We report 2 cases of patients affected by non-infectious corneal macroperforations treated with TachoSil® and Tutopach®, which closed the defect.
DiscussionThis procedure is an excellent choice for the emergency treatment of corneal perforation, especially in those centres that have no other therapeutic options, preserving the eye and visual acuity.
Se presentan dos pacientes diagnosticados de macroperforación corneal no infecciosa. Se tratan con la combinación de TachoSil® y Tutopach®, consiguiendo el cierre completo de la perforación.
DiscusiónEsta técnica proporciona una excelente alternativa para el tratamiento de urgencia de la perforación corneal, sobre todo en aquellos centros en los que no se dispone de opciones terapéuticas más regladas, preservando el ojo y la agudeza visual útil.
Nontraumatic sterile corneal perforations exceeding 2mm diameter are difficult to treat. The causes which could produce said perforations include hypovitaminosis A, peripheral ulcerative keratitis, dry eye keratopathies, neurotrophic keratopathies exposure keratopathies.
This report presents a therapeutic option comprising the combined use of TachoSil® (Nycomed Pharma, Zurich, Switzerland) and Tutopach® (Tutogen Medical GmbH, Neunkirchen, Germany) for closing a sterile and nontraumatic corneal perforation exceeding 2mm diameter.
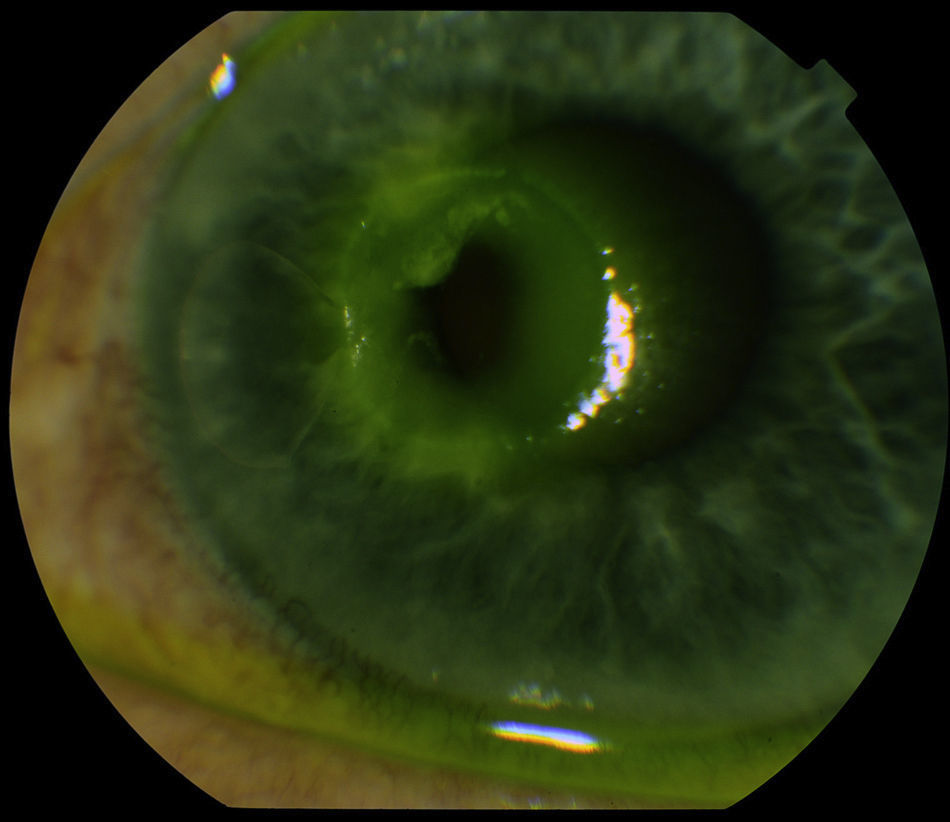
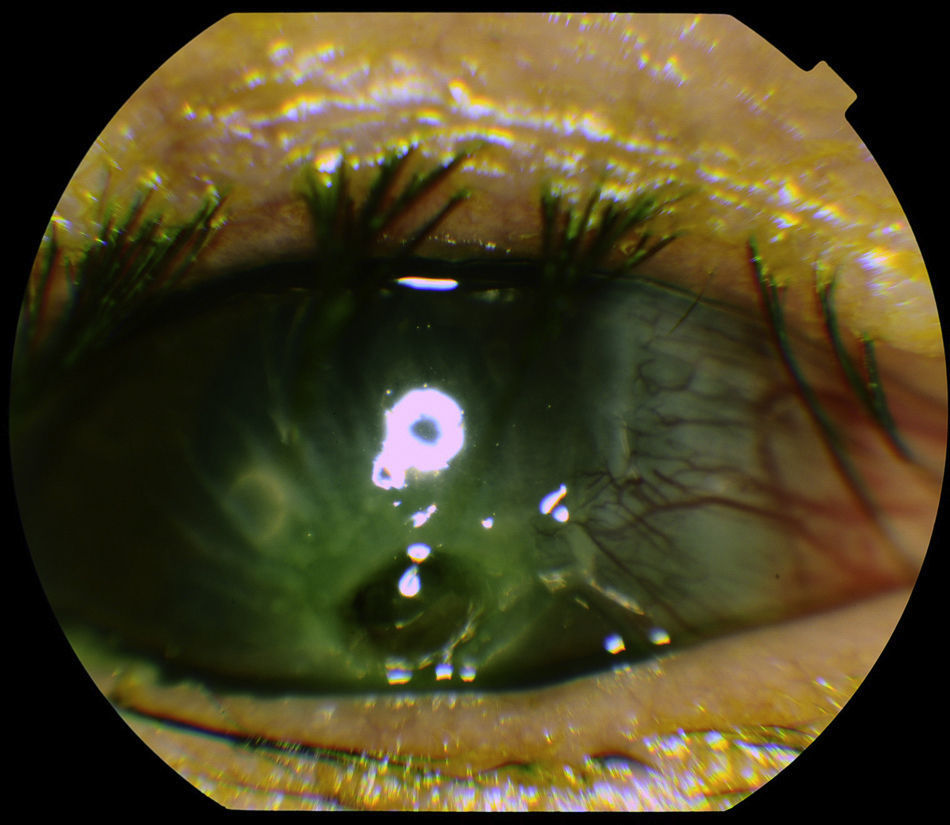
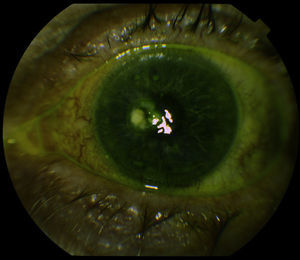
Clinical caseClinical case 1Male, 64, diagnosed with Sjögren syndrome, who visited the emergency service referring ocular pain, reddening and photophobia in both eyes with several days evolution. Examination revealed bilateral corneal ulcers with ocular perforation in the left eye, with positive Seidel test (Fig. 1).
Therapeutic contact lens was provided and antibiotic treatment was established together with lubrication after discarding infectious disease. Due to the urgency of the condition, the size of the perforation, the risk of contralateral eye perforation and the lack of other therapeutic options such as amniotic membrane or scleral patches, it was decided to perform the following technique.
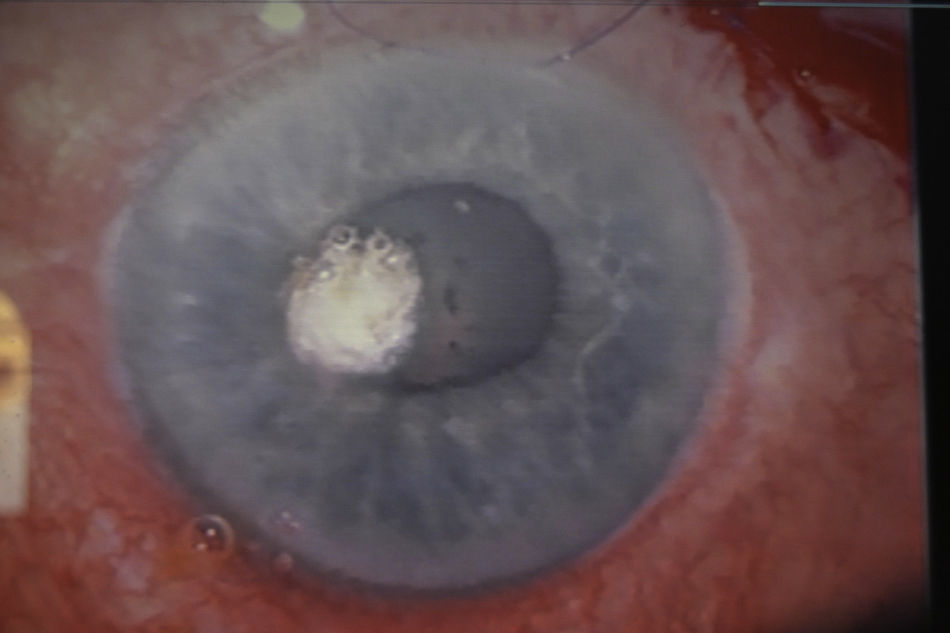
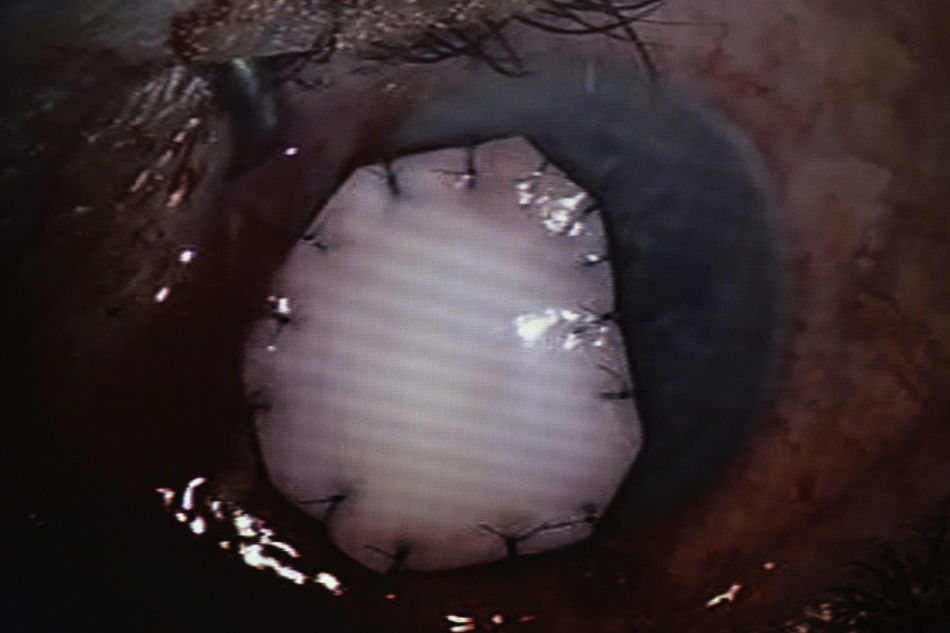
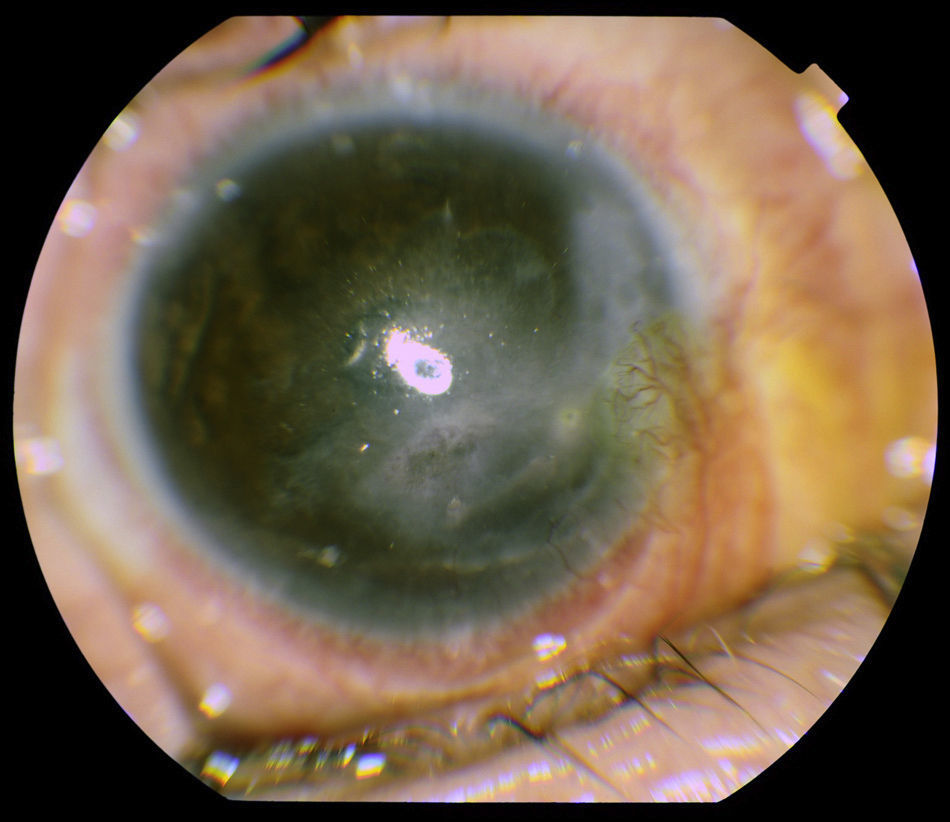
TachoSil® was placed to cover the perforation, covering with a Tutopach® patch larger than the perforation diameter to enable suture and maintain occlusion long enough before reabsorption (Figs. 2 and 3).
The suture was made with loose, radial and equidistant stitches. The eye was occluded during 48h.
After 2 days, the eye was uncovered in the practice and exhibited correct occlusion of the perforation. The patch began to thin out one week after surgery and after about 10 days it began to reduce in size until it disappeared entirely after 2 months post-surgery.
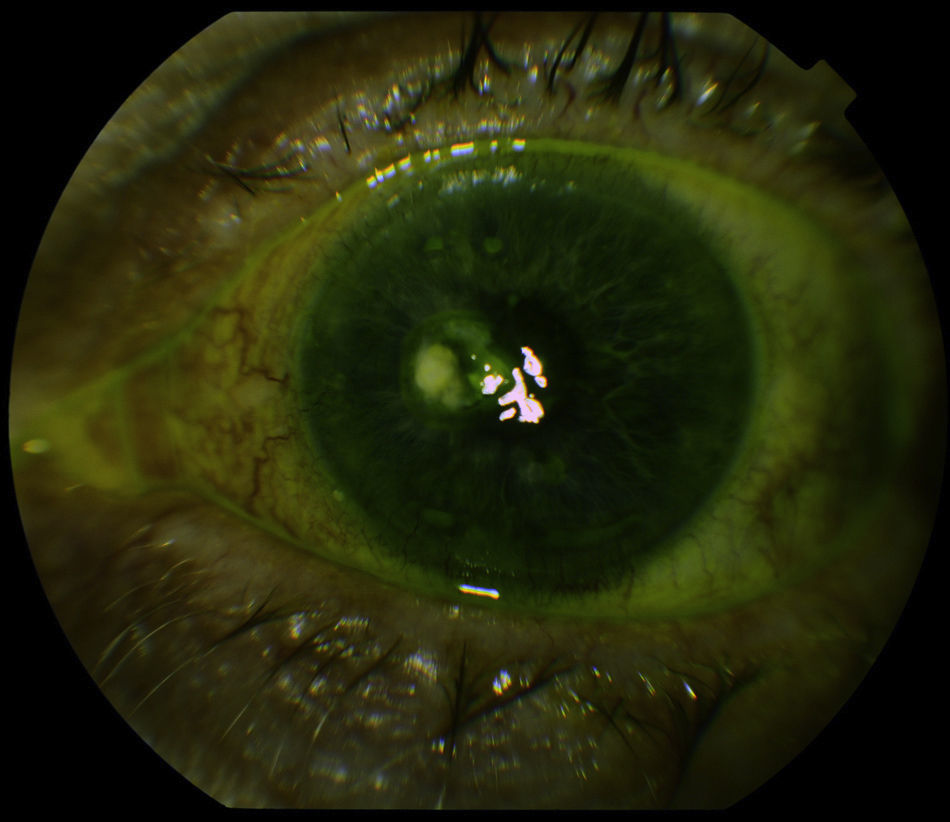
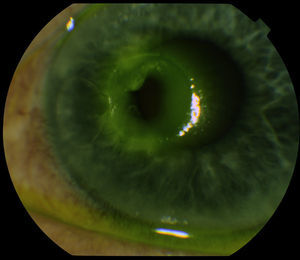
Topical treatment with autologous serum was established and at present the patient exhibits BCVA of 1 in the right eye and of 0.5 in the left eye, with corneal opacification in the perforation area. To this date, the patient remains asymptomatic (Fig. 4).
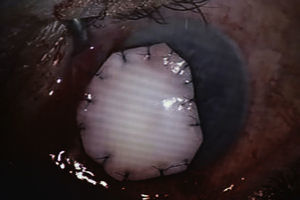
Clinical case 2Male, 65, with personal history of retina detachment in the left eye and ocular dryness syndrome who visited the emergency service due to visual acuity loss and pain in right eye (the only eye) of 5 days evolution.
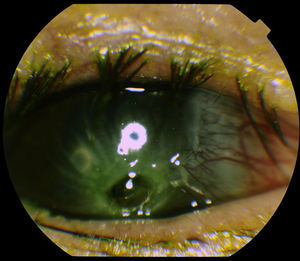
The patient exhibited a visual acuity in the right eye of <0.05. Examination revealed a corneal perforation with a diameter of 2.5mm (Fig. 5).
Antibiotic treatment was initiated and urgent surgery was carried out, placing TachoSil® by way of cover for the perforation and this was covered with a Tutopach® patch.
Two days post-surgery the eye was uncovered in the practice, with the perforation being adequately occluded. In this case, the patch degraded quicker and disappeared one month after surgery.
At present, the patient exhibits BCVA of 0.1 in the right eye with corneal opacification in the perforation area. To date the patient remains asymptomatic (Fig. 6).
DiscussionTherapeutic options for corneal perforation include therapeutic contact lenses, tissue adhesives, the application of a conjunctival flap, a scleral flap, amniotic membrane and keratoplasty among others.1,2
Published cases on the use of TachoSil® in nontraumatic corneal microperforations (under 1mm) report good tolerance at the ocular level and adequate evolution of corneal perforations.3,4 Recently, the use of TachoSil® has been reported in corneal macroperforations (over 2mm) associated to amniotic membrane with good results in what concerns corneal perforation closure.5
TachoSil® is a collagen sponge covered with coagulation factors that produces hemostasia, with sealing properties and providing a supportive adhesive matrix.
In the clinical cases reported herein, the corneal perforations exceed 2mm, which led us to consider supplementary treatment in addition to TachoSil®, based on the application of a Tutopach® patch in the absence of other materials for sealing and stabilizing the structure of the eye.
Tutopach® is a biological membrane obtained from bovine pericardium which can be preserved in a sterile form. It has already demonstrated its usefulness in glaucoma surgery.6
The references below report the use of Tutopach® for preventing neurotrophic ulcer perforation, associating tarsorrhaphy during 2–3 weeks.7
In the present case we have gone a step beyond, i.e., we did not use the product to prevent but to treat established macroperforations to achieve corneal closure, patient tolerance and visual acuity preservation without requiring prolonged ocular occlusion, which is very important in patients with only one eye as in the second clinic case.
The technique described above provides an excellent alternative for urgent treatment of corneal perforations, mainly in hospitals which are not equipped for more conventional therapeutic options, preserving the eye and useful visual acuity.
Conflict of interestNo conflict of interest has been declared by the authors.
Please cite this article as: Feliciano-Sánchez A, García-Gil R. Macroperforaciones corneales no infecciosas tratadas con la asociación de TachoSil® y Tutopach®. A propósito de 2 casos. Arch Soc Esp Oftalmol. 2014;89:250–253.