Full-thickness macular hole is a rare complication of macular telangiectasia type 2, and its treatment is still controversial. A patient with a full-thickness macular hole secondary to macular telangiectasia type 2 underwent vitreoretinal surgery with a plasma rich in growth factors membrane in the macular hole. At the sixth month of follow-up, anatomical and functional improvements were achieved, with no adverse effects. Plasma rich in growth factors is a new option, with advantages due to its biological properties that achieves good results in terms of safety and effectiveness in the surgical treatment of macular hole.
El agujero macular de espesor total es una complicación rara de la telangiectasia macular tipo 2, y su tratamiento es aún controvertido. Una paciente con esta entidad fue llevada a cirugía vitreorretiniana con aplicación de membrana de plasma rico en factores de crecimiento sobre el agujero macular. Al sexto mes de cirugía se logró mejoría anatómica y funcional, sin efectos adversos asociados. El plasma rico en factores de crecimiento es una alternativa nueva en el tratamiento quirúrgico del agujero macular atípico y/o persistente, que logra buenos resultados en términos de seguridad y efectividad, debido a sus propiedades biológicas.
Macular telangiectasia type 2 (Mac Tel 2) is a bilateral disease of unknown cause, with characteristic alteration of the macular capillary network and neurosensory atrophy1. Full-thickness macular hole (FTMH) secondary to Mac Tel 2 is a rare complication initially described in 2006, the pathogenesis of which is uncertain2. It is thought to be due to alteration of the endothelial wall and its metabolism, leading to increased permeability and chronic deficits in metabolism and degeneration of Müller cells. This nutritional deficit in addition to atrophy is what has been proposed to lead to weakness and consequent formation of the hole, and it is still debated whether vitreomacular traction may contribute to its development3. A recent study of patients treated with pars plana vitrectomy (PPV) had moderately successful results in the management of this pathology4.
Plasma rich in growth factors (PRGF) is a substance with biological properties for tissue regeneration and modulation of inflammation. Its effectiveness depends on platelet concentration, platelet activation and the absence of leukocytes5.
The case of a patient with FTMH secondary to Mac Tel 2 is presented, who was successfully treated with the innovative PRGF membrane technique.
Case reportFemale, 70, with a history of systemic arterial hypertension and refractive surgery performed 20 years ago, who consulted for blurred vision in both eyes (BE) of 9 months of evolution. Corrected visual acuity (CVA) of the right eye (RE) was 20/200 and left eye (LE) 20/70 with Snellen chart. Examination revealed incipient cataract BE, rest of biomicroscopy without alterations. Fundus BE: normal disc, hyperplasia of the retinal pigment epithelium (RPE) parafoveal temporal retina, adherent retina. RE: FTMH, LE: macular pseudohole.
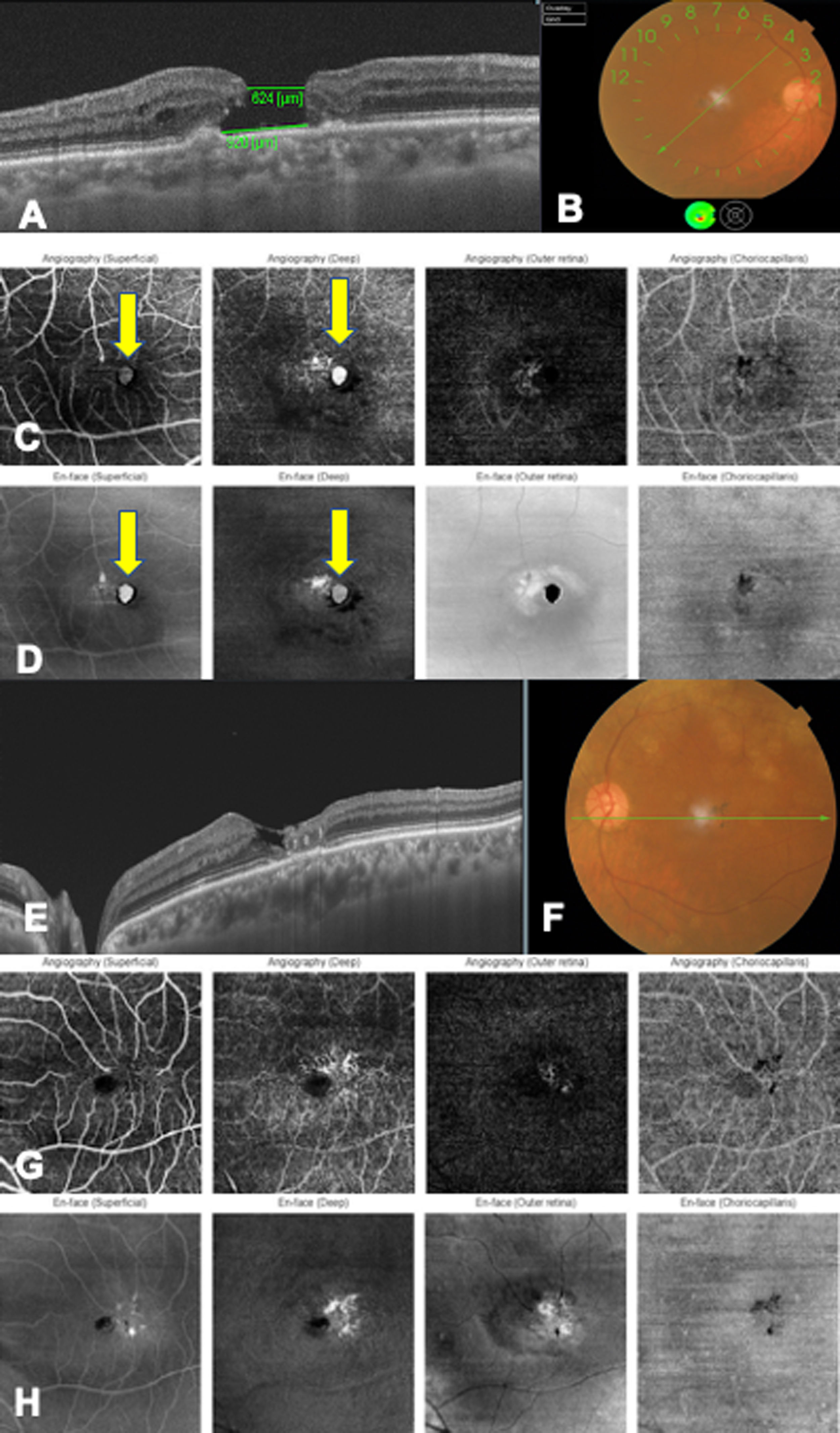
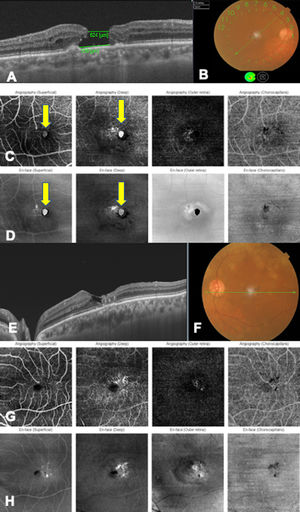
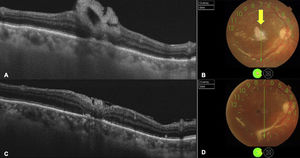
Optical coherence tomography angiography (OCT-A) (DRI OCT-1 Triton, Topcon, USA) showed Mac Tel in BE, FTMH in RE and cavitations in LE (Fig. 1). Due to the characteristics of the case, the visual and anatomical prognosis with conventional treatment was lower, so the new surgical technique was proposed.
Multimodal BE image.
A. Macular OCT of RE showing full-thickness macular hole with measurements of the hole (inner diameter 624 μm, and basal diameter 920 μm) without vitreous traction at the edges of the hole. B. Color fundus photograph shows artifact in foveal area, migration of temporal RPE to fovea. C. OCT angiography shows circular hyperreflective lesion corresponding to the macular hole (yellow arrow), nasal to telangiectatic vessels. D. En-face image shows the same hyperreflective lesion nasal to the macular telangiectasias (yellow arrow). E. OCT of the LE shows alteration of the foveal architecture, hyperreflective lesions in intermediate layers, loss of the outer segments of the temporal photoreceptors to the fovea, foveal hyperreflective lesions corresponding to cavitations and thickened choroid. F. Color fundus photograph shows artifact in foveal area, migration of temporal RPE to fovea. G. OCT. Angiography shows temporal telangiectasias to the fovea in the superficial and deep plexuses. H. En-face image shows temporal hyperreflective lesions to the fovea.
The PRGF membrane was prepared according to the Endoret® system (BTI Biotechnology Institute, Alava, Spain). Blood was collected from the patient in tubes, then centrifuged, obtaining 3 components: fraction 1 (F1) with platelet number similar to peripheral blood, fraction 2 (F2) with 3 times higher concentration of platelets and lower concentration of erythrocytes, fraction 3 (F3) whole blood. To obtain the PRGF membrane shape, 2 mm of F2 was obtained and activated with 10% calcium chloride, then incubated at 37 °C for 30 min until a clot was achieved, which was flattened with a mold.
In the same procedure, after cataract extraction and intraocular lens implantation, PPV with internal limiting membrane peeling was performed, the PRGF membrane was introduced through a trocar and placed as a plug inside the FTMH. Subsequently, endocular silicone was left as a buffering agent, because the patient had to travel by plane to her city of residence.
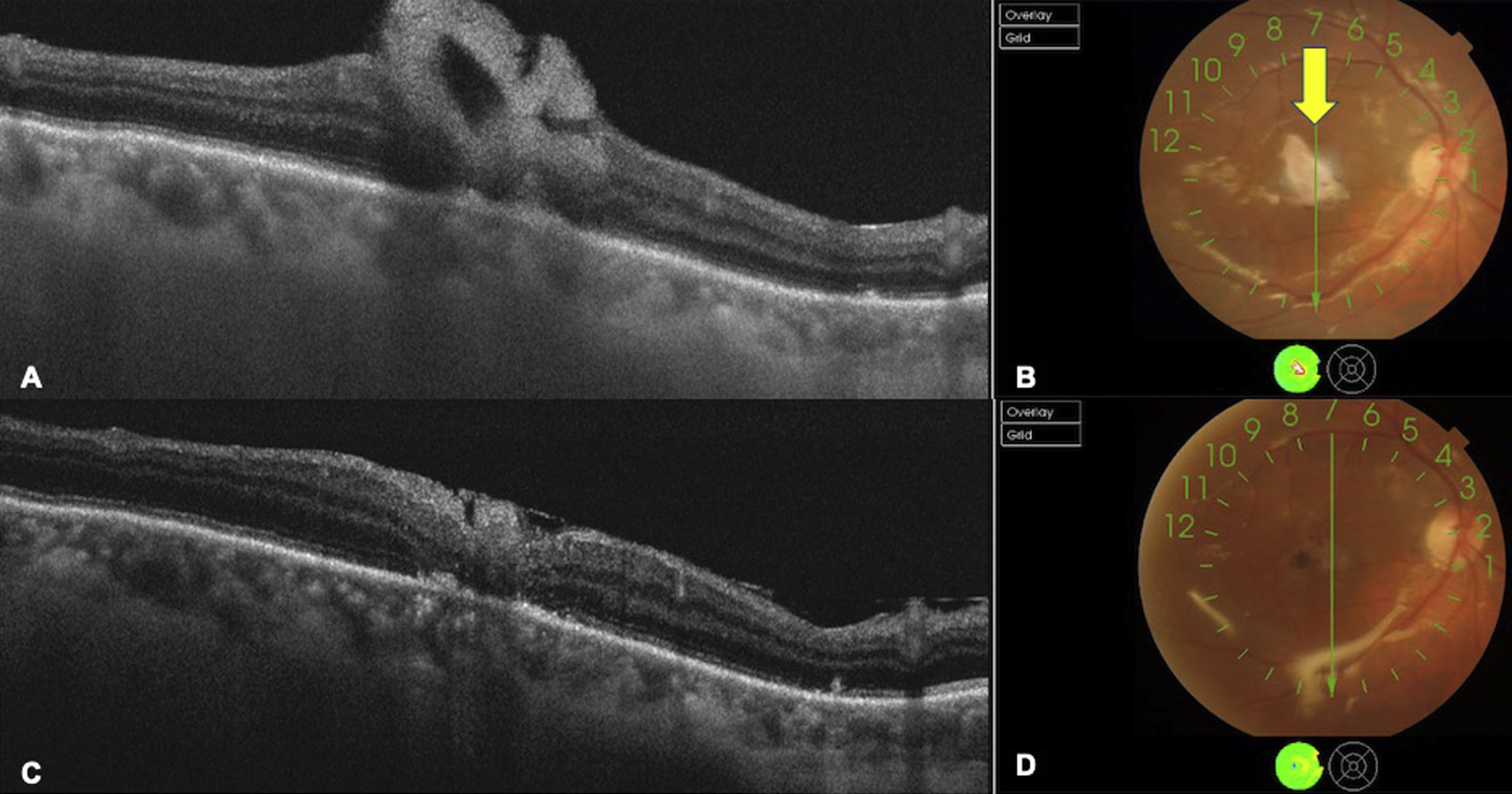
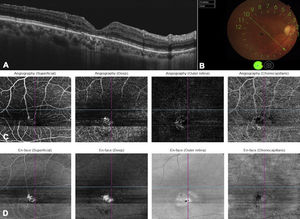
On the first postoperative day, the PRGF membrane was properly positioned (Fig. 2). The silicone oil was removed 4 months after surgery. At the sixth month of follow-up, anatomical closure of the MH was achieved, with visual acuity with RE correction of 20/100 (Fig. 3), with no evidence of FTMH recurrence or associated adverse events.
OCT postoperative RE findings.
A. OCT of the first postoperative day showing hyperreflective band covering the macular hole. B. Color fundus photograph shows silicone in vitreous cavity and PRFG membrane (yellow arrow) covering the macular hole. C. 10-day postoperative OCT shows smaller hyperreflective area and closure of the macular hole. D. Color fundus photograph shows silicone in vitreous cavity and macular hole closure.
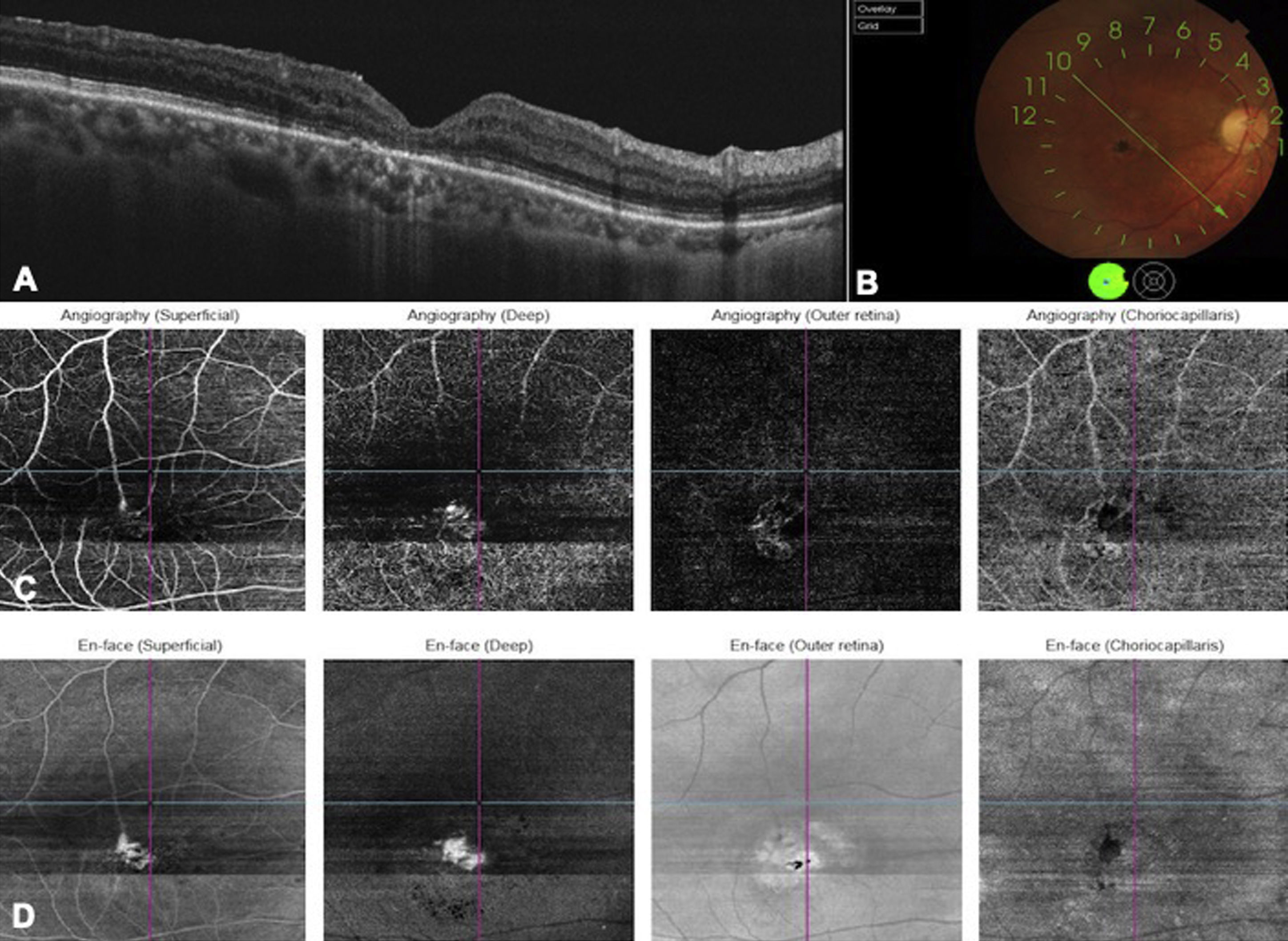
Multimodal image of postoperative RE findings.
A. OCT B-scan showing macular hole closure with incomplete regeneration of the outer retinal layers. B. Color photograph shows migration of the temporal RPE to the fovea and closed macular hole. C. OCT-Angiography reveals resolution of the hyperreflective lesion seen preoperatively and only telangiectasias are seen in the superficial and deep vascular plexus. D. En-face image shows hyperreflective lesions which correspond to macular telangiectasias, however, without the hyperreflective lesion seen preoperatively.
Mac Tel 2 is a disease of unknown etiology with characteristic macular capillary disorders and neurosensory atrophy; it has recently been described as an autosomal dominant inherited disease with reduced penetrance. The prevalence is 0.1% in people over 40 years of age1.
Currently, treatment for Mac Tel 2 in the absence of retinal neovascularization is merely supportive. Studies have been published with no demonstrable effectiveness in controlling the disease with macular grid laser photocoagulation, photodynamic therapy or intravitreal injections of anti-VEGF1. Similarly, a recent retrospective study by Miller et al. confirmed that in patients with TMA due to Mac Tel 2 and despite improved OCT findings no statistical difference was observed in visual acuity in patients who underwent conventional PPV compared to those who did not undergo surgery4.
In 2010, Gregori and Flynn reported 2 cases, one of which reopened during follow-up6. Charbel Issa et al. established the differences in the success rate of FTMH closure related to Mac Tel and suggest the coexistence of factors other than traction that may influence it1.
The PRGF preparation is characterized by a moderate concentration of platelets, activated platelets and lack of leukocytes5. The absence of leukocytes is because they synthesize matrix metalloproteinases, free radicals and proinflammatory cytokines that hinder the process of tissue regeneration7. This PRGF technology is an alternative treatment of autologous origin in ophthalmology with active biological properties that promote tissue regeneration, modulate healing response and anti-inflammatory properties.
PRGF has been successfully used in ophthalmology in patients with sequelae of dry eye and complex FTMH5,7. On the other hand, in 2015 Figueroa et al. report a prospective case series of 7 patients with myopic FTMH who underwent PPV with removal of the internal limiting membrane and application of PRGF liquid glue over the foramen, showing anatomical improvement in 100% of cases. However, no statistically significant difference was found in the improvement of CVA8. Sánchez-Ávila et al., reported a patient with high myopia who underwent a conventional surgical procedure without PRGF and presented with recurring FTMH 3 months later. A second surgery with PRGF membrane showed a successful complete closure of the MH, without recurrence, and VA was stable during the 6 months of follow-up5. Although few articles use PRGF membrane, those that do show good results5,7.
The proposed mechanism by which the PRGF membrane achieves TMA closure is due to the trophic actions exerted by growth factors, in addition to promoting the activation of Müller cells, serving as a bed for cell growth, regeneration of the affected tissue that modulates the healing response and decreases the inflammatory process5,7,8.
Tha authors consider the use of PRGF membrane is promising when looking for a stable improvement of VA, despite having only isolated case reports. Some advantages of PRGF membrane in contrast to its liquid form is that it remains longer in the area of interest, thus not only filling the area of the hole, but also maintaining a continuous release of growth factors, which stimulate not only the hole closure but also the reconstitution of the inner and outer retinal layers. On the other hand, in liquid form, it does not remain for a long time and loses its effect within a few hours. A disadvantage with the technique may be the difficulty in handling the membrane intraoperatively to place it in the hole and that in the early postoperative period it comes out of the hole. If we compare the liquid form of PRGF vs. inverted internal limiting membrane no significant differences can be observed, although the few studies that exist do find superiority with the PRGF membrane5,7.
Figueroa et al. found adequate anatomic closure with PRGF glue although with no impact on the final VA. Meanwhile, with PRGF membrane presentation, successful results were observed in both VA and anatomical closure of FTMH. Concordantly, Arias et al. reported 2 cases of persistent FTMH in which complete closure was achieved with stable visual improvement during a 12-month follow-up7, a result consistent with the present case.
In conclusion, in the knowledge of the authors, this is the first case report of FTMH secondary to Mac Tel 2 treated with the PRGF membrane technique. Since this is a challenging foramen both for size and concurrent disease such as Mac Tel 2, the main objective was to achieve anatomical and functional success in the first intervention. These results indicate that this is a valid, safe and effective alternative to manage this type of disease. However, the literature search evidenced the lack of clinical trials evaluating the PRGF membrane as an alternative treatment for FTMH of difficult cases such as those greater than 600 μm, traumatic, persistent and myopic, among others, and their long-term results.
Conflict of interestNo conflicts of interests were declared by the authors.
Please cite this article as: Rangel CM, Blanco NA, Pedraza-Concha A, Gomez MA, Parra MM, Arias JD. Plasma rico en factores de crecimiento como tratamiento para agujero macular de espesor total secundario a telangiectasia macular tipo 2. Arch Soc Esp Oftalmol. 2022;97:219–223.