Describe 2 rare causes of central serous chorioretinopathy.
Clinical casesCase 1: A 35-year-old woman with loss of vision in her left eye, with a recent history of a flu vaccination. This could have been the process that triggered an immune response, with increased circulating immune complexes that favor choroidal ischemia.
Case 2A 41-year-old man with loss of vision in his left eye. As history, had consumed cocaine, which could be related to its adrenergic effect adrenergic, and earlier excimer laser refractive surgery (LASIK).
ConclusionIn both cases there was a temporal relationship between cause and effect.
Describir dos causas poco frecuentes de coriorretinopatía serosa central.
Casos clínicosCaso 1: mujer de 35 años con pérdida de visión del ojo izquierdo. Como antecedente presenta vacunación reciente contra la gripe. Podría ser la causa del proceso por desencadenar una respuesta inmune con aumento de inmunocomplejos circulantes que favorecieran isquemia coroidea. Caso 2: varón de 41 años con pérdida de visión del ojo izquierdo. Como antecedente presenta toma de cocaína, que podría relacionarse por su efecto adrenérgico, y antigua cirugía refractiva con láser excimer (LASIK).
ConclusiónEn ambos casos se produce una relación temporal entre causa-efecto.
Central serous chorioretinopathy (CSC) is a multifactorial disease of complex etiology1 that combines choriocapillaris fluid leak with impaired retinochoroidal pumping function of the retinal pigment epithelium (RPE).
Clinical casesCase 1A 35-year-old woman with loss of vision in her left eye progressing for 5 days. Her best corrected visual acuity (BCVA) was 0.6. Her medical history included recent Mutagrip® influenza vaccination.
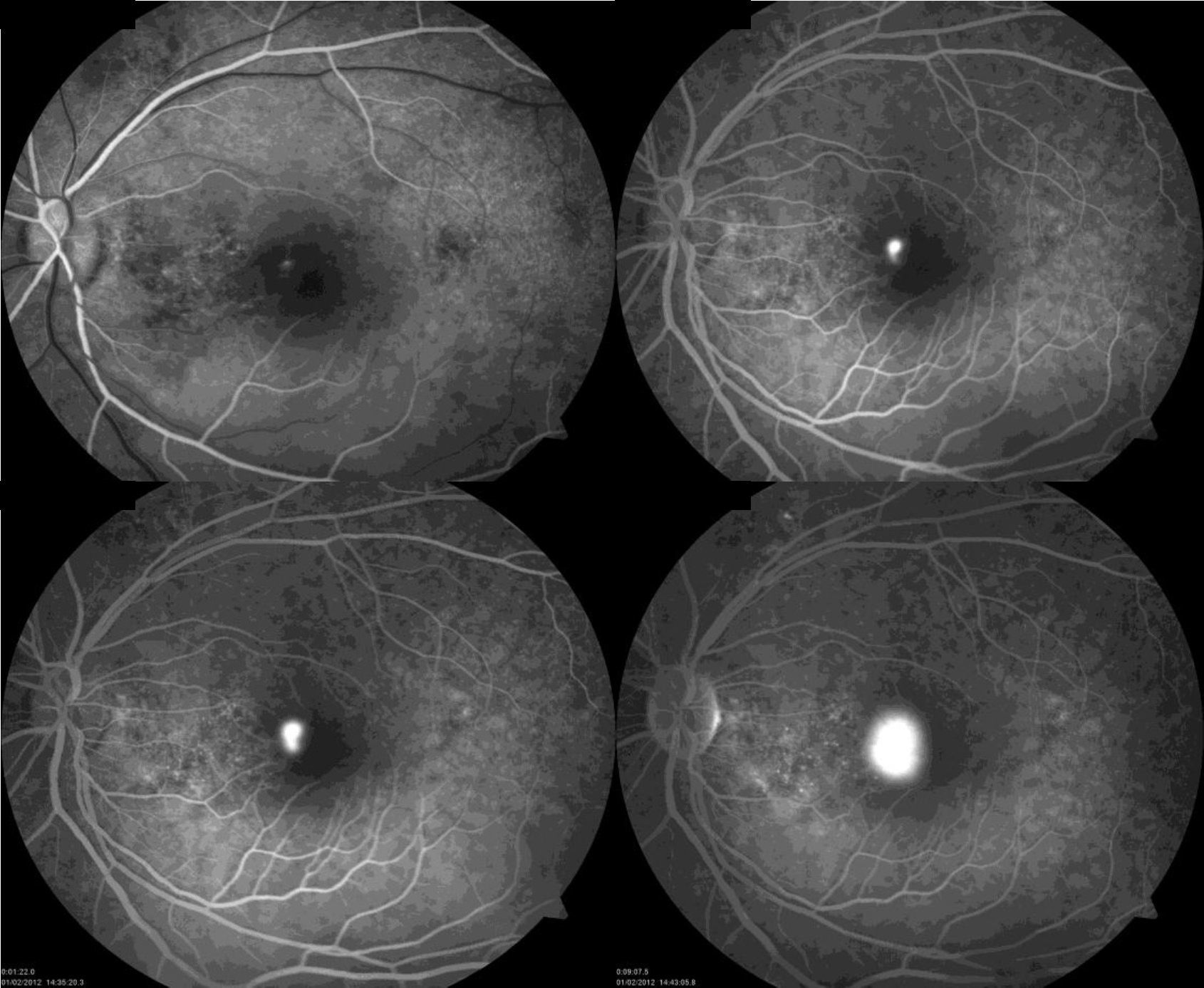
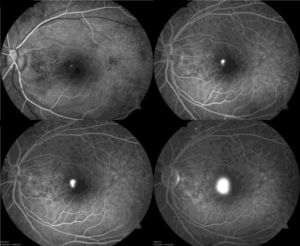
On examination, she presented relative afferent pupillary defect in her left eye. The ocular fundus shows a well-defined neurosensory retinal detachment (NRD) that occupies the entire posterior pole.
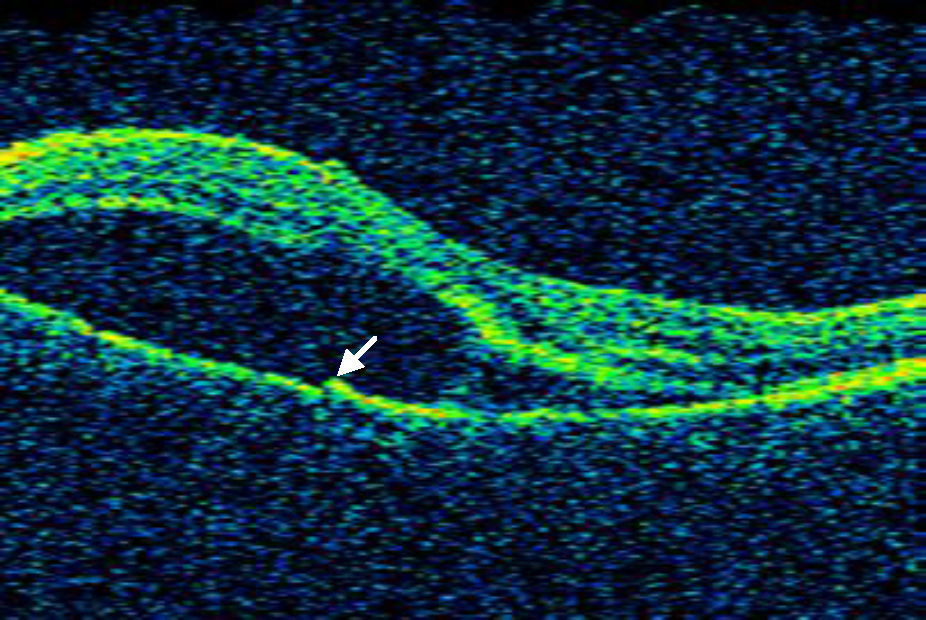
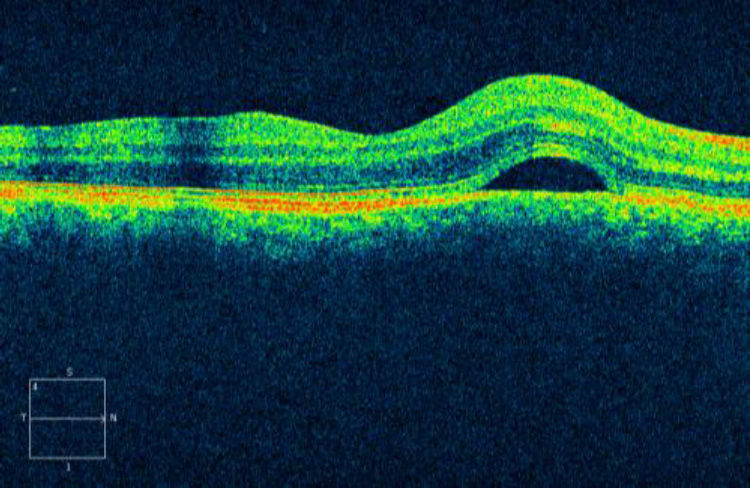
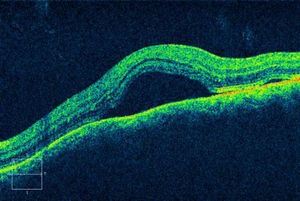
Optical coherence tomography (OCT) (Cirrus HD-OCT version 4.0, Zeiss) shows a large NRD with a retinal pigment epithelium (RPE) defect, slightly raised on the inferonasal quadrant, which coincides in the fluorescein angiography (FA) with the hyperfluorescent vanishing point in a chimney-smoke-like pattern (Figs. 1 and 2).
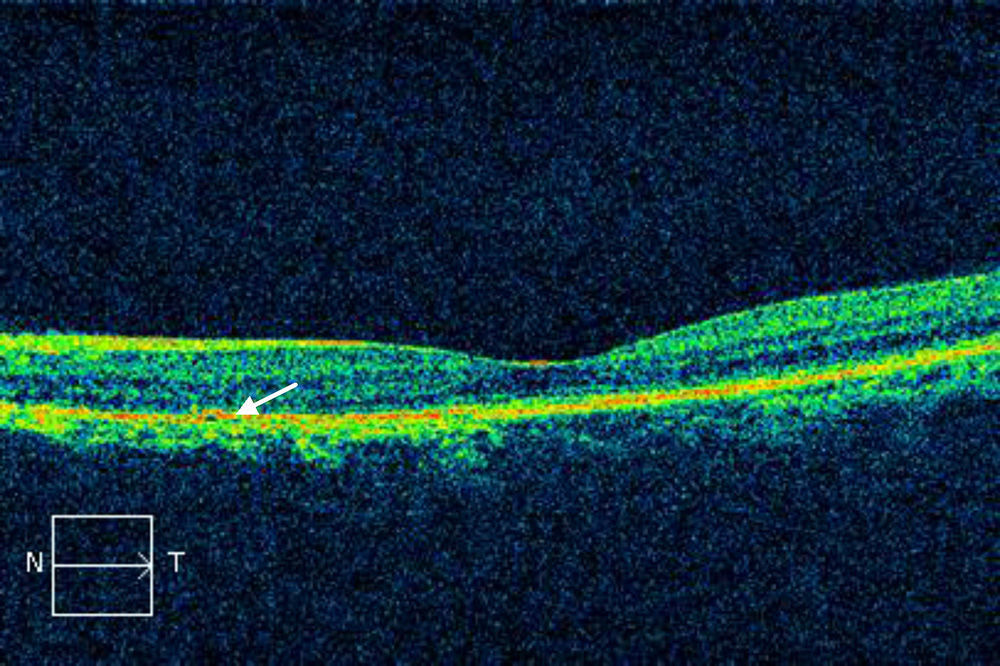
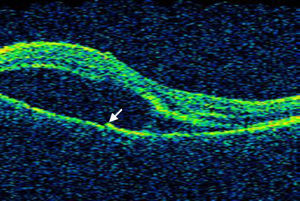
The NRD was resolved a month and a half later (Fig. 3). However, her BCVA is 0.8.
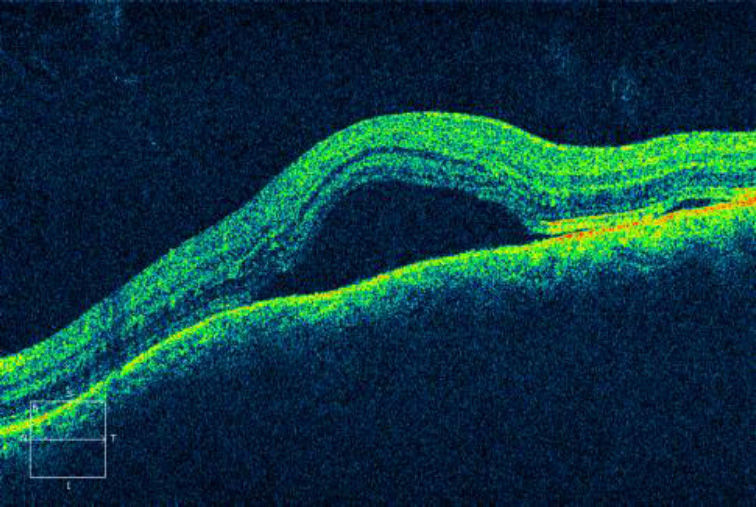
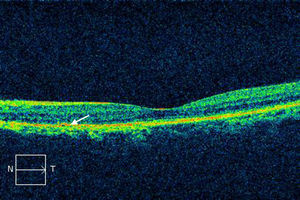
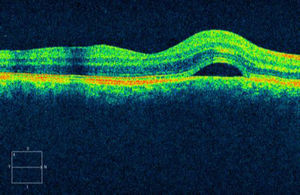
Case 241-year-old male with decreased visual acuity in his left eye, with 24h of progression. His medical history includes myopic LASIK intervention 6 years ago and cocaine consumption 2 days prior. BCVA in his right eye was 1, and 0.6 in the left eye. Examination of the right eye fundus shows one NRD in papillomacular bundle, and 2 NRD in the left eye: one subfoveal and the other one temporal fovea. Macular OCT confirmed NRD without any other abnormalities (Figs. 4 and 5). NRD resolved at 3 months, and his BCVA was 1 in both eyes.
DiscussionCSC pathogenesis remains unclear, but there is a strong association with the use of corticosteroids as described by Bouyon et al. in 2 cases treated with corticosteroids in which clinical improvement occurred after they are removed.2 As in cataracts or glaucoma, CSC may be a possible side effect of treatment with corticosteroids and, therefore, internists must be aware of it.
Although advances have occurred in understanding autoimmune diseases, the possible mechanisms triggering tolerance break remain unknown. The vaccine produces an abnormal immune activation; there are reports of small vessel lymphocytic vasculitis cases after vaccination due to immunoglobulin G and C3 immune complex deposits in dermal vessels. It has also been linked to genetic predisposition to cause an autoimmune reaction, HLA-DRB1 variant specifically.3
Bradley et al. present a CSC case within 14 days from Anthrax vaccination4 and cited 3 cases after smallpox vaccination reported by Rosen et al.
There are reports that indocyanine green angiography has exposed choroidal vasoconstriction with blood flow deterioration in the CSC, whereby CSC may be a result of choroidal ischemia with venous congestion.5
There is a clear association between cocaine use and ischemic heart disease due to catecholamine reuptake blocking caused by the drug.6 Therefore, in case 2, adrenergic system stimulation may also be involved in acute CSC, not just by possible cocaine-triggered ischemia, but also by an increase in endogenous corticosteroids, which increase adrenergic receptor sensitivity.1 Hassan et al. already linked ecstasy use with CSC.7
In our case, moreover, the patient had undergone LASIK refractive surgery, albeit 6 years prior. Although there are CSC cases after PRK due to myopia reported by Moshirfar et al.,8 and cases after LASIK from hyperopia reported by Peponis et al.,9 all occurred in the first month. Risks during surgery that could lead to CSC are: suction at submacular level and stress; however, it has not been linked to topical use of corticosteroids.
Ascaso et al. reported the first case of rare bilateral maculopathy (non-CSC) after long-lasting intranasal cocaine use, causing alteration in color vision, without alteration detected in OCT. Early hyperfluorescence at the foveal level, maintained until late stages, is commonly observed with FA.10
ConclusionCSC could be an uncommon but significant adverse event after vaccination, to be taken into account especially in patients with immune disorders.
With regard to Case 2, although the link between cocaine and CSC is inconclusive, patient was informed of the high probability of recurrence if he uses again. Therefore, patients with acute CSC must be questioned carefully on drug use.
Both the cause–effect relationships in these two cases are only hypotheses, and are not proven in this paper.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Palacios AI, Rodríguez M, Martín MD. Coriorretinopatía serosa central de etiología inusual: a propósito de dos casos. Arch Soc Esp Oftalmol. 2014;89:275–278.