Ventricular fibrillation (VF)-related sudden cardiac death (SCD) is a leading cause of mortality and morbidity. Current biological and imaging parameters show significant limitations on predicting cerebral performance at hospital admission. The AWAKE study (NCT03248557) is a multicentre observational study to validate a model based on spectral ECG analysis to early predict cerebral performance and survival in resuscitated comatose survivors.
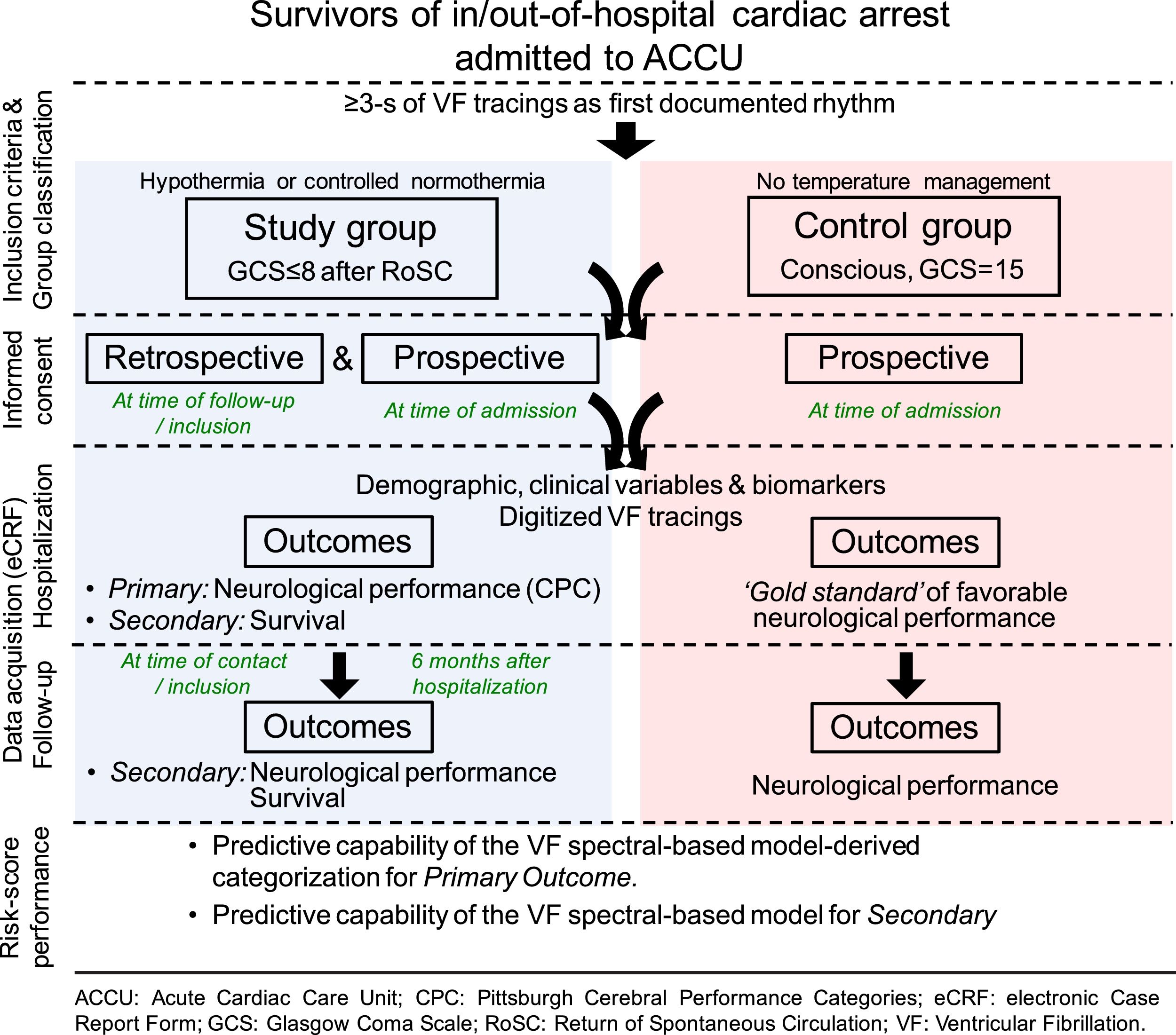
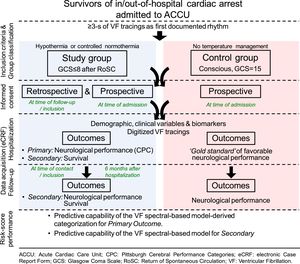
MethodsData from VF ECG tracings of patients resuscitated from SCD will be collected using an electronic Case Report Form. Patients can be either comatose (Glasgow Coma Scale – GCS – ≤8) survivors undergoing temperature control after return of spontaneous circulation (RoSC), or those who regain consciousness (GCS=15) after RoSC; all admitted to Intensive Cardiac Care Units in 4 major university hospitals. VF tracings prior to the first direct current shock will be digitized and analyzed to derive spectral data and feed a predictive model to estimate favorable neurological performance (FNP). The results of the model will be compared to the actual prognosis.
ResultsThe primary clinical outcome is FNP during hospitalization. Patients will be categorized into 4 subsets of neurological prognosis according to the risk score obtained from the predictive model. The secondary clinical outcomes are survival to hospital discharge, and FNP and survival after 6 months of follow-up. The model-derived categorisation will be also compared with clinical variables to assess model sensitivity, specificity, and accuracy.
ConclusionsA model based on spectral analysis of VF tracings is a promising tool to obtain early prognostic data after SCD.
La muerte súbita (MS) por fibrilación ventricular (FV) es una importante causa de morbilidad y mortalidad. Los métodos biológicos y de imagen actuales muestran limitaciones para predecir el pronóstico cerebral al ingreso hospitalario. AWAKE es un estudio observacional, multicéntrico, con el objetivo de validar un modelo basado en el análisis espectral del electrocardiograma (ECG), que predice precozmente el pronóstico cerebral y la supervivencia en pacientes resucitados y en estado de coma.
MétodosSe recogerán datos de los ECG con FV de pacientes reanimados de MS. Los pacientes pueden ser tanto supervivientes en estado de coma (Glasgow Coma Scale [GCS]≤8) sometidos a control de temperatura tras la recuperación de circulación espontánea (RCE), como aquellos que recuperan la consciencia (GCS=15) tras RCE; todos ellos ingresados en unidades de terapia intensiva cardiológica de 4 hospitales de referencia. Los registros de FV previos al primer choque se digitalizarán y analizarán para obtener datos espectrales que se incluirán en un modelo predictivo que estime el pronóstico neurológico favorable (PNF). El resultado del modelo se comparará con el pronóstico real.
ResultadosEl objetivo principal es el PNF durante la hospitalización. Los pacientes se categorizarán en 4 subgrupos de pronóstico neurológico según la estimación de riesgo obtenida en el modelo predictivo. Los objetivos secundarios son supervivencia al alta hospitalaria, y PNF y supervivencia a los 6 meses. El resultado de este modelo también se comparará con el pronóstico según variables clínicas.
ConclusionesUn modelo basado en el análisis espectral de registros de FV es una herramienta prometedora para obtener datos pronósticos precoces tras MS por FV.
Sudden cardiac death (SCD) causes one-fourth of all cardiovascular mortality worldwide,1 and ventricular fibrillation (VF) is the most commonly associated arrhythmia with such a fatal event.2 Survival to hospital admission is rarely higher than 65%,1,3,4 and up to 50% of these patients may remain with neurological damage after hospital discharge.4 Central temperature control, either by mild therapeutic hypothermia (32–34°C) or controlled normothermia (36°C) is the only treatment that has proven to improve neurological outcomes in comatose patients resuscitated from VF-related cardiac arrest and return of spontaneous circulation (RoSC).4–7 Prognosis is currently estimated using a combined strategy with clinical data, serum biomarkers, electroencephalogram, somatosensory evoked potentials and brain imaging.4 Nevertheless, none of these parameters by itself has demonstrated to predict reliably neurological outcomes, even when deferred up to 7 days after the event. Moreover, temperature control during the first 24h further complicates an early neurological evaluation due to sedation and a higher rate of misleading biomarker values within the first 48h.8
Back in the 80s, survival after cardiac arrest due to VF was related to the type of VF waves at resuscitation; thus, ‘fine VF’ (fibrillatory waves <0.2mV) was associated with higher mortality,9 while wave amplitudes >0.5mV were associated with higher survival rates and greater success after a direct current (DC) shock.10 However, VF amplitude values from surface ECG leads are subject to important limitations like changes in transthoracic impedance (e.g. obesity), electrode placement and contact, or artifacts (e.g. chest compressions)11; all commonly present during resuscitation. In fact, recent data have shown the futility of surface VF wave amplitudes as predictor of neurological damage.12
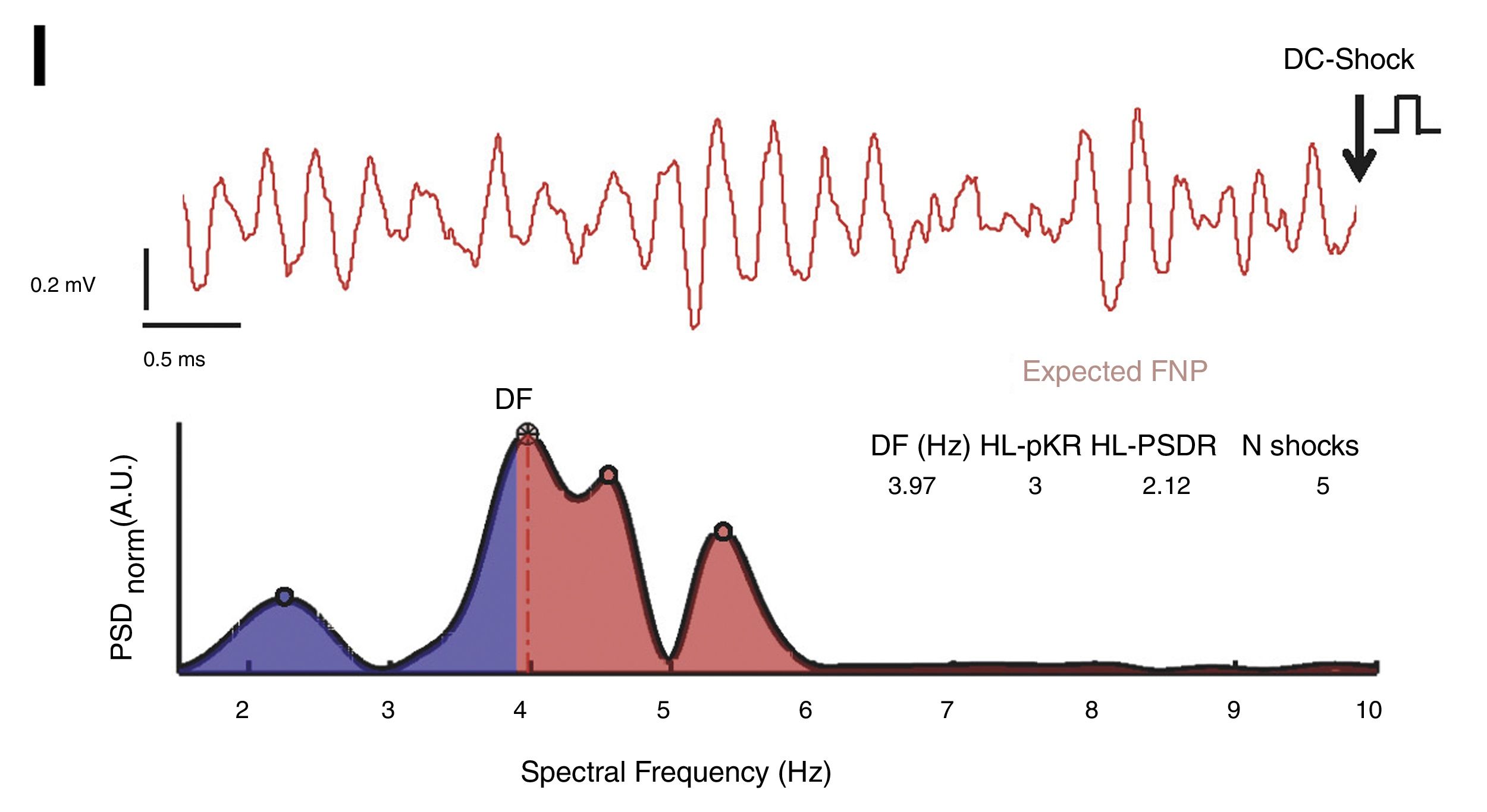
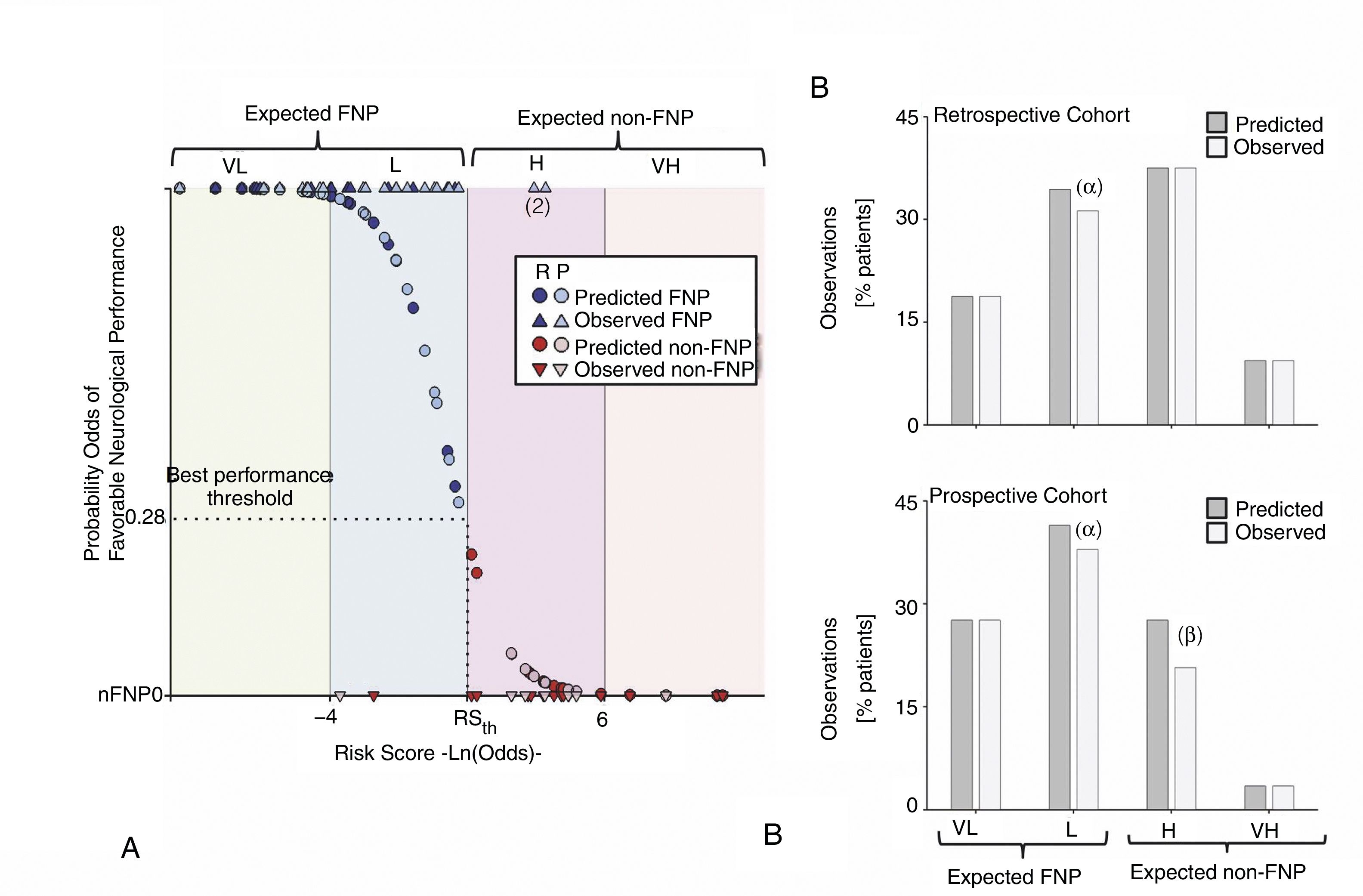
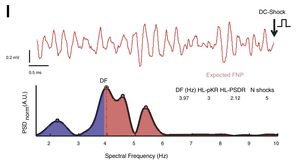
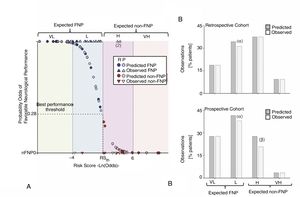
More relevant and robust is an approach based on waveform analysis during VF to obtain spectral parameters that enable to estimate both the time in VF and clinical outcomes as neurological performance and survival.12–15 Interestingly, as the VF episode lasts, progressive myocardial ischemia leads to gradual decline in VF spectral values.15–18 Moreover, we have recently suggested that such a decline reflects accurately the degree of acute cerebral injury as a consequence of time in VF and concomitant myocardial ischemia.12 Briefly, we studied a single center retrospective cohort of comatose patients (≤8 score in the Glasgow Coma Scale, GCS) resuscitated from SCD due to VF. All patients underwent therapeutic hypothermia to minimize post-reperfusion brain damage. Multivariate analysis identified 3 VF spectral variables (dominant frequency – DF – of the VF spectrum, high-to-low power spectral density ratio – HL-PSDR – as the relative power between high and low frequency bands with a cut-off at 3.9Hz, and high-to-low peak ratio – HL-pKR – as the relative number of spectral peaks above and below the 3.9Hz threshold with power above 40% the frequency with the highest power) and 1 clinical variable (number of defibrillation shocks delivered before RoSC) that enable to predict both neurological performance and survival with high sensitivity and specificity (≥0.94).12Fig. 1 shows a sample case with calculation of predictive spectral variables. The model-derived risk score was validated in a single center and small prospective cohort, preserving high sensitivity and specificity (≥0.88) (Fig. 2).12 Other series have also shown the potential value of VF spectral variables to predict clinical outcomes.14,19–21 However, these series show important limitations as they do not distinguish between patients with or without comatose status on admission or do not provide information about post-cardiac arrest care using mild hypothermia,14,20 or even do not consider neurological performance as an outcome.19 It is also often seen in previous series that spectral analysis is limited to a single spectral parameter without comparisons with other parameters that might perform better.14,20
Representative VF recording and spectral-derived predictive variables. Upper panel, digitized tracing before the first DC shock. Lower panel, representative spectrum of the VF signal. Blue-filled and red-filled spectra show low (1.5–3.9Hz) and high spectral bands (3.9–10Hz), respectively. The DF peak (3.97Hz), HL-PSDR (2.12), HL-pKR (3) and the number of shocks delivered before RoSC (5) correctly classified such a case within low risk of non-favorable neurological performance. DF: dominant frequency; FNP: favorable neurological performance; HLPSDR: high-to-low power spectral density ratio; HL-pKR: high-to-low peak ratio; RoSC: return of spontaneous circulation; VF: ventricular fibrillation. Reproduced from Filgueiras-Rama et al.12 with permission of the publisher.
Risk score based on the predictive performance of the model. (A) Observed (triangles) and predicted (circles) probability of favorable neurological outcome for the entire population. Blue and red represent favorable (FNP) and non-favorable neurological performance (non-FNP), respectively (dark-filled circles, retrospective; light-filled circles, prospective). Overall, above 93% of observations were correctly classified. We defined four risk groups of non-FNP performance according to their risk scores as follows: expected FNP (VL; Very Low risk and L; Low risk) and expected non-FNP (H; High risk and VH; Very High risk). (B) Percentage of patients (observed, dark gray and predicted, light gray) who belong to each of the risk score groups in both the retrospective (B1) and prospective cohorts (B2). (α) and (β) represent false negative and positive individuals, respectively. Reproduced from Filgueiras-Rama et al.12 with permission of the publisher.
Despite the potential clinical impact of an ECG-based prognostic tool easily available at hospital admission, the multivariable model mentioned above has not been validated in a multicenter study with a larger number of patients. Besides, the model was tested only in a small control cohort (without comatose status after the DC shock/s), in whom risk score stratification should show consistently favorable neurological performance (FNP).
The AWAKE study (NCT03248557) aims to overcome previous limitations to establish the early prognostic value of a VF spectral-based model in resuscitated comatose survivors admitted to specialized intensive care units after VF-related SCD. The study will also compare the predictive performance of the model with a clinical-based model including current brain biomarkers and imaging data. This article describes the design and justification for the AWAKE study.
MethodsStudy designThe AWAKE study is an investigator-initiated, multicenter, observational study currently underway in 4 centers in Spain (Hospital Clínico San Carlos, Hospital Universitario La Paz, Hospital General Universitario de Ciudad Real, and Hospital Universitario Gregorio Marañón), and open to more participant hospitals. Only tertiary care hospitals with expertise in the management of SCD and post-resuscitation care will participate in the study. All centers are required to have on-site 24/7 availability for percutaneous coronary intervention and critical care units staffed by cardiologists and/or critical care specialists. This selective recruitment is supported by recent data suggesting that admission to invasive heart centers is associated with lower mortality after out-of-hospital cardiac arrest (OHCA).22
Consecutive patients admitted after out- or in-hospital cardiac arrest due to VF will be screened for inclusion in the study. Patients will be classified into either of two groups:
- (1)
Assessment group: comatose survivors (GCS≤8) after RoSC and in whom neurological prognosis is unknown upon admission. This group is divided into a prospective cohort (new admissions) and a retrospective one, in which cases will be obtained from existing databases in the participating centers.
- (2)
Control group: patients who are conscious (GCS=15) and whose neurological status is known and good at admission. This will be the control group for the spectral-based predictive model, setting the gold standard for predicting FNP.
The study protocol has been approved by the ethics committee of the Hospital Clínico San Carlos, compliant with the Helsinki Declaration. According to current national regulations (Real Decreto 1090/2015), the study is classified as not-for-profit clinical research, and no further clearance in each participating center is required. Every patient will be requested to sign an informed consent form (ICF) before inclusion in the study. If patient's condition makes it unfeasible to obtain a signed ICF, it will be requested to their next of kin. Prospective patients will be requested to sign the ICF during hospital admission, whereas retrospective patients/relatives will sign it at the time of follow-up contact. The main investigator at each participating center will be responsible for its on-site obtainment and storage according to current Spanish law.
Decisions to withdraw life support will be led by the physician in charge and discussed with representatives according to institutional standards, with no intervention whatsoever from the investigating team.
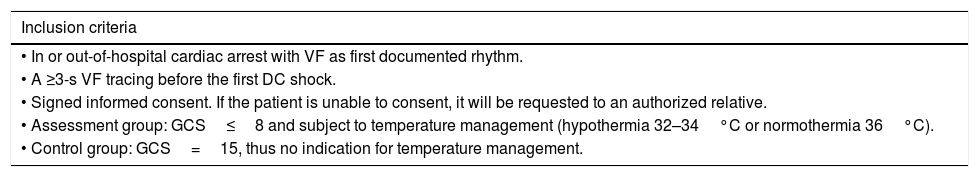
Inclusion and exclusion criteriaThe inclusion criteria for both study groups (Assessment and Control) are described in Table 1. Eligible patients will need to fulfill all of the inclusion criteria. The following exclusion criteria will also apply:
- •
First documented rhythm other than VF (e.g. ventricular tachycardia, pulseless electrical activity, asystole).
- •
Unavailable or suboptimal quality of the ECG tracing before the first DC shock.
- •
Terminal disease or cognitive impairment before the SCD event.
- •
Other possible causes of comatose status different from SCD (e.g. drugs, traumatic brain injury, hypoxia).
- •
Aged under 18.
- •
Unwilling to provide the informed consent.
- •
Comatose status (GCS≤8) and absence of temperature management or GCS≥9 if temperature management was undertaken.
- •
Hemodynamic instability leading to incomplete 24h of temperature management.
- •
Early mortality and absence of subsequent withdrawal of sedation to assess cerebral performance.
- •
GCS<15 in patients allocated to the control group.
Inclusion criteria.
| Inclusion criteria |
|---|
| • In or out-of-hospital cardiac arrest with VF as first documented rhythm. |
| • A ≥3-s VF tracing before the first DC shock. |
| • Signed informed consent. If the patient is unable to consent, it will be requested to an authorized relative. |
| • Assessment group: GCS≤8 and subject to temperature management (hypothermia 32–34°C or normothermia 36°C). |
| • Control group: GCS=15, thus no indication for temperature management. |
Patients in the assessment group must have undergone therapeutic mild hypothermia (target temperature 32–34°C) or controlled normothermia (target temperature 36°C) for at least 24h according to the institution protocol, in agreement with current requirements.23 Routine use of prehospital or in-hospital cooling during cardiopulmonary resuscitation with rapid infusion of large volumes of cold intravenous fluid is discouraged, due to lack of evidence to improve neurological outcome or mortality.24 Rewarming strategies (e.g. passive or active rewarming) are open depending on institutional standards. Sedation, drug-induced paralysis during mechanical ventilation, the use of cardiovascular drugs, support devices or any other intensive care therapy is left at the criteria of the treating physicians.
The flow chart of the study is represented in Fig. 3.
Data collection and spectral analysis of VF tracingsAll data will be entered in an electronic Case Report Form (eCRF) by individual investigators at each center. Demographic and clinical variables will be obtained from all available medical records and by in-person interview, if possible. Clinical variables and biomarkers as neuron-specific enolase (highest recorded value), electroencephalogram, somatosensory evoked potentials (N20 component with median nerve stimulation) and brain imaging, are encouraged to be collected in the prospective cohort. VF recordings prior to the first DC shock will be scanned using commercial desktop scanners (600 dots per inch) and uploaded to the eCRF. Data consistency and quality will be weekly monitored by one of the investigators (M.M.B).
Stored ECG traces in a codified digital format will be processed as reported elsewhere.12 Briefly, digitization will be performed using a supervised semi-automatic approach based on region of interest selection, histogram thresholding and intensity transformations. Segments are extracted after segmentation and signal codification from artifact-free VF tracings. Signals are band-pass filtered between 1.5 and 40Hz. Two independent investigators will visually inspect the extraction quality (J.G.Q and M.M.B). Averaged power spectral density will be obtained at each frequency using the non-parametric Welch method for using fast Fourier transform and normalized to the peak power in the 1.5–10Hz band for each patient. DF, HL-PSDR and HL-pKR, along with the number of DC shocks before RoSC, will be the variables used to obtain a model-derived risk score for outcome prediction. Investigators blinded to clinical outcome will perform all data analysis, extraction and quantification using custom-made scripts of MATLAB software (V. 2016b, The Mathworks, Inc., Natick, MA). The results of such analysis will not be disclosed to the treating physicians and site investigators, not to interfere in standard care, decision-making and outcome assessment.
Outcome assessmentThe primary clinical outcome is FNP during hospitalization. All patients will be classified using the Pittsburgh Cerebral Performance Categories (CPC) outcome categorization of brain injury, according to current standards of care for SCD assessment.25,26 Patients will be considered to have FNP if they score 1 or 2 in the CPC scale (good performance and moderate disability, respectively). CPCs 3, 4 and 5 (severe disability, vegetative state and brain death, respectively) will be considered as a non-FNP. In the prospective cohort, neurological outcome will also be determined using the mini-mental state examination (MMSE). The threshold value in MMSE for normal cognitive function is 24/30.27,28 In the prospective cohort, neurological outcome will be established before hospital discharge. In the retrospective cohort, the assessment will be done using medical records and in-person interviews with the patient or relatives.
During follow-up, neurological outcome will be prospectively assessed by in-person interview in all survivors. Patients within the prospective cohort will be evaluated 6 months after hospitalization. In the retrospective cohort, the follow-up will take place at the moment of patient enrolment or contact with patient's relatives, in case of decease.
The secondary clinical outcomes will be survival to hospital discharge, and FNP and survival at follow-up. The control group will be used to test the predictive model against a cohort of patients with known FNP, in which the model should also properly predict FNP.
Sample size and study timelineThe sample size was estimated using the diagnostic performance obtained from the pivotal study.12 The spectral-based four-variable model using DF, HL-PkR, HL-PSDR, and the number of shocks delivered before RoSC, showed a diagnostic sensitivity of 0.94. Looking for a 95% confidence interval and 5% precision, and assuming that 61% patients will show FNP according to our previous research, a total of 143 individuals (both prospective and retrospective cohorts) suitable for analysis must be included.
It is estimated that each of the aforementioned centers receives ∼60 SCD survivors per year, but only around one-fourth of them will fulfill the inclusion criteria, namely VF as first documented rhythm and ECG tracing availability. Considering the incidence of cases per hospital and retrospective cases from previous years, the sample size will be achieved in a time frame of 30 months. The latter includes the follow-up period for the last group of patients who will be enrolled in the study. As of the writing of this manuscript, the centers have already evaluated 160 patients, of whom 47 met the inclusion criteria and are enrolled in the study.
Statistical analysisPatients from the assessment group (prospective and retrospective) will be categorized according to the risk score obtained from the multivariate spectral-based model.12 More specifically, patients will be categorized within four subsets for FNP as follows: very high and high probability of FNP (expected FNP), low and very low probability of FNP (expected non-FNP). Model-derived categorization will be compared with clinical outcomes to assess model sensitivity, specificity and accuracy during hospitalization and follow-up.
In order to assess the clinical relevance of the spectral-based model we will compare its performance and overall accuracy with the most associated and clinically relevant variables (e.g. highest recorded value of neuron-specific enolase, somatosensory evoked potentials). To develop a clinical-based predictive model, each of the clinical variables will undergo univariate analysis to evaluate its association with in-hospital FNP.
Normal distribution of variables will be assessed with the Shapiro–Wilk test. Statistical significance will be assessed by the parametric Student's t-test or the non-parametric Mann–Whitney test, as appropriate. If necessary, we will use Bonferroni correction for multiple comparisons. Categorical variables and percentile comparisons will be performed using a Chi-squared test or the Fisher's exact test, as appropriate. Two-sided p<0.05 will be considered statistically significant. Variables with statistically significant differences and clinically relevant variables will be regressed out against the in-hospital FNP by using a stepwise backwards multivariate logistic regression approach.29 The clinical-based model will be developed to predict FNP with the highest sensitivity and specificity achievable by using the minimum number of variables that guarantees the best performance and predictive accuracy.
DiscussionThe management of cardiac arrest after VF is still a matter of debate and the mechanisms involved in cardiopulmonary resuscitation and successful recovery are not fully understood.4 Nowadays, there is no reliable index that provides early neurological and survival prognosis on admission in patients with comatose status after DC shock and RoSC. Moreover, many VF episodes are unwitnessed, or patient collapse occurs during fast ventricular tachycardia before VF onset,30 making it difficult to assess VF onset. The latter makes unreliable the time to advanced life support, as reported in our previous series.12 However, the strong predictive value of a spectral-based model may be explained by its ability to provide reliable information of both the time from VF onset and the quality of cardiopulmonary resuscitation.15,16
Patients’ relatives and survivors of such a dramatic event as SCD due to VF face the risk of severe cerebral disability and terrible social consequences.31 This study aims to provide multicenter validation of a spectral-based model to obtain early and accurate prognosis information from the very moment of resuscitation and RoSC. The prognostic score will provide objective data that will be extremely valuable to patients’ relatives and physicians working in intensive care units, either to minimize the initial impact when chances for recovery are present or to provide realistic information about severe cerebral damage in those patients without chances for recovery. The latter has significant clinical impact considering the current trend toward increasing incidence of SCD in developed nations and limited resources for a rising population of patients requiring highly specialized intensive care who might not have chances for recovery due to severe cerebral damage.
ConclusionsThere is lack of reliable and early prognostic biomarkers in comatose survivors after SCD due to VF. VF-derived spectral characteristics are robust indicators of time in VF and myocardial ischemia, and a spectral-based model of VF tracings is a promising tool to obtain early prognostic data after SCD. This study aims to provide multicenter validation of such a model based on VF-analysis.
FundingDr. J. Palacios-Rubio has received a fellowship grant from the Spanish Society of Cardiology to support the execution of this study.
Conflict of interestNone relevant to the topic.
Dr. Palacios-Rubio has been awarded with a fellowship grant from the Spanish Society of Cardiology related to the execution of the featured study. The CNIC is supported by the Ministry of Economy, Industry and Competitiveness (MINECO) and the Pro CNIC Foundation, and is a Severo Ochoa Center of Excellence (MINECO award SEV-2015-0505). Partially supported by European Regional Development Fund (ERDF). We thank the computing department of CNIC for their assistance during eCRF development.