved the case, and 8.4% presented some type of abnormal renal anatomy. The patients’ demographic data are listed in Table 1.
Demographic characteristics.
| Age | 51.4±12.2 |
| Gender | |
| Male | 44 (41.5) |
| Female | 62 (58.5) |
| Comorbidity | |
| Diabetes mellitus | 15 (14.2) |
| High blood pressure | 13 (12.3) |
| Heart disease | 4 (3.8) |
| BMI | |
| 18.5–24.9 | 29 (27.4) |
| 25–29.9 | 31 (29.2) |
| 30–34.9 | 26 (24.5) |
| 35–39.9 | 12 (11.3) |
| >40 | 8 (7.6) |
| ASA | |
| 1 | 19 (17.9) |
| 2 | 68 (64.2) |
| 3 | 19 (17.9) |
| Treatments | |
| Antiplatelet | 10 (9.4%) |
| Anticoagulation | 4 (3.8%) |
| Abnormalities | |
| Renal ectopia | 2 (1.9) |
| Malrotation | 2 (1.9) |
| Horseshoe | 3 (2.8) |
| AV malformation | 1 (0.9) |
| Solitary kidney | 2 (0.9) |
| Treatment for previous lithiasis | |
| PCNL | 9 (8.5) |
| Pyelolithotomy | 4 (3.8) |
| ESWL | 29 (27.4) |
Data presented as number of patients and the percentage within parentheses or as the mean±standard deviation.
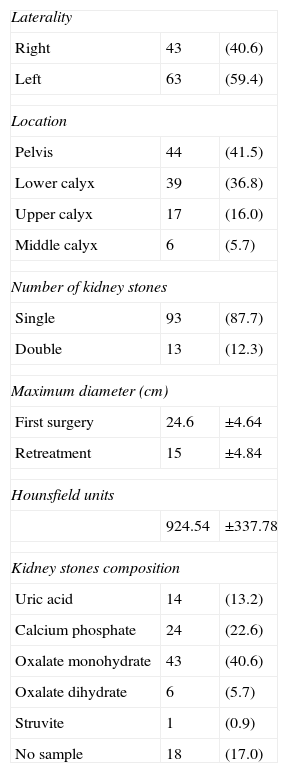
The characteristics of the kidney stones appear in Table 2. The mean size of the kidney stones was 2.46cm (radius, 20–40mm). The mean hardness was 924HU (849–999.71HU). In terms of the location, 41.5% of the kidney stones were found in the renal pelvis, and a high percentage (36.8%, 39 cases) were found in the lower calyceal group. The most common biochemical composition was calcium oxalate (48.9%). The variables related to the kidney stones are shown in Table 2.
Characteristics of the lithiasis.
| Laterality | ||
| Right | 43 | (40.6) |
| Left | 63 | (59.4) |
| Location | ||
| Pelvis | 44 | (41.5) |
| Lower calyx | 39 | (36.8) |
| Upper calyx | 17 | (16.0) |
| Middle calyx | 6 | (5.7) |
| Number of kidney stones | ||
| Single | 93 | (87.7) |
| Double | 13 | (12.3) |
| Maximum diameter (cm) | ||
| First surgery | 24.6 | ±4.64 |
| Retreatment | 15 | ±4.84 |
| Hounsfield units | ||
| 924.54 | ±337.78 | |
| Kidney stones composition | ||
| Uric acid | 14 | (13.2) |
| Calcium phosphate | 24 | (22.6) |
| Oxalate monohydrate | 43 | (40.6) |
| Oxalate dihydrate | 6 | (5.7) |
| Struvite | 1 | (0.9) |
| No sample | 18 | (17.0) |
Data presented as number of patients and the percentage within parentheses or as the mean±standard deviation.
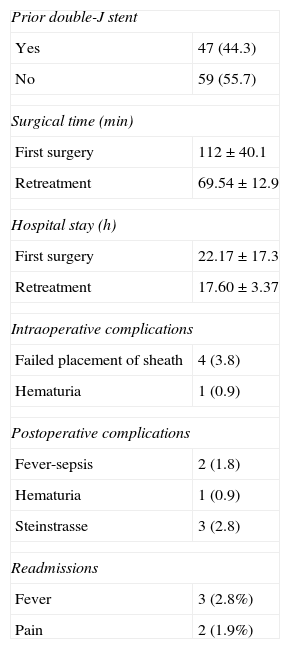
In 47 cases (44.3%), the patients had double-J stents prior to the surgery, either for past treatments or for needs prior to the surgery (symptomatic lithiasis, dilation or functional delay in the preoperative CT study). The mean surgical time was 112min (104.26–119.74), with a mean hospital stay of 16h. Some 4.7% of the patients experienced perioperative complications: blocked passage of the ureteral sheath (4 cases; 3.77%) and poor visibility due to hematuria in 1 case. Only 6.7% of the patients experienced postoperative complications: fever or sepsis with no organ dysfunction (2 cases), hematuria (1 case) and 3 patients with steinstrasse, which required simple ureteroscopy to release the blockage. These complications can be grouped as Clavien I, II and IIIa. Hospital readmission occurred in 4.7% of the cases due to fever and pain. The perioperative data are listed in Table 3.
Perioperative Data.
| Prior double-J stent | |
| Yes | 47 (44.3) |
| No | 59 (55.7) |
| Surgical time (min) | |
| First surgery | 112±40.1 |
| Retreatment | 69.54±12.9 |
| Hospital stay (h) | |
| First surgery | 22.17±17.3 |
| Retreatment | 17.60±3.37 |
| Intraoperative complications | |
| Failed placement of sheath | 4 (3.8) |
| Hematuria | 1 (0.9) |
| Postoperative complications | |
| Fever-sepsis | 2 (1.8) |
| Hematuria | 1 (0.9) |
| Steinstrasse | 3 (2.8) |
| Readmissions | |
| Fever | 3 (2.8%) |
| Pain | 2 (1.9%) |
Data presented as number of patients and the percentage within parentheses or as the mean±standard deviation.
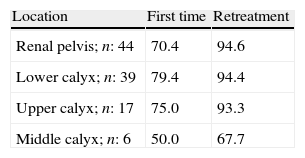
Table 4 shows the proportion of success with the first and second procedures. After the first procedure, a 73.6% success rate was achieved; after the second procedure, the overall success rate was 93.5%. The success rates after the first and second procedure for lithiasis in the lower calyceal group was 79.4% and 94.4%, respectively.
DiscussionFlexible ureterorenoscopy and laser fragmentation of renal lithiasis has progressed and has become an effective and minimally invasive technique for the treatment of this condition.1,2,14,15 Furthermore, we should consider that complications resulting from percutaneous nephrolithotomy have been reported in 20.5% of cases in most published series on this subject within the CROES group, with major complications (Clavien grade II or higher) representing 9.48% of the cases.16 In contrast, the analysis by Aboumarzouk et al.6 estimated the aggregate of RIRS complications at 10%, the majority of which are minor if adjusted to this classification, which the authors do not do in their study.
Therefore, the RIRS has gone from not fitting within the clinical guidelines of the UAE to a first-level alternative in the treatment of kidney stones measuring ≥2cm in the latest review of their 2012 Clinical Guidelines.1,11 The current reality for the results of this type of treatment shows that it is possible to achieve lithiasis elimination rates above 90%, according to a meta-analysis on contemporary studies published on the subject.6 The importance of this study, in relation to that published in the reviewed literature, is determined by the number of cases of this condition, the success rate achieved and the scarcity of complications.
The most extensive series published in the literature was the multicenter study by Hyams et al.7 that included 120 cases, followed by the series by at-Qahtani et al.,14 which included 104 cases at the Tennon University Hospital of Paris. Compared to these 2 studies, our site has performed 106 cases in the period between January 2009 and December 2011.
An important fact when comparing our results with those of the large published series is the fact that the primary variables, such as the mean size of the kidney stones, surgical time and rate of retreatment, are similar to those of these series. In our series, the mean size obtained was 2.46cm, which is similar to that of Hyams6 and that obtained in the meta-analysis by Aboumarzouk6 and significantly smaller than that of at-Qahtani.14 In terms of surgical times, the mean was 112min, which was significantly higher than that of centers with greater experience (89.1min), as is the case with Tennon University Hospital. In our case, the rate of retreatment was 1.7, which is in line with studies published in the literature.6,8,14
Another issue to consider when assessing these results is the systematic use of sheaths (100% of the cases), in line with other recent references. We agree that this use facilitates and protects the passage of the flexible ureteroscope, reduces the intrarenal pressure over the course of the surgery and is in part a mechanism for protecting the ureter.6,9,10 The passage of the sheath can become a factor that conditions the decision whether or not to perform the surgery. There are authors in the literature who advocate the placement of a double-J stent prior to the surgery to ensure the passage of the ureteral sheath.17 In our experience, we do not consider this necessary based on the low rate of sheath placement failure (3.77%) and the discomfort that endoscopy prior to the surgery causes the patient, along with the discomfort from the catheter. Although it has not been analyzed due to the considerable number of variables that would enter into play, prior semirigid ureteroscopy that dilates the intramural ureter and provides direct vision of the ureter (as well as having sheaths of various calibers) ensures a lower proportion of nonperformance due to a lack of ureteral access by the sheath.
In our study, we defined success as the absence of lithiasis or residual kidney stones measuring less than 5mm in the radiological controls after the surgery. It is important to note that when we established this cutoff at the start of our series in 2009, there was no consensus in the literature on this subject. There is still no consensus because there are authors who consider success to be sizes below 2mm9,14,18; however, other authors, such as Hyams et al.,7 place success at 4mm.
The results of our series support RIRS as an effective and safe technique for the treatment of kidney stones ≥2cm. The analysis of the results revealed success rates of 73.6% (for a single procedure) and 93.4% for retreatment. These results are similar to those of other authors, such as Alqahtani (96.7%)14, Hyams et al. (97.5%)7 and Breda.10 An important fact to consider is that a number of authors in the literature have reported their overall results without listing the rates of retreatment, such as the case of Hyams et al. However, based on the meta-analysis by Aboumarzouk,6 which lists a mean retreatment rate in the analyzed series of 1.6; our series is close to this result with a rate of 1.7. In terms of postoperative complications, the overall rate was low (6.7%). If we adjust the complications to the Clavien classification system, they would correspond to grades I, II and IIIa, if we consider the formation of steinstrasse that requires instrumentation for its treatment as a complication, as in other studies.6 In this respect, our series conforms to the results of the major series that achieved a mean overall percentage of complications of 10%,6 although this study was not adjusted to the Clavien classification system.
Although the measurement of factors that determine the success of treatment was not the purpose of this study, it does seem that the size of the kidney stone was important.6,14 In our study, we did not perform an analysis by subgroups of size; we cannot, therefore, make any conclusions about this aspect. We observed that the location seemed to have no relevance to the success of the procedure, given that the results by location (pelvis, lower and upper calyceal groups) were similar and ranged from 93% to 94.1%.
Few studies have jointly analyzed the results of PCNL and RIRS for kidney stones measuring ≥2cm.19,20 However, the positive results of the CRIR series6 in these cases and the low rate of severe complications has consolidated this technique as an alternative to PCNL in these cases.11 It remains to be determined whether the costs attributed to the maintenance of flexible ureteroscopes compensate the lower need for hospitalization and the fewer complications of RIRS compared with PCNL. A number of studies have analyzed this issue and advocated for the lower cost of CRIR21; however, there are few references on the issue, and this analysis depends on numerous factors that cannot be extrapolated to each particular healthcare setting.
One of the limitations of our study is the fact that it is a retrospective analysis. Despite being retrospective, the low rate of complications and the high success rates oblige us to reflect on this technique as a current alternative to PCNL. Another of the study's limitations was the use of different imaging techniques to assess the kidney stones residues. Although CT has the highest sensitivity for detecting residual fragments, its cost prevents us from performing it on all patients in standard practice.22 The radiation dosage from this test should also be considered, given that these patients are eventually exposed to larger future doses due to the recurrent character of the disease. In defense of RIRS, this technique requires precision to assess residual lithiasis that the other techniques, such as extracorporeal lithotripsy and PCNL, do not demand (in standard practice we do not assess the results of ESWL and PCNL with CT for all our patients). Further randomized studies are needed on the postoperative management of residual fragments to clarify and unify protocols, because unfortunately there is no consensus and the follow-up in the literature varies significantly.23
ConclusionWith these results, we can conclude that RIRS with Holmium laser lithotripsy for the treatment of kidney stones ≥2cm is a safe and effective procedure and should be considered as an alternative to PCNL in these cases. Prospective studies are needed to establish postoperative control strategies and unify success criteria to provide greater strength to these conclusions.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Palmero JL, Castelló A, Miralles J, Nuño de La Rosa I, Garau C, Pastor JC. Resultados de la cirugía retrógrada intrarrenal en el tratamiento de litiasis renales mayores de 2cm. Actas Urol Esp. 2014;38:257–262.