Type 2 idiopathic macular telangiectasia (MacTel 2) is a rare retinal disease that has still not been well-defined. The aim of the present manuscript is to describe the clinical features by multimodal retinal imaging, to present the functional characteristics, and to estimate the prevalence of the disease.
MethodsA retrospective study was conducted on the 12 eyes of 6 patients with MacTel 2. Fundus color photographs, fundus autofluorescence, fluorescein angiography, optical coherence tomography (OCT), and OCT-angiography were performed and subsequently analyzed. Visual acuity (VA) was prospectively recorded. The prevalence was established based on the patients referred to a specialized macular diseases unit. Minimum follow-up period was 18 months.
ResultsPrevalence of MacTel 2 in our study was 0.12%. Clinical features were presented using multimodal retinal imaging. VA remained stable during follow-up. Three patients developed choroidal neovascularisation (CNV), requiring intravitreal treatment with antiangiogenic agents.
ConclusionsThe prevalence of the disease found was 0.12%. The study using multimodal imaging allows a more accurate diagnosis and follow-up of this pathology. The VA is maintained during the 18-month follow-up (p=.492). Patients who develop CNV and are treated with antiangiogenic agents appear to respond adequately to them. More studies are needed to establish these conclusions.
Las telangiectasias maculares idiopáticas de tipo2 (MacTel2) son una enfermedad retiniana poco frecuente y aún no completamente caracterizada. El objetivo del presente trabajo es describir las características clínicas en imagen multimodal de la retina, presentar los resultados funcionales y estimar la prevalencia de la enfermedad en nuestro medio.
MétodosEstudio retrospectivo en el que se analizaron 12 ojos de 6 pacientes con MacTel2. Se realizaron fotografías en color de fondo, autofluorescencia, angiografía fluoresceínica, tomografía de coherencia óptica (OCT) y angiografía por OCT y se analizaron posteriormente. Se registró prospectivamente la agudeza visual. La prevalencia se estableció en base en los pacientes referidos a una unidad especializada en enfermedades maculares. El período mínimo de seguimiento fue de 18meses.
ResultadosLa prevalencia de MacTel2 en nuestro medio fue de 0,12%. Se presentaron las características clínicas en imagen multimodal de la retina. La agudeza visual permaneció estable durante el seguimiento (p=0,492). Tres pacientes desarrollaron neovascularización coroidea (NVC), requiriendo tratamiento intravítreo con agentes antiangiogénicos.
ConclusionesLa prevalencia de la enfermedad en nuestro medio es del 0,12%. El estudio mediante imágenes multimodales permite un diagnóstico y seguimiento de esta patología más preciso. La agudeza visual se mantuvo durante los 18meses de seguimiento. Los pacientes que desarrollan NVC y son tratados con agentes antiangiogénicos parecen responder adecuadamente a ellos. Se necesitan más estudios para establecer estas conclusiones.
Macular telangiectasia are caused by dilatation of retinal capillaries in the macula1,2 and can be idiopathic or primary—when underlying etiology cannot be identified—or secondary to a range of retinal vascular pathologies, primarily venous occlusions.3 There are 2 types of idiopathic or primary macular telangiectasia (MacTel)4 according to the classification updated by Yannuzzi et al.1 In the first place, MacTel 1 or aneurismatic present unilaterally and are more frequent in male patients, characterized by aneurysms with varying sizes and more or less profuse lipidic exudation and variable severity macular edema. In the second place, MacTel type 2 (MacTel 2) or perifoveal usually presents bilaterally and asymmetrically without visible aneurysms in conventional ocular fundus examination. In turn, MacTel 2 can be classified on the basis of the presence of secondary choroidal neovascularization (CNV) as nonproliferative—in the absence of this complication—and proliferative—when the presence of CMV is evidenced. Overall prevalence has been estimated at 0.1%.5
The advent of new ocular fundus imaging diagnostic techniques has enabled greater knowledge of the physiopathological and structural substrate of MacTel 2 due to multiple clinic signs described with the analysis of various imaging forms. The objective of this manuscript is to summarize the characteristics of said pathology through multimode image and estimate the prevalence of the disease in the authors’ environment.
Material and methodsThe present study was designed as a retrospective case series. It included all patients with a clinical diagnostic of MacTel 2 visited by the same physician (RGP), a specialist in optical coherence tomography (OCT) interpretation at the Macula Unit of the University and Polytechnic Hospital of La Fe (Valencia, Spain). The study was carried out in accordance with the Helsinki declaration, the approval of the institutional board and the regulation of informed consent. The clinic and epidemiological characteristics of all patients were registered and analyzed together with the ocular fundus multimode image examination. The minimum follow-up during which comparisons were made was 18 months.
Best corrected visual acuity data were obtained with Snellen optotypes in decimal scale from the electronic clinic records of the patients. Similarly, the images obtained during the follow-up of each MacTel 2 patient were assessed. These included conventional color retinography (Visupac, Carl Zeiss Meditec, Jena, Germany), high resolution macular OCT images (HRA-OCT Spectralis, Heidelberg Engineering, Heidelberg, Germany), sodium fluorescein angiography (HRA-OCT Spectralis, Heidelberg Engineering, Heidelberg, Germany), ocular fundus shortwave autofluorescence (Blue Peak Spectralis, Heidelberg Engineering, Heidelberg, Germany), infrared reflectance (HRA-OCT Spectralis, Heidelberg Engineering, Heidelberg, Germany) and OCT angiography (OCT-A) by means of full-spectrum protocol (full-spectrum amplitude decorrelation angiography [FSADA]) (HRA-OCT Spectralis, Heidelberg Engineering, Heidelberg, Germany).
The statistical study was made with nonparametric tests, specifically the Wilcoxon test for comparing mean values of related samples.
ResultsEpidemiological characteristicsOverall, the study included 12 eyes of 6 patients with a clinic diagnostic of MacTel 2. In accordance with the registry comprising all 4903 patients visited by the same specialist (RGP) of the Macula Unit of the University and Polytechnic Hospital of La Fe, Valencia, Spain, between January 2013 and May 2017, the estimated prevalence being 0.12%.
All patients were female, with a mean age of 63.00±6.03years (range: 56–74; median: 63). The mean follow-up of all these cases was 5.17±3.72years (range: 1–12; median: 4.5). As all patients had at least 18 months follow-up, visual acuity changes were registered randomly and assessed on the basis of said follow-up period.
Systemic associations in the sample of patients with MacTel 2 include the fact that 5 out of 6 patients (83%) exhibited systemic arterial hypertension during treatment, while 3 had diabetes mellitus type 2 (50%), and one was an active smoker (16%).
Functional characteristicsBest corrected visual acuity at diagnostic was 0.71±0.25 (range: 0.3–1.0; median: 0.7). Visual acuity at the end of the 18-month follow-up, was 0.71±0.26 (range: 0.3–1.0; median: 0.7). No statistically significant differences were observed (p=0.492).
Mean intraocular pressure at diagnostic was 17.16±2.41mmHg (range: 12–21; median: 17.5) and at the end, 18.5±2.69mmHg (range: 15–25; median: 18). Statistically significant differences were observed in these values (p=0.010); however, none of the patients required antihypertensive treatment.
Albeit subjectively, all patients referred progressive loss of vision, particularly for reading, as well as progressive alteration in contrast sensitivity and adaptation from light to dark.
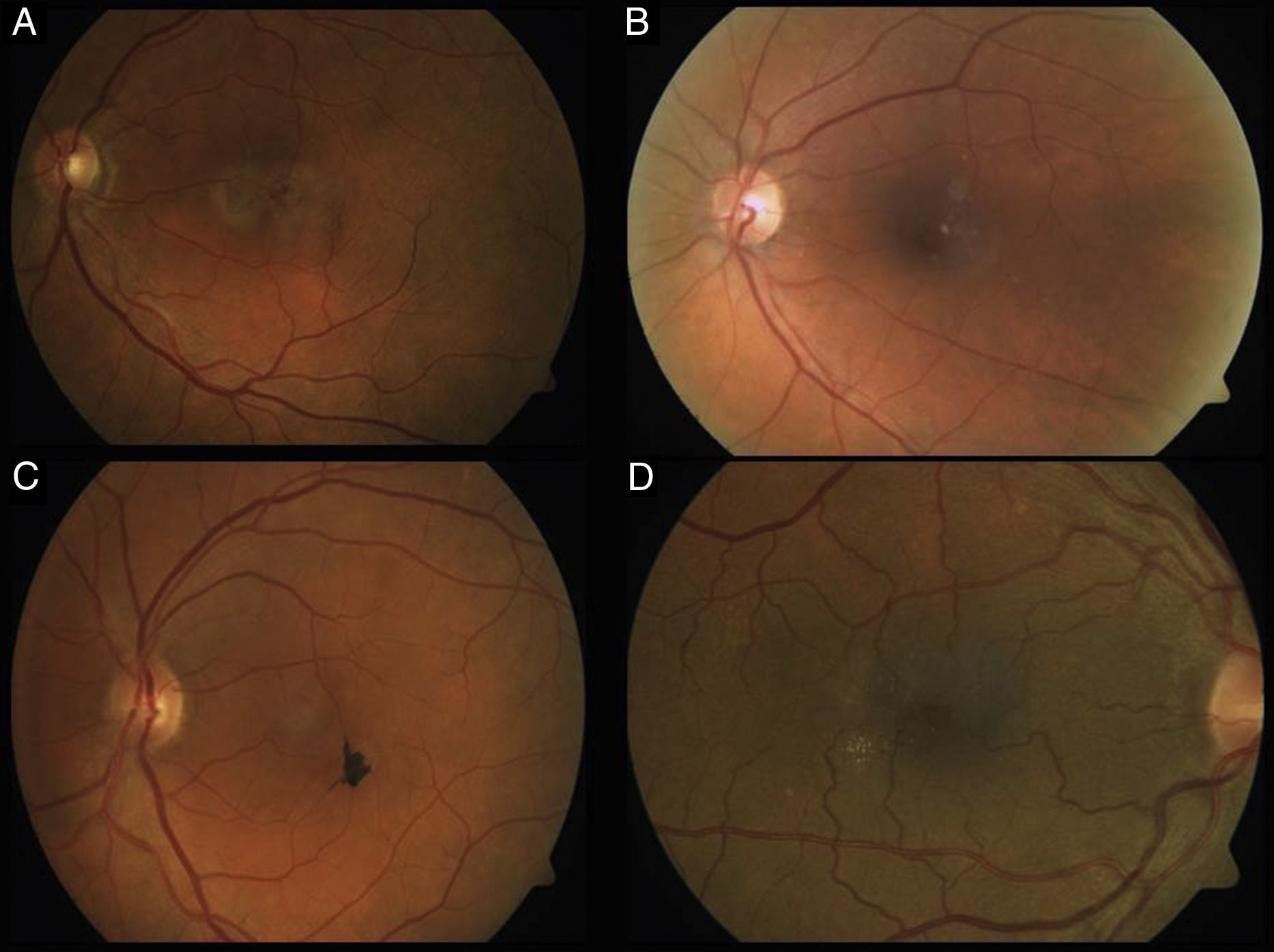
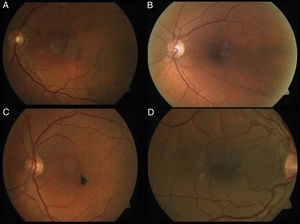
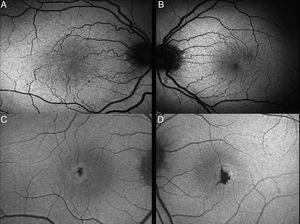
Phenotype characteristics in color retinographyThe main and most typical characteristic observed in all the retinographies of the eyes included in the study was the presence of grayish discoloration with loss of patency in the temporal juxtafoveal region (100%). Likewise, venule dilatation with right angle arrangement in the temporal juxtafoveal region was objectively observed in 12 eyes (100%). Finally, hyper-pigmented plates corresponding to retina pigment epithelium hyperplasia were observed in 3 eyes (25%), as well as crystalline deposits in 6 eyes (50%) (Fig. 1).
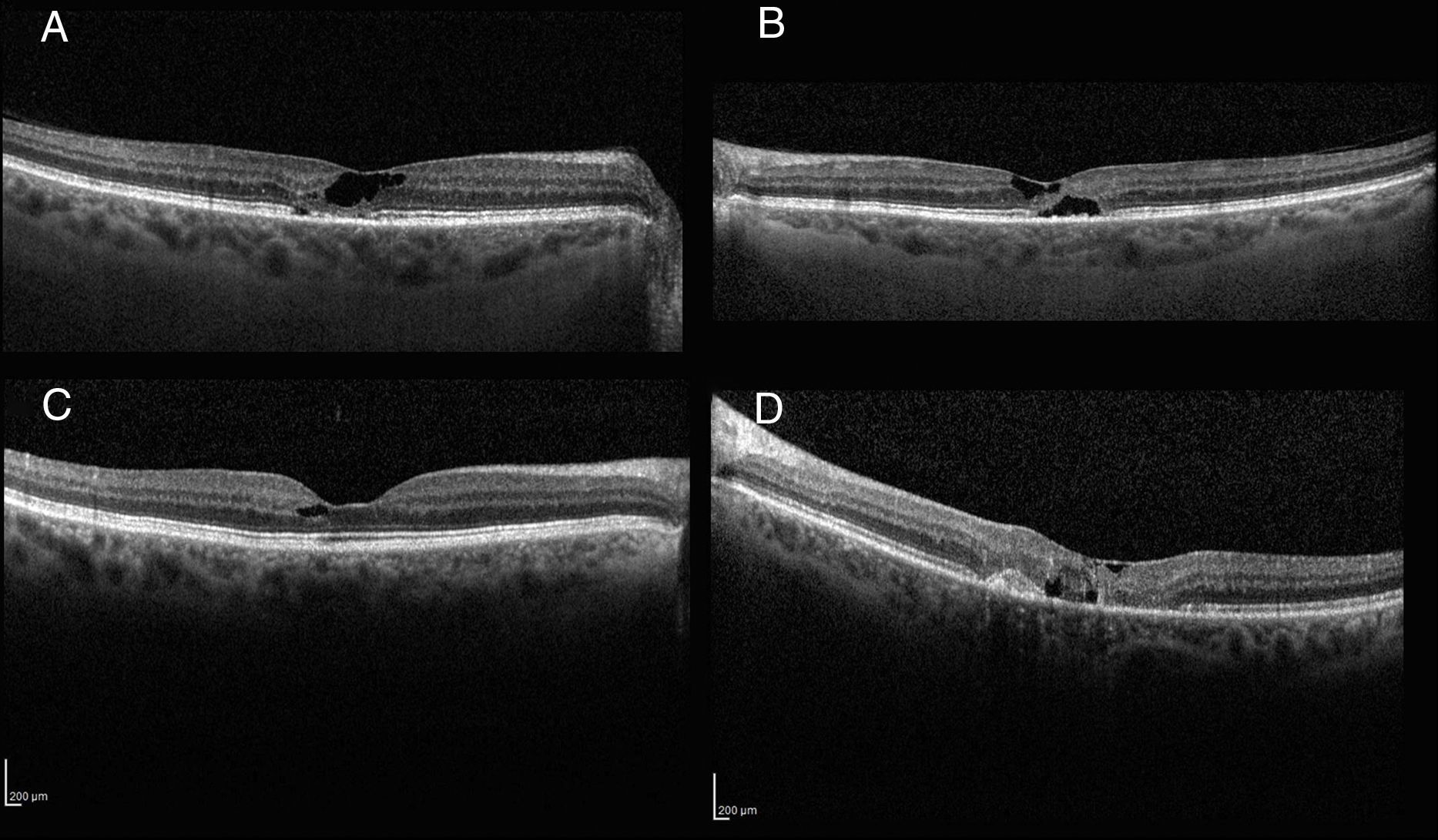
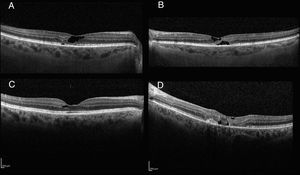
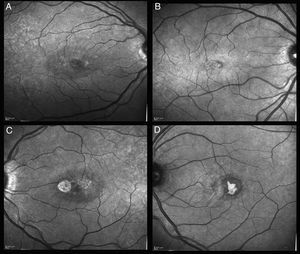
Morphometric tomographic characteristicsOCT images were characterized by the presence of hypo-reflective spaces that did not produce retinal thickness increases in all cases (100%), together with external retina layer disruption in 3 of the studied eyes (25%). Fig. 2 comprises macular OCT images showing typical lesions as well as a case with CNV.
Baseline foveal thickness was 237.7±36.6μm (range: 196–301μm; median: 240μm); at 18 months follow-up the thickness was 246.3±37.5μm (range: 186–306μm; median: 232μm). No significant changes were observed (p=0.844).
OCT analysis showed the development of CNV in 3 eyes (2 patients) that required intravitreal treatment with antiangiogenics medicaments (one injection in 2 eyes and 4 and the remainder) with remission of activity and subsequent visual acuity improvement up to previous levels. In accordance with the anatomic classification of neovascular lesions, this type of CNV was type 2 lesions in all cases.
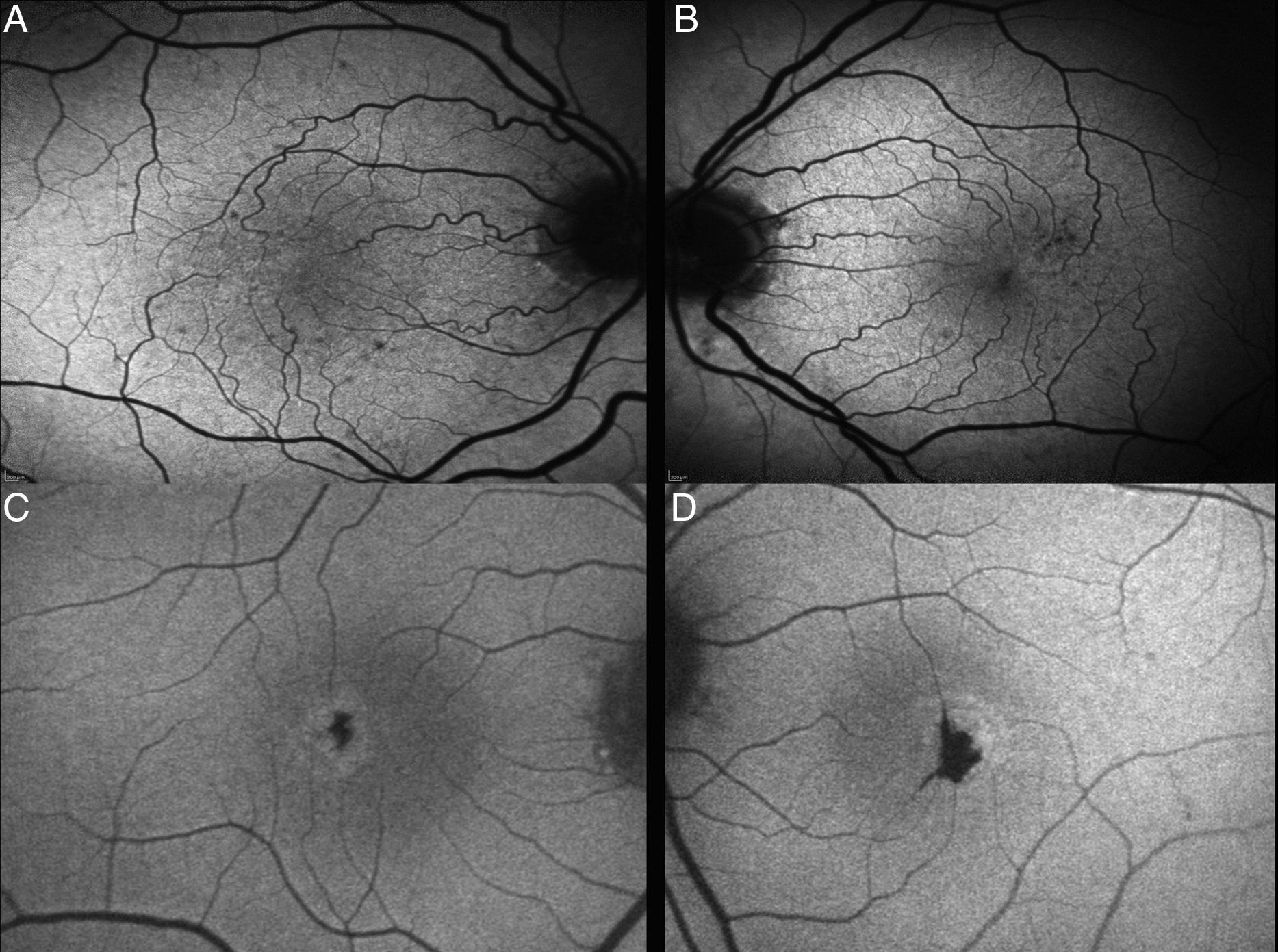
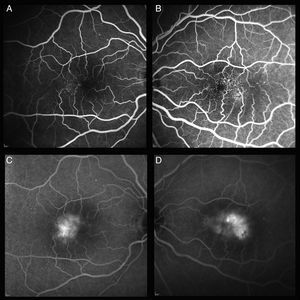
Phenotype characteristics in ocular fundus autofluorescenceAutofluorescence images of patients with this pathology initially showed loss of hypoautofluorescence, that was observed in all patients (100%). In one case, epithelium hyperplasia was also observed (Fig. 3).
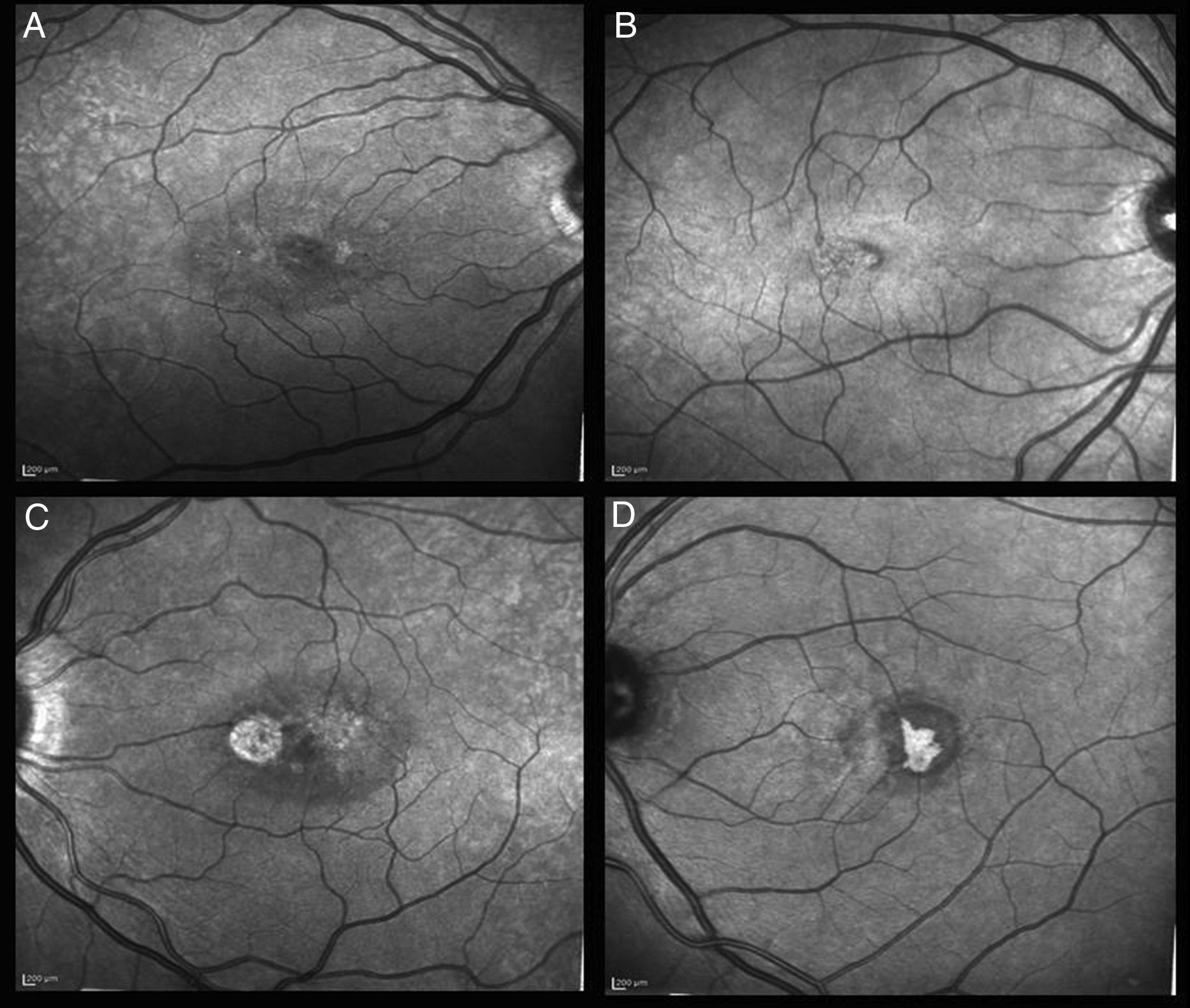
Phenotype characteristics in infrared reflectanceInfrared reflectance images show a hypo-reflective perimacular ring and hyper-hypo-reflectance areas matching pseudocysts and retina pigment epithelium (RPE) hyperplasia, in addition to small reflectile crystals (Fig. 4).
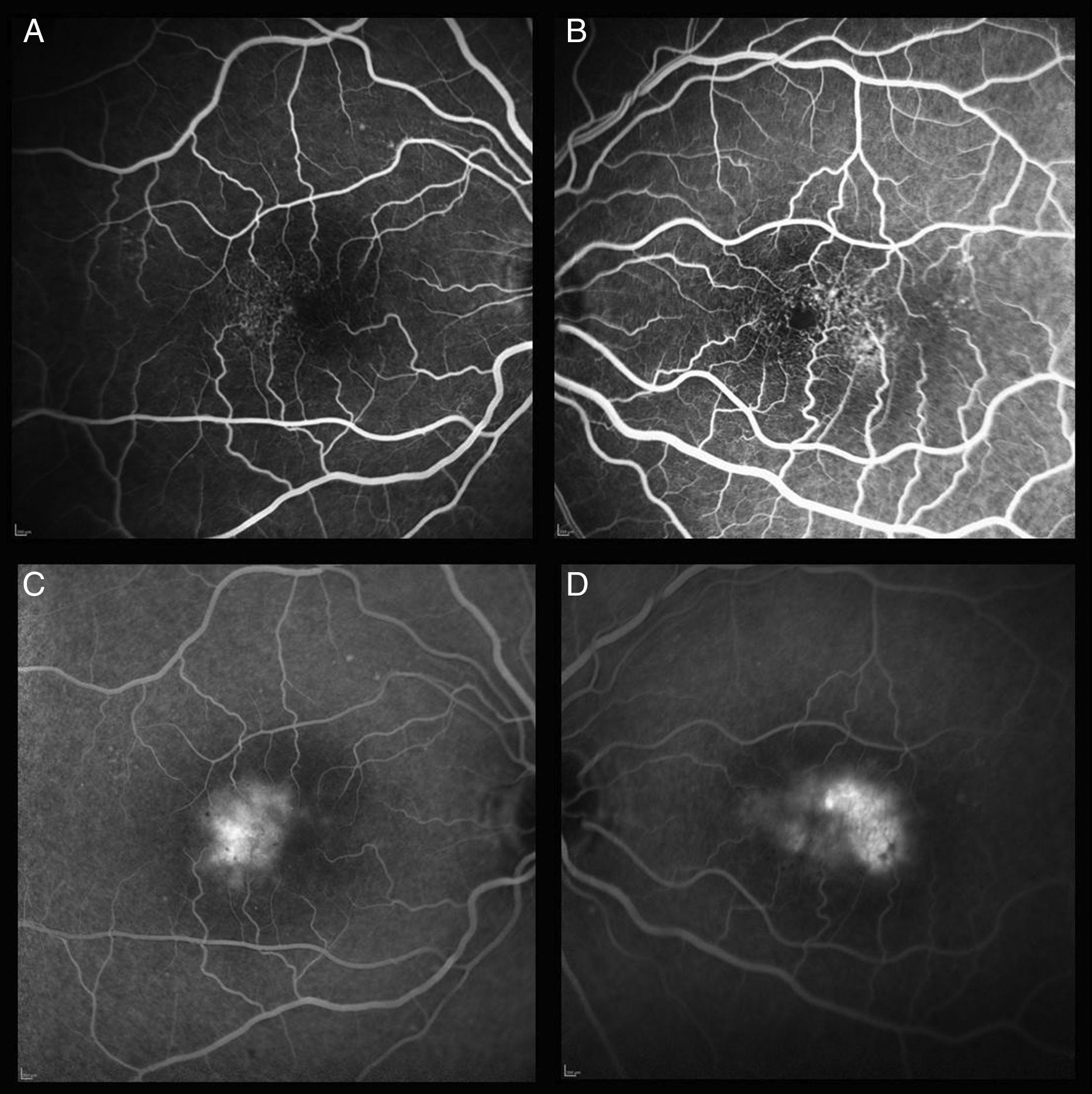
Phenotypic characteristics in fluorescein angiographyEarly stages of fluorescein angiography revealed little or no capillary dilatation evidence. Late stages showed perifoveal temporal retina staining respecting the central foveal area. With the progression of the disease, alterations completely surrounded the fovea. In the patients of this study, leak areas were observed above all in the temporal parafoveal area. In some cases the presence of CNV was also found in angiographic images (Fig. 5).
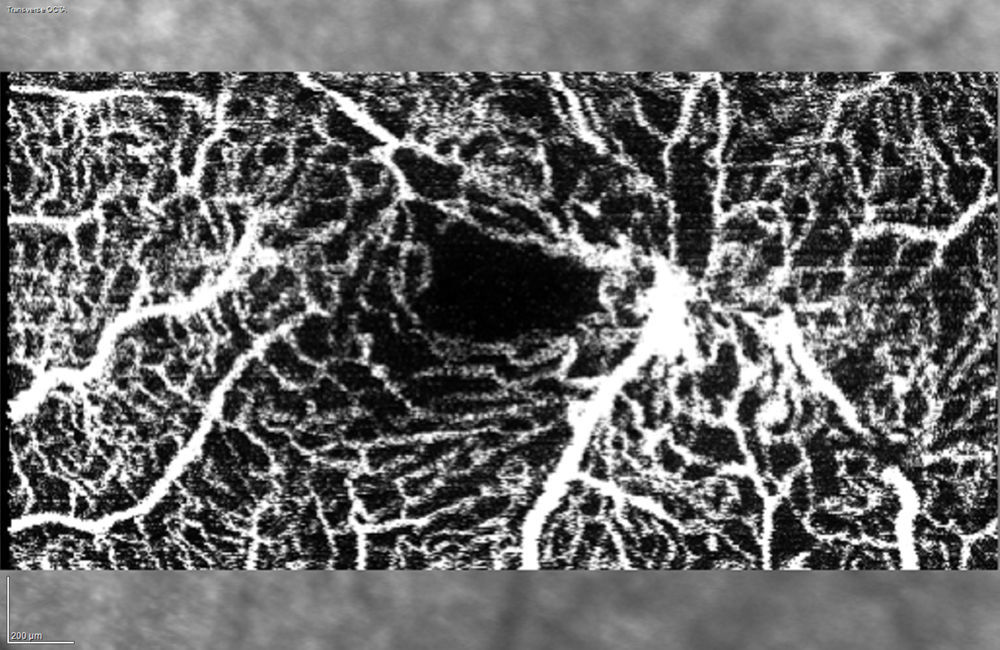
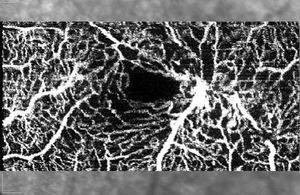
Phenotypic characteristics in optic coherence tomography angiographyOCT-A provides detailed images of retinal microcirculation. In the case of this pathology, vessel patency alterations are observed such as ectasic vessels with diffused or sectorial shape, distorted or even with neovascularization. The most frequent finding is vascular dilatation visible in the deep capillary plexus, which can progress and compromise the superficial capillary plexus. In addition, intravascular spaces increase with progressive capillary rarefaction and abnormal capillary anastomosis (Fig. 6).
DiscussionThe prevalence of type 2 macular telangiectasia was established at approximately 0.1%.5 In the authors’ environment, a prevalence of 0.12% was found, similar to previously reported data.
Type 2 macular telangiectasia do not exhibit gender predisposition. However, in the present case a predominance in females was observed as in other studies such as by Kim et al.4 and Mehta et al.6
In a number of studies, a significant relationship has been observed between MacTel 2 and medical factors such as smoking, diabetes, arterial hypertension and obesity.7 In the present study, the percentage of patients with arterial hypertension was 83%, of which 50% had diabetes and 16% were smokers, without finding other relevant pathological antecedents.
Initially, MacTel 2 could be asymptomatic.4 Several authors describe that visual acuity diminishes slowly in nonproliferative stages,8 as observed by the authors in their patients. In contrast, the eventual appearance of CNV produces hemorrhages, fibrosis and neurosensory detachment with rapid and severe central vision impairment,9 which could be recovered after treatment with antiangiogenics drugs.
Various treatments have been applied for each stage of said pathology, including laser photocoagulation, photodynamic therapy, photothrombosis measured with indocyanine green, trans-pupil thermotherapy, surgery and medicaments such as acetazolamide, corticoids or intravitreal antiangiogenics as well as combined treatments.3 Recent studies have suggested that laser treatment is not indicated due to risk of worsening and NVC.3 Intravitreal antiangiogenic therapy has no effect on the evolution of the disease in nonproliferative cases, although it is the treatment of choice in neovascularization cases as it has demonstrated to improve visual acuity, resolve the CMV and diminish macular thickness.3 There is not sufficient evidence for a specific treatment, and initial injection with pro re nata posterior administration appears to be adequate according to some authors.3
Clinically, funduscopic examination reveals loss of retinal transparency in the juxtafoveal temporal area. In advanced stages, a visible dilatation of juxtafoveal retinal capillaries occurs,7 with the additional possibility of hyper-refringent crystalline deposits located at the level of the vitreoretinal interface,6 as well as right-angle dilated venules9 and pigment changes such as hyperplasia plates in the RPE and/or intraretinal pigment migration.7 These typical lesions were observed in the patients of the present study.
Technological developments have improved knowledge of retinal diseases.4,10,11 Spectral domain OCT enables diagnosing MacTel 2 cases at earlier and asymptomatic stages.4 Tomographic images show diminished thickness, temporal foveal and perifoveal thinning with loss of neurosensory retina tissue, giving rise to pseudocysts in the internal as well as external layers of the retina. These findings were previously described in numerous studies.9,12–14
It would be important to emphasize the necessity of following up these patients due to the possibility of developing neovascularization and subsequent vision impairment requiring treatment. The authors recommend utilizing OCT for follow-up.
As can be observed in the autofluorescence images, initially it can increase (hyperautofluorescence) due to the loss of luteal pigment15 prior to clinic and angiographic changes.16
It has been suggested that macular pigment plays an important role in the physiopathology of several diseases, and diminished amounts of lutein and zeaxanthin have been described in the foveal area of patients with MacTel 2.17 Macular pigment density distribution has been calculated with autofluorescence, identifying abnormal paracentral distribution.18 The central area exhibits reductions whereas the peripheral area is preserved, which could indicate a local defect in the ability to accumulate pigment.18 It has not been demonstrated that supplements with lutein and zeaxanthin are able to modify the course of the disease.
Infrared reflectance produces a characteristic finding of a hyporeflective perimacular ring and hyper-hyporeflectance areas matching pseudocysts and RPE hyperplasia, in addition to small refractile crystals.19
In fluorescein angiography, perifoveal ectasic dilated capillaries can produce exudation. In early stages, little or no evidence of capillary dilatation can be seen. In later stages, perifoveal temporal retina staining is observed, which usually respects the central foveal area. As the disease progresses, alterations completely encircle the fovea.9,20 In the patients of this study, leak areas were observed mainly in the temporal parafoveal area, a characteristic previously described by Thorell et al.9
OCT-A provides detailed images of retinal microcirculation. In the case of this pathology, vessel patency alterations are observed such as ectasic vessels with diffused or sectorial shape, distorted or even with neovascularization. The most frequent finding is vascular dilatation visible in the deep capillary plexus, which can progress and compromise the superficial capillary plexus.9,21
Limitations of the present study include its retrospective nature and the small number of cases. It would be convenient to study the evolution of this disease in longer terms.
Conflict of interestsNo conflict of interests was declared by the authors.
Please cite this article as: Bayón-Porras RM, Pascual-Camps I, Plaza-Laguardia C, Gallego-Pinazo R. Telangiectasias maculares idiopáticas de tipo 2: prevalencia en nuestra área y estudio morfométrico y fenotípico. Arch Soc Esp Oftalmol. 2018;93:105–112.