Although the ophthalmic manifestations appear to be associated with the coronavirus disease 2019 (COVID-19), there is not enough evidence. Hence, the aim of this study was to determine the various types and frequency of ophthalmic manifestations in patients recovered from SARS-CoV-2 infection in Mexico.
Material and methodsThis retrospective, observational and descriptive study included all patients recovered from SARS-CoV-2 infection attending the tertiary level hospital of Mexican Social Security Institute (IMSS) from June 2020 to June 2022. During the hospital admission of patients, the demographic data such age, name, gender was recorded. Ophthalmologic examination was performed under torchlight by an ophthalmologist in the Department of Ophthalmology from IMSS. Data was compiled and statistically analyzed using Fisher’s exact test and Spearman correlation.
ResultsA total of 3081 SARS-CoV-2-positive patients were recorded, of which 318 (10.32%) met the inclusion criteria. Of them, 21 (6.60%) had ophthalmic manifestations and the female-to-male ratio was 1.6:1. The mean age (±SD) was 47.95±15.27 years and the median (interquartile range) time from the diagnosis of COVID-19, as defined by positive SARS-CoV-2 RT-PCR testing, to detection of the ophthalmic manifestation was 31 (142) days. The most common ocular manifestation was orbital mucormycosis (23.80%). Interestingly, the presence of ophthalmic manifestations was not associated with severe COVID-19 (p=0.665).
ConclusionsThe ophthalmic manifestations are infrequent in patients recovered from severe COVID-19. Nevertheless, further large sample studies are needed to confirm these findings.
Aunque las manifestaciones oftálmicas parecen estar asociadas a la enfermedad por coronavirus 2019 (COVID-19), no hay suficiente evidencia. Por ello, el objetivo de este estudio fue determinar los distintos tipos y la frecuencia de las manifestaciones oftálmicas en pacientes recuperados de la infección con SARS-CoV-2 en México.
Material y métodosEste estudio retrospectivo, observacional y descriptivo incluyó a los pacientes infectados con SARS-CoV-2 de junio de 2020 a junio de 2022. El examen oftalmológico fue realizado bajo luz de linterna por un oftalmólogo del Departamento de Oftalmología. Los datos fueron analizados estadísticamente mediante la prueba exacta de Fisher y la correlación de Spearman.
ResultadosSe registraron un total de 3.081 pacientes positivos de SARS-CoV-2, de los cuales 318 (10,32%) cumplían los criterios de inclusión. De ellos, 21 (6,60%) tenían manifestaciones oftálmicas y la proporción entre mujeres y hombres era de 1,6:1. La edad media (±DE) fue 47,95±15,27 años y la mediana (rango intercuartil) del tiempo transcurrido desde el diagnóstico de COVID-19, definido por la prueba RT-PCR del SARS-CoV-2 positiva, hasta la detección de la manifestación oftálmica fue de 31 (142) días. La manifestación ocular más común fue la mucormicosis orbital (23,80%). Interesantemente, la presencia de manifestaciones oftálmicas no fue asociada con COVID-19 grave (p=0,665).
ConclusionesLas manifestaciones oftálmicas son infrecuentes en los pacientes recuperados de COVID-19 grave. No obstante, se necesitan más estudios con una muestra de mayor tamaño para confirmar estos hallazgos.
Severe acute respiratory syndrome virus (SARS-CoV-2), the cause of coronavirus disease 2019 (COVID-19), causes gastrointestinal and ocular symptoms, hepatocellular injury, neurological disease and dermatological complications due to the presence of its receptor, ACE2, in the cells of these organs.1 Wagner et al. reported that ophthalmic manifestations are related to the activity of the renin-angiotensin system at the ocular level with the presence of the ACE2 receptor.2
Although pulmonary manifestations are the main conditions in patients with COVID-19, Douglas et al. demonstrated a prevalence of ophthalmic manifestations of 1.4%–5.2% in this type of patients.3 On the other hand, Costa et al. reported a prevalence of ophthalmic manifestations of 10% in SARS-CoV-2 infected patients.4 Ophthalmic manifestations included unexplained visual impairment, chemosis, epiphora, conjunctival hyperemia, keratoconjunctivitis, follicular conjunctivitis, pseudomembranous and hemorrhagic conjunctivitis.3 In this regard, ophthalmological manifestations in patients who had COVID-19 can range from mild to severe, causing discomfort, injury, functional limitation and even blindness in the patients involved. However, little is known about ophthalmic manifestations in recovered COVID-19 patients in Mexico. Therefore, the aim of this study was to determine the different types and frequency of ophthalmic manifestations in patients recovered from SARS-CoV-2 infection in Mexico.
Material and methodsStudy design and participantsAn observational, descriptive, cross-sectional, retrospective study was conducted and approved (R-2022-3001-047) by the Ethics and Research Committee of the Unidad Médica de Alta Especialidad, Hospital de Especialidades No. 14, Centro Médico Nacional Adolfo Ruiz Cortines, Instituto Mexicano del Seguro Social (IMSS). Sampling was non-probabilistic and included patients who were positive for SARS-CoV-2 by real-time PCR in the period June 2020 to June 2022. Exclusion criteria: (1) patients with ophthalmic manifestations of known cause prior to infection with SARS-CoV-2, (2) individuals with comorbidity related to the detected ophthalmic manifestation and (3) patients who had no record of care in the Ophthalmology Service. Inclusion criteria: (1) patients between 20 and 80 years of age, (2) individuals seen in the Ophthalmology Department of the UMAE H. E. No. 14, and (3) patients with a positive test for SARS-CoV-2. Patients with a confirmed diagnosis of COVID-19 were classified into four types: (1) mild, patients with mild clinical symptoms and no finding of pneumonia on imaging; (2) moderate, patients with fever and respiratory symptoms, and signs of pneumonia on radiological evaluation; (3) severe, patients who met any of the following criteria (a. shortness of breath, RR≥30 times/min; b. oxygen saturation ≤93% at rest; and c. partial pressure of oxygen [PaO2]/fraction of inspired oxygen [PaO2/FiO2≤300mmHg]; d. lung imaging showing significant progression of injury >50% within 24–48h); and (4) critically ill, patients with respiratory failure that required mechanical ventilation, shock or failure of other organs that required intensive care and treatment. For further analysis in this study, patients were grouped as “non-critical” (classified as mild or moderate) and “critical” (classified as severe or critical). Patients with missing data or without clinical records were eliminated from the study.
Data collectionAll data for patients meeting the inclusion criteria were obtained from physical and electronic records (via the Electronic Health Record system, E.C.E.).
Statistical analysisDescriptive data were obtained for analysis and the association study was performed using Fisher’s exact test. A Spearman correlation analysis was also performed. A value of p<0.05 was considered a statistically significant difference. The data were analysed using IBM SPSSv.25.
Ethical approvalThis study was approved (registration number: R-2020-3001-068) by the Ethics Committee of the Unidad Médica de Alta Especialidad, Hospital de Especialidades No. 14, CMN Adolfo Ruiz Cortines, Instituto Mexicano del Seguro Social (IMSS), including waiver of the requirement for informed consent due to the retrospective nature of the study. The study complied with the Declaration of Helsinki. We certify that all protocols and methods were conducted under the relevant guidelines and regulations.
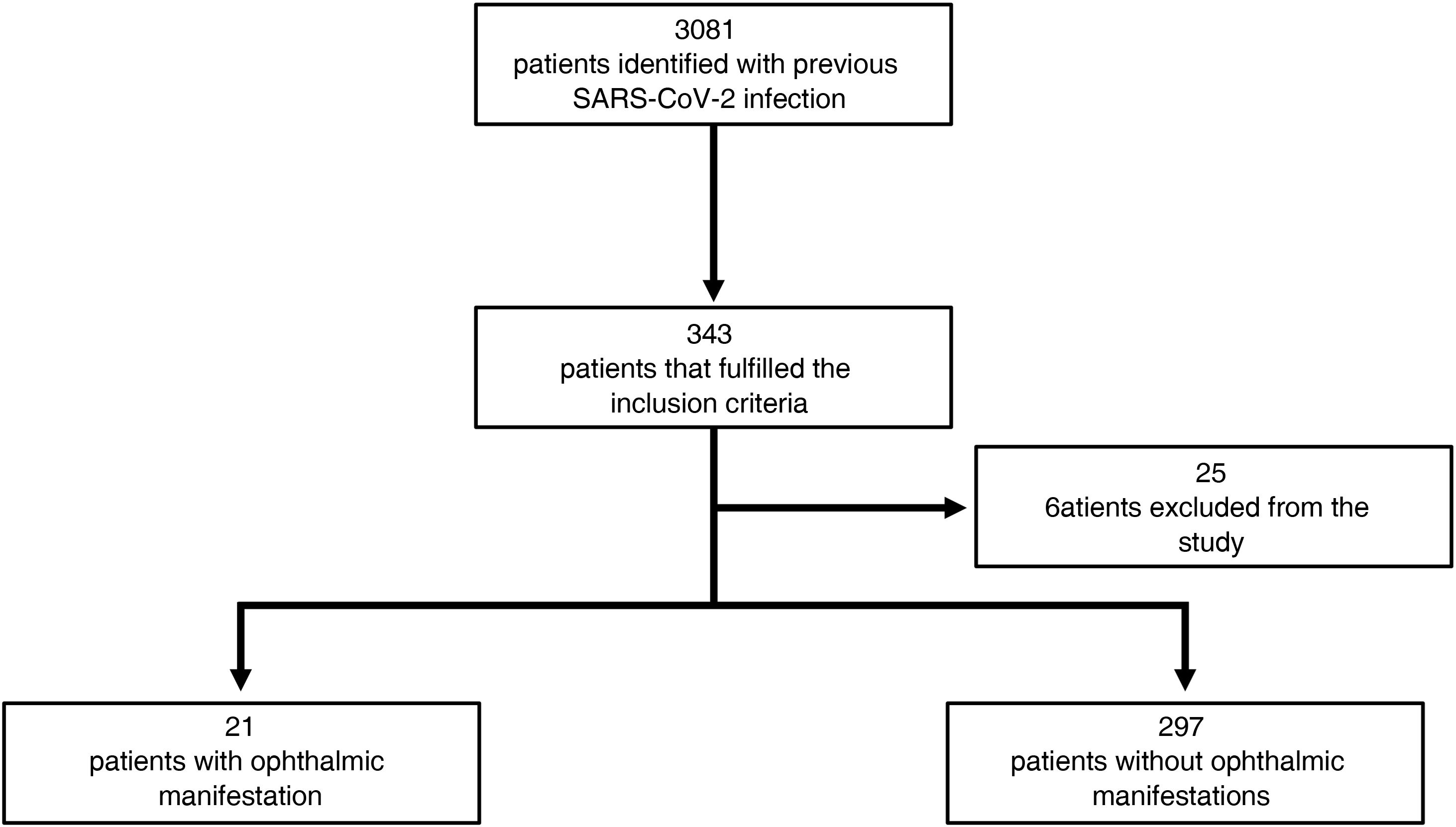
ResultsA total of 3081 patients admitted to the hospital during the period 1 June 2020 to 30 June 2022 had a positive real-time PCR test for SARS-CoV-2. Of these patients, 343 (representative sample determined by non-probability sampling) were included in the study, of which 25 were eliminated due to missing data in the clinical record. Therefore, 318 patients were considered as the sample for this study. The sample was stratified into SARS-CoV-2 infected patients who had (n=21) or did not (n=297) have ophthalmic manifestations (Fig. 1).
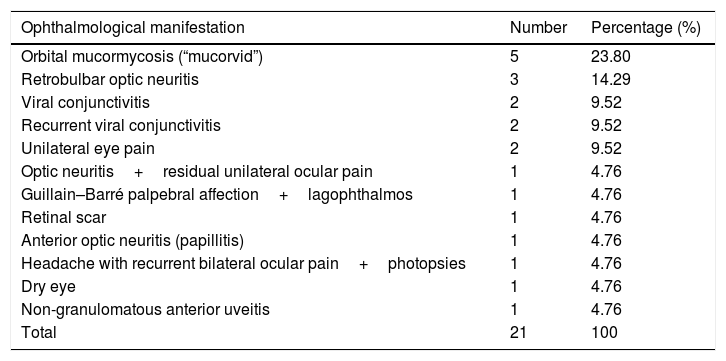
Of the patients infected with SARS-CoV-2 and who had ophthalmic manifestations (n=21), 13 were female (61.90%) and 8 were male (38.10%), with a ratio of 1.625:1. The minimum and maximum age of the patients was 24 years and 79 years, respectively, with a mean of 47.9 years (standard deviation [SD]±15.3) and a median of 46 years. Fourteen of these patients were originally from the state of Veracruz (66.66%), 6 from Tabasco (28.57%) and one from Oaxaca (4.76%). The different ophthalmological manifestations detected in patients with SARS-CoV-2 are shown in Table 1.
Ophthalmic manifestations detected in patients recovered from COVID-19.
| Ophthalmological manifestation | Number | Percentage (%) |
|---|---|---|
| Orbital mucormycosis (“mucorvid”) | 5 | 23.80 |
| Retrobulbar optic neuritis | 3 | 14.29 |
| Viral conjunctivitis | 2 | 9.52 |
| Recurrent viral conjunctivitis | 2 | 9.52 |
| Unilateral eye pain | 2 | 9.52 |
| Optic neuritis+residual unilateral ocular pain | 1 | 4.76 |
| Guillain–Barré palpebral affection+lagophthalmos | 1 | 4.76 |
| Retinal scar | 1 | 4.76 |
| Anterior optic neuritis (papillitis) | 1 | 4.76 |
| Headache with recurrent bilateral ocular pain+photopsies | 1 | 4.76 |
| Dry eye | 1 | 4.76 |
| Non-granulomatous anterior uveitis | 1 | 4.76 |
| Total | 21 | 100 |
In terms of comorbidities, three patients had a diagnosis of type 2 diabetes mellitus (DM2) and hypertension (HAS) (14.28%); one patient had DM2, HAS, obesity, immunodeficiency and cancer (4.76%); one patient had DM2, HAS and other pathologies (4.76%); one patient had only obesity (4.76%); and one patient had only cancer (4.76%). In this study, two (9.52%) of the 21 patients with previous SARS-CoV-2 infection had optic neuritis as an ophthalmic manifestation and, in addition, had been vaccinated against COVID-19.
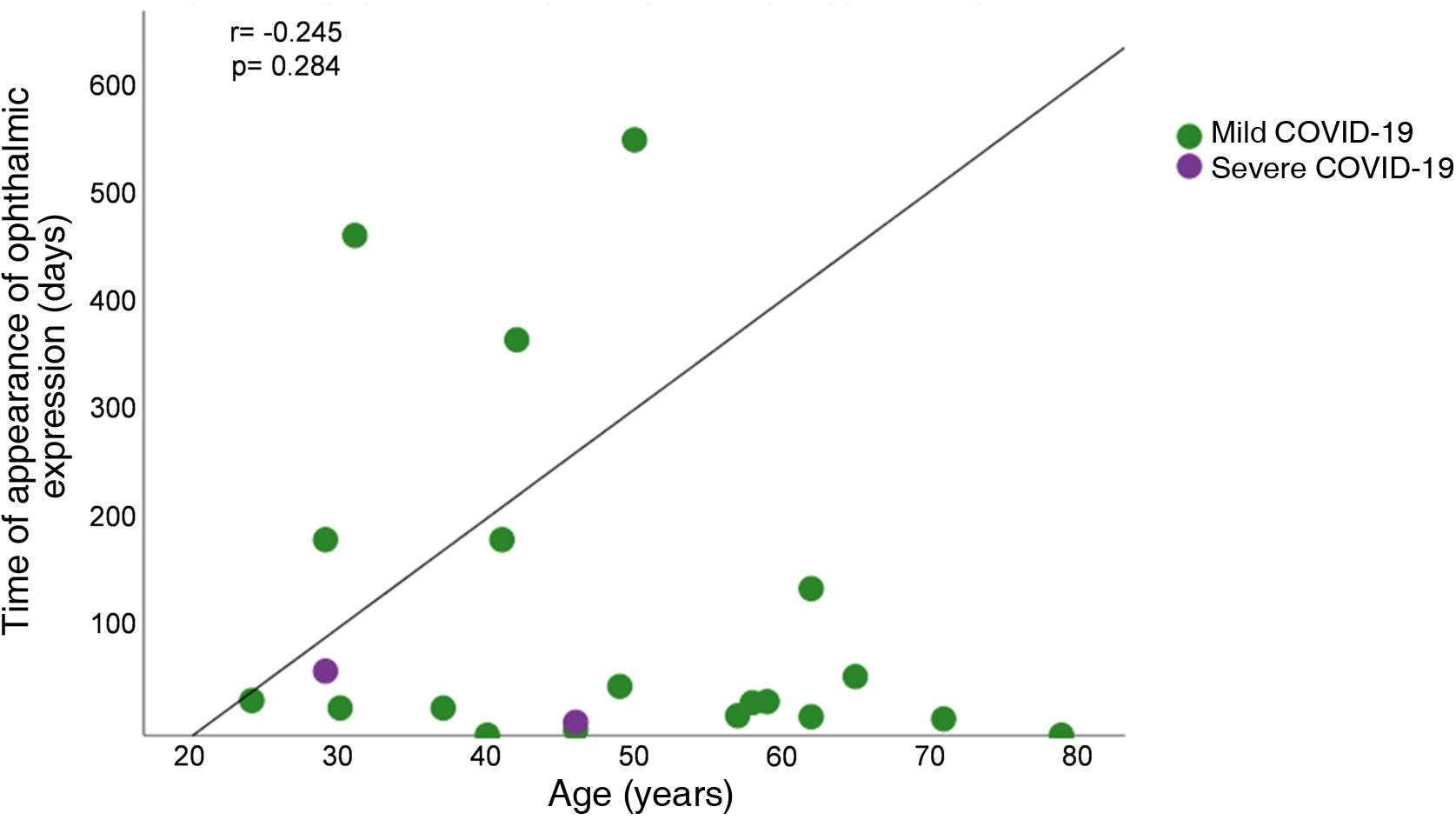
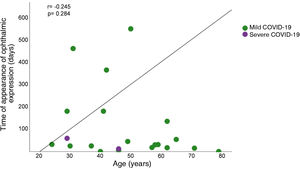
The number of days between the date of the SARS-CoV-2 positive real-time PCR test and the onset of ophthalmic manifestations was also determined. The time to onset of ophthalmic manifestation was estimated with a mean of 106.4 days (SD±158.6 days), with a minimum of 0 days and a maximum of 548 days and a median of 31 days. To determine the correlation between time to onset of ophthalmic manifestation and patient age, a Spearman correlation analysis was performed, which showed an absence of correlation (r=−0.245, p=0.284) (Fig. 2). Interestingly, patients with non-severe COVID-19 had a longer time to onset of ophthalmic manifestation compared to patients with severe COVID-19 (>100 days) (Fig. 2).
Distribution plot depicting the correlation analysis between time to onset of ophthalmic manifestation (days) and age (years) of patients who had COVID-19 and at least one ophthalmic manifestation. Patients are represented with circles to indicate whether they had mild COVID-19 (green) or severe COVID-19 (purple).
To assess the association between SARS-CoV-2 infection and ophthalmological manifestations according to disease severity, the 318 individuals were grouped into patients with severe and non-severe COVID-19. In this regard, 294 patients (92.45%) had non-severe COVID-19, of whom 19 (6.46%) had ophthalmic manifestations. On the other hand, 24 patients (7.55%) had severe COVID-19, but only 2 patients (8.33%) had ophthalmic manifestations. Fisher’s exact test analysis of association determined that there was no statistically significant difference (p=0.665).
DiscussionAlthough the ophthalmological approach to COVID-19 has been neglected since the beginning of the study of the disease, several ophthalmological manifestations have been reported since the beginning of the pandemic. In this regard, extrapulmonary manifestations during COVID-19 are a subject of controversy and interest. In this study, a percentage of ophthalmological manifestations of 6.60% was obtained for a sample of 318 patients who were qRT-PCR positive for SARS-CoV-2. This percentage of patients with ophthalmic manifestations is similar to that observed in studies by Costa et al. (10%), Douglas et al. (1.4%–5.2%) and Sen et al. (0.81%–34.5%).3–5 Among the variety of ophthalmic manifestations described, manifestations similar to those reported in population-based studies were found, as well as in case reports.4–8
Of the 21 patients who had COVID-19 and developed ophthalmic manifestations, a high percentage of mucormycosis was found with orbital manifestation (23.80%) and retrobulbar optic neuritis (14.29%). In our study, the diagnosis of mucormycosis was made on the basis of clinical manifestations, computed tomography and biopsy. Although mucormycosis is an opportunistic fungal infection occurring mostly in immunosuppressed patients, the frequency of this mycosis in patients with severe or non-severe COVID-19 has not yet been fully characterised, as mentioned by Fouad et al.9 Therefore, our finding of patients with non-severe COVID-19 and mucormycosis might be relevant to contribute to the statistics. The mucor complication has been associated with previous infection with SARS-CoV-2, with orbital involvement and rapid deterioration, termed “mucorvid”.9–12 Here, mucor in one patient proved to be non-fatal, while two of the patients with this manifestation required ophthalmic intervention, due to the severity. Patients with optic neuritis were managed in conjunction with the neurology service, resulting in an improvement of the picture and visual acuity, but without regaining previous vision.
The tropism for neurological structures is also evident in the present work, with the reported conditions of optic neuritis, Guillain–Barré with palpebral involvement and ocular pain. In other studies and case reports, optic neuritis and optic atrophy even lead to patients with no light perception, without subsequent visual recovery.13 Conjunctivitis is also described and there is even a case report of recurrent cases. This may be evidence of its tropism for this ocular structure, both in the acute as well as in the subacute and chronic phase. Dry eye is also a condition in patients with COVID-19,4,14,15 which was observed in the patients in this study. Although non-granulomatous anterior uveitis is not common in recovered COVID-19 patients,16 it was detected in one patient 6 months after infection with SARS-CoV-2.
On the other hand, of the 21 patients previously infected with SARS-CoV-2, one patient had a retinal scar of unknown cause detected one year after infection in the study period. In addition, patients included in this study showed specific manifestations as previously described, but also some non-specific ones such as unexplained eye pain and headache with photopsia. Interestingly, patients who were recently vaccinated against SARS-CoV-2 were observed to have optic neuritis. This finding is consistent with studies by Abdin et al., Bolleta et al. and Chen et al.16–18
Some other described manifestations such as retinal vascular occlusions, optic atrophy, ophthalmoplegia, choroidal conditions, panuveitis, pigmentary disorders, retinal serous detachments, among others, were not found in the present study. However, all ophthalmological manifestations require priority attention in the multidisciplinary management of COVID-19.
Although in the present study no significant association was found between ophthalmological manifestations and severe COVID-19 (p>0.05), it is important to consider the visual functional impairments, which in some of the patients remain and do not have a good prognosis in the short, medium or long term. This study has some limitations: (1) the study was conducted in a single tertiary hospital centre and with a small sample; (2) a large percentage of the SARS-CoV-2 positive patients did not return to the hospital for their subsequent assessments; (3) patients were not followed up to obtain more information on the development and outcome of ophthalmic manifestations; and (4) during the assessment of patients with COVID-19, ophthalmic manifestations may not have been explored and perhaps for this reason they did not receive adequate ophthalmic care.
It is important to consider that, due to underreporting and underestimation of these clinical manifestations, it is likely that they are not associated with previous SARS-CoV-2 infection. Therefore, this study has the strength to report that, although infrequent, patients with COVID-19 may develop ophthalmic manifestations.
Similar studies with a larger sample size and an appropriate approach could provide more conclusive results to establish an ophthalmic care protocol for patients infected or previously infected with SARS-CoV-2.
ConclusionsThe results of this study suggest an absence of statistically significant association between patients recovered from severe COVID-19 and ophthalmological manifestations (p>0.05). However, further studies with a larger sample size are required to confirm these findings.
FundingThis research has not received specific support from public sector agencies, the commercial sector or non-profit organisations.
Conflict of interestNo conflicts of interest were declared by the authors.
The authors would like to thank all the health workers, doctors, nurses and support staff who worked in the UMAE, H. E. No. 14, Centro Médico Nacional Adolfo Ruiz Cortines, IMSS Veracruz, who were working together against COVID-19.