A 78-year-old man presented with a 2-week history of decreased vision in the right eye (RE). Ocular history included uncomplicated cataract surgery in the RE 2 years earlier. Gonioscopy revealed a retained small nuclear fragment (sNF) in the anterior chamber (AC) and OCT showed macular edema (ME). The NF was fragmented with a YAG laser.
DiscussionAC retained NF resulted in ME and reduced visual acuity. We recommend gonioscopy in cases of reduced visual acuity and history of phacoemulsification. ME and reduced vision may be reversed by removing the NF with YAG laser.
Varón de 78 años con pérdida de visión en el ojo derecho (OD) de 2 semanas de evolución. En los antecedentes destaca cirugía de catarata en el OD 2 años antes. La gonioscopia demostró un fragmento nuclear pequeño (FNp) en la cámara anterior (CA) y la OCT un edema macular (EM). Con YAG se fragmentó el FN.
DiscusiónLos FN en la CA pueden producir EM y visión reducida. Con pérdida de visión y con historia de facoemulsificación se recomienda una gonioscopia. El EM y la pérdida de visión se pueden revertir fragmentando el FN con láser YAG.
Nuclear fragments (NF) retained in the anterior chamber (AC) after cataract surgery can cause persistent chronic inflammation, which manifests early, or it may occur much later (years later); therefore, neither patient nor ophthalmologist relate it to the previous surgery.1–4 NF can stay hidden in paracentesis, in the crypts or behind the iris.1–4 This is a report on a patient with a small nuclear fragment (sNF) retained in AC with sharp macular edema (ME) 2 years after cataract surgery.
Clinical caseA 78-year-old male is seen for painless loss of vision in OD with 2 weeks of progression. History included syringomyelia, a recent ischemic stroke and uncomplicated phacoemulsification with intraocular lens implant (IOL) in the posterior chamber (PC) in OD, 2 years prior.
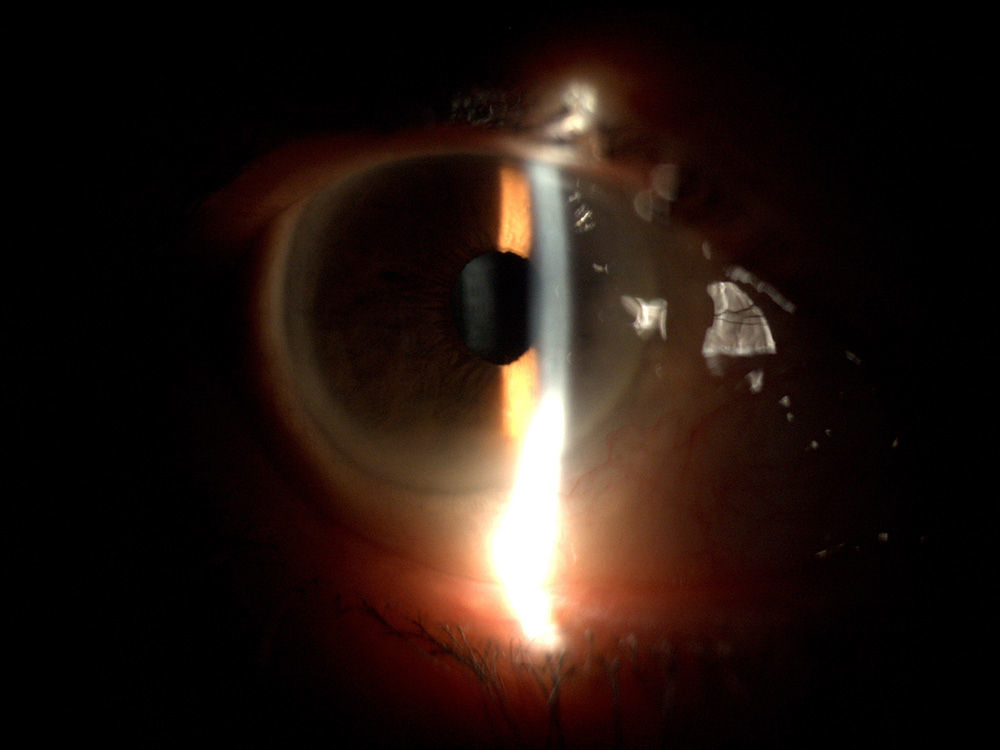
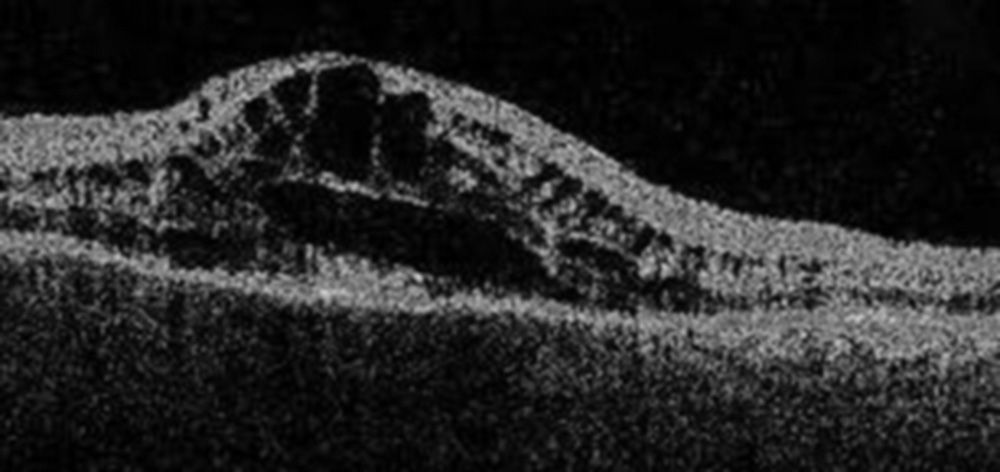
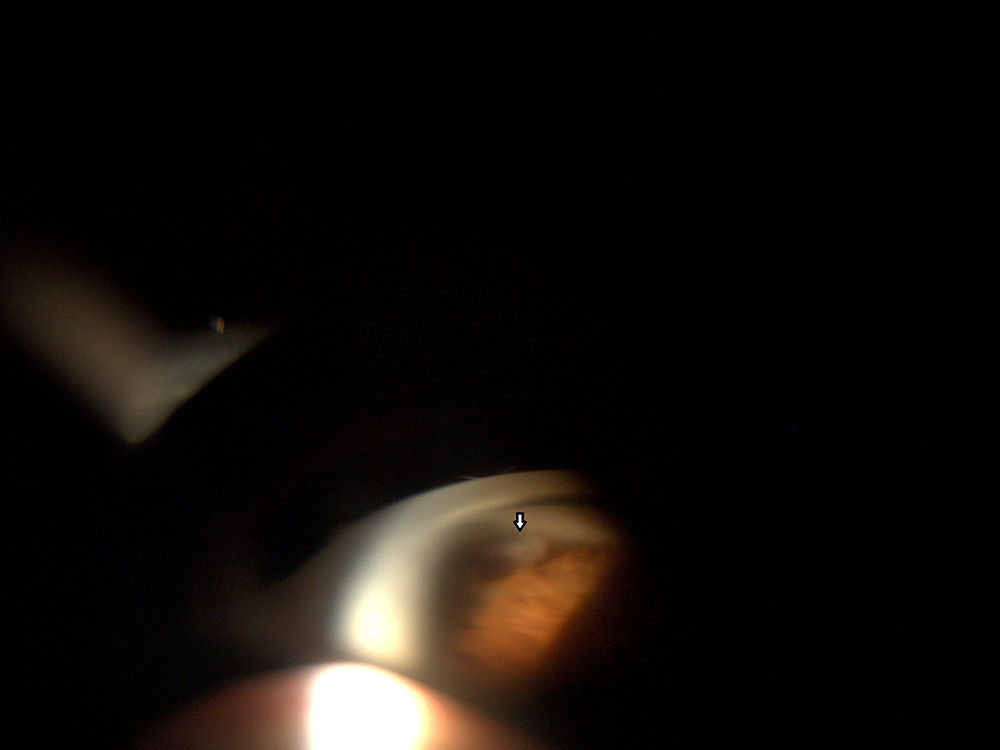
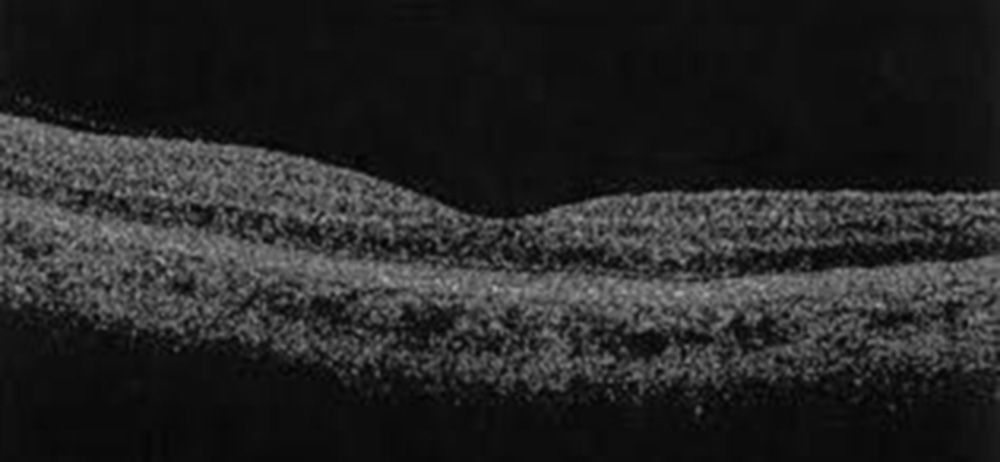
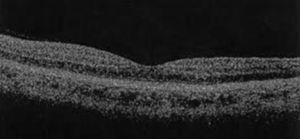
Best visual acuity (VA) in OD was 0.05 (it was 0.8 in the last examination one year prior). Intraocular pressure was 20mmHg. Previous biomicroscopic analysis only detected slight iritis (Fig. 1). Mydriasis examination showed IOL in sac with both haptics in situ and intact PC. The fundus showed ME of cystic appearance, confirmed by OCT (3D OCT-2000, Topcon) (Fig. 2). Gonioscopy revealed a sNF retained in the lower angle (Fig. 3). It was treated with 1% prednisolone acetate, 4 times daily and ranibizumab. One month later, patient's VA was hand motion, and had no corneal edema; however, ME was more intense. The patient's bad condition contraindicated surgical extraction; therefore, a YAG laser was used to fragment the NF into tiny particles. Two months later, VA in OD was 0.7 and ME had disappeared (Fig. 4).
Optical coherence tomography of the right eye two months after YAG laser. Linear scan, same as in Fig. 2. Resolution of macular edema.
Although the presence of vitreous sNF may not be uncommon due to the large number of phacoemulsifications, there are very few reports of NF retention in the AC with clinical manifestations years after the surgery.1–4 Retained NF are responsible for early or late, low-grade chronic intraocular inflammation. Kang et al.1 published a case of a patient with severe corneal edema and moderate uveitis 15 years after cataract surgery due to NF retained in the AC. Pandit et al.2 reported an acute corneal edema due to NF retained in the AC 8.5 years after surgery without complications. Bohigian et al.3 published the case of a patient with corneal edema and ME one month after surgery that were only resolved with surgical removal of the fragment. Hui et al.4 studied 16 patients with NF retained in the AC; 31.3% of them (four patients) had no corneal edema, only mild inflammation of the anterior segment, but showed 43.7% loss of vision (between 0.6 and hand motion). 62.5% (10 patients) had visible pieces under slit lamp; the remaining 37.5% (five patients) underwent gonioscopy as a diagnostic method. The fragment was removed surgically in all cases. The patient described in this study remained asymptomatic for 2 years, was not myopic and had no miotic pupil during surgery. The patient did no complain of pain episodes or redness, although he had low-grade chronic inflammation in the AC. He was seen for a severe, sudden and painless loss of vision due to an ME, without an ocular or systemic cause to justify it. Slit lamp examination was not diagnostic. Gonioscopy was essential to identify sNF. Most likely, it lodged behind the iris during surgery and abruptly moved to the AC two years after phacoemulsification. Another explanation is that the fragment remained sequestered in PC or IOL, protected from the aqueous humor and, due to capsular contracture, it moved to the AC, producing a minimal chronic inflammatory reaction.1 Occasionally, an NF will lodge in the paracentesis or incision and go unnoticed.1–4 NF extraction is the primary treatment in all cases1–4; however, the systemic disease of our patient contraindicated surgery. With the YAG laser5 we were able to reduce the NF to tiny pieces that were eliminated through the trabecular meshwork or were not sufficiently antigenic to trigger an inflammatory reaction. What is difficult to explain is why the patient had no corneal edema at any time but did have ME. This case reflects a high index of suspicion by the ophthalmologist of an NF retained in the AC in patients with late ME lacking a systemic cause, with a history of phacoemulsification and the need for careful gonioscopy.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Asensio-Sánchez VM, Ajamil S, Ramoa-Osorio R, Trujillo-Guzmán L. Edema macular agudo 2 años después de la cirugía de catarata por un fragmento nuclear retenido. Arch Soc Esp Oftalmol. 2014;89:272–274.