Tuberculous aortitis is a rare entity first described by Weigert in 1882.
ReportA 73-year-old male under regular imagiologic surveillance due to a 4cm abdominal aortic aneurysm, was referred to our department for suspected contained rupture. He was asymptomatic and his CT scan showed an inflammatory mass surrounding the aneurysm. During elective conventional surgery, aneurysm wall infiltration and adenopathies were identified. The histological analysis was compatible with tuberculosis. Eight months after surgery the patient is well, under tuberculostatic therapy.
ConclusionThe combination of surgical treatment and long duration tuberculostatic therapy is the best treatment option for tuberculous aortitis.
A aortite tuberculosa é uma entidade rara inicialmente descrita por Weigert em 1882.
ReportUm homem de 73 anos, sob controlo imagiológico regular por aneurisma da aorta abdominal de 4cm de diâmetro, foi referenciado ao Departamento por suspeita de ruptura contida. O doente estava assintomático e a Angio-TC evidenciava uma massa inflamatória envolvendo o aneurisma. Durante a cirurgia electiva convencional, infiltração da parede do aneurisma e adenopatias foram identificadas. A análise histológica era compatível com tuberculose. Oito meses após a cirurgia, o doente encontra-se estável e sob terapêutica tuberculostática.
ConclusãoA associação entre tratamento cirúrgico e terapêutica tuberculostática de longa duração é a melhor opção terapêutica para os casos de aortite tuberculosa.
Tuberculous aortitis was first described by Weigert in 18821 and constitutes an extremely rare entity, with less than 100 reported cases, but fatal if undiagnosed.
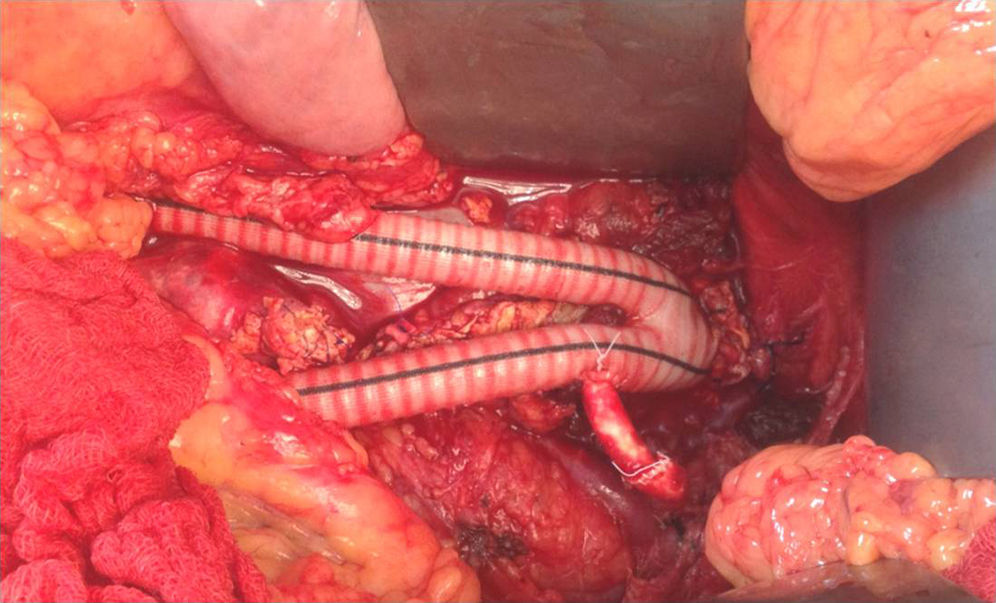
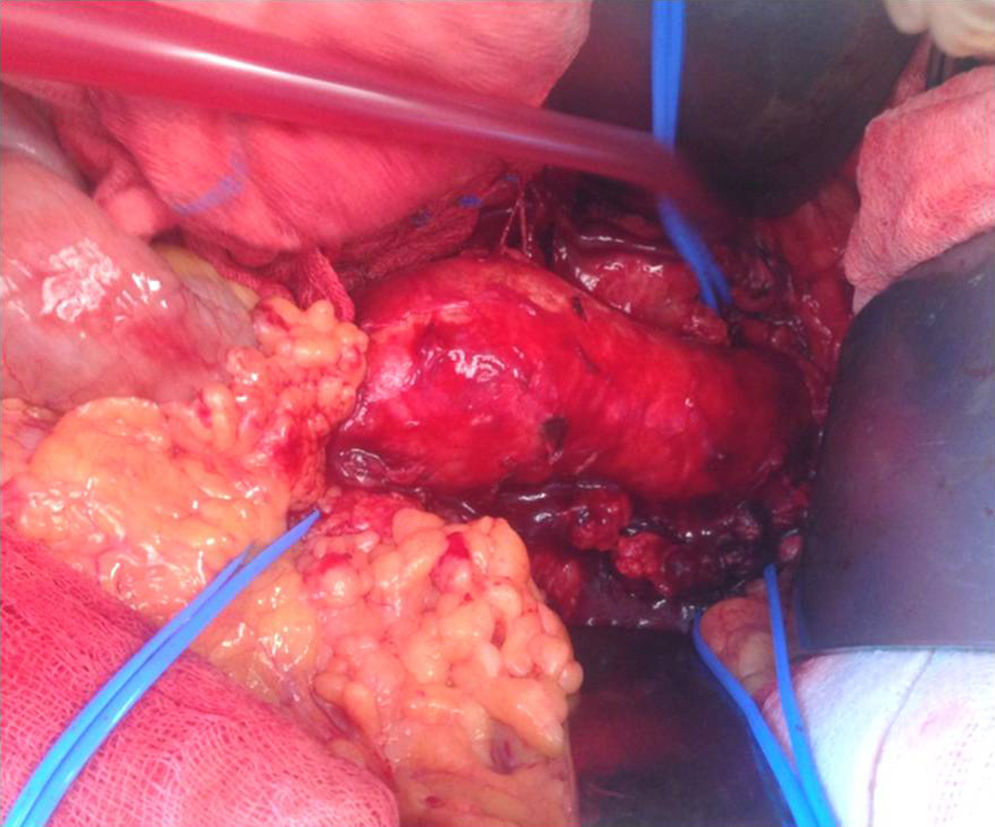
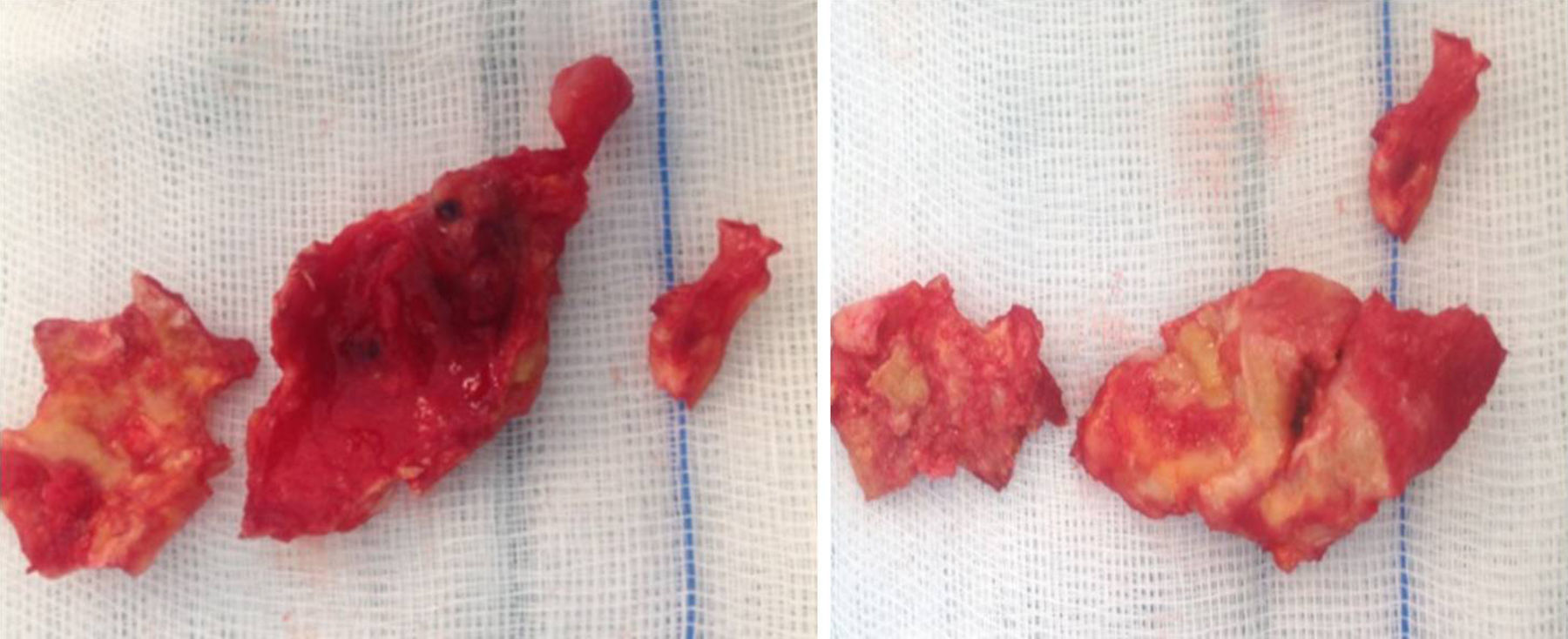
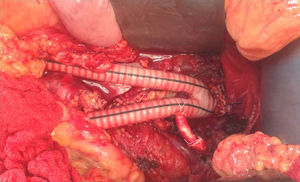
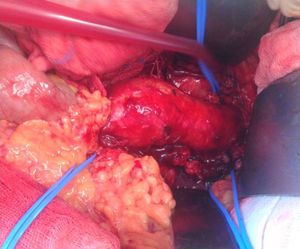
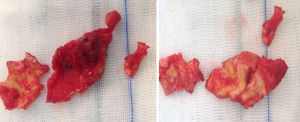
Case reportA 73 year old male, with smoking habits, ischemic cardiopathy and hypertension, was the subject of regular imagiologic surveillance due to a 4cm pararenal abdominal aortic aneurysm. He was taken to the emergency department after routine CT examination for suspected contained aneurysm rupture. The Angio-CT was repeated and an inflammatory mass surrounding the aneurysm was identified, which enclosed the left renal artery ostium, without any signs of rupture (Fig. 1). This inflammatory mass was not described in the previous CT scans the patient had been submitted to. The patient denied previous Tuberculosis infection as well as having had fever, shivers or abdominal pain prior to admittance, referring a 10kg weight loss during the previous year. The laboratory analysis did not present any relevant changes or increased inflammatory parameters and the blood cultures and serologies were negative. He was submitted to elective surgery. Under supra-renal clamping the aneurysm was partially resected and, using a bifurcated Dacron graft, an aorto-bifemoral interposition and a bypass to the left renal artery done (Fig. 2). The aneurysm's intraoperative appearance was that of an inflammatory aneurysm (Fig. 3), no abscess or fluid collection was identified. Several tissue samples were sent to histopathological analysis (Fig. 4), including aneurysm wall fragments which had been infiltrated by the inflammatory mass and grayish adenopathies. The patient was discharged 8 days after the surgery, without any complications having taken place. The histological analysis of the samples revealed aspects compatible with tuberculosis (acid and alcohol-fast bacilli were not identified), the patient was referred to the Pneumologic Diagnostic Center and is at the moment under tuberculostatic therapy, doing well at eight months follow-up.
Intra-operative appearance, compatible with an inflammatory aneurysm. The inflammatory mass involved the left renal artery and grayish adenopathies were evident. The left renal artery, the right renal artery and the inferior mesenteric artery were isolated and identified by a blue Silastic® band.
The majority of tuberculous mycotic aneurysms are saccular (98%) and false (88%), and the aorta is the most frequently affected vessel, being the abdominal and the descending thoracic locations preferential.1 The size of the aneurysm does not dictate the need for surgery as the rate of the destruction of the aortic wall is unpredictable.1,2
Most tuberculous aortitis occurs due to direct extension of the infection from a contiguous focus, either lymph node, paraspinal abscess or adjacent organ tissue; direct implantation of circulating bacilli on the vessel's wall is another possible mechanism. Identifying the precursor event, either the aortitis or the adjoining infected tissue, especially when tuberculosis lymphadenitis is present, is challenging.1 What distinguishes our patient from the previous case studies is the fact that it is the first report, to our knowledge, of tuberculosis infection of a preexisting aortic aneurysm.
In the long series, over one third of patients did not have a tuberculosis diagnosis before surgery. A high suspicion rate is therefore mandatory, especially in an era of increasing immunocompromised conditions which might lead to an increase of this life-threatening condition.3 As it is a rare entity, the recognition of tuberculous mycotic aneurysm is problematic. The possibility of a tuberculosis infection may not have been anticipated, the intra-operative appearance of the aneurysm could be uncharacteristic and the surgical decision process is in many instances that of an inflammatory aneurysm or a mycotic aneurysm caused by a more common pathogen,1 as in our case.
The treatment for tuberculous aortitis must be an association of medical and surgical therapy, as no patients survived with either of them on its own.1 Surgical therapy allows for debridement and excision of the infected tissues, improving antimycobacterial action, and should be the first choice if allowed by the patient's condition. A few reports of endovascular therapy have emerged, in patients with high surgical risk, with mixed results.4 Controversy exists, however, on the duration of medical treatment, some authors defend long duration, or even lifelong tuberculostatic treatment, to prevent prosthetic infection and the development of false anastomotic aneurysms.5 In fact, leaving a vascular prosthesis on a potentially infected field does not seem to adversely outcome as long as medical treatment is maintained; the cases of aortic rupture after treatment reported happened after tuberculostatic drugs had been suspended.3–5 The initial antituberculous therapy regimen should last for no less than 9–12 months. The decision of performing a long term antimicrobial treatment, as well as the drug combination and its duration, should be taken bearing in mind the presence of in situ prosthetic aortic graft, as well as the pattern of tuberculostatic resistance identified on the cultures.2,3
ConclusionTuberculous mycotic aneurysms are very rare and the combination of surgical treatment and long duration tuberculostatic therapy is the best treatment option, with the best long term results.1,3
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.