The latest global health threat is the ongoing outbreak of respiratory disease, which was named COVID-19 and multiple ever-evolving neurological complications have since been reported. We present the case of a patient with a bilateral tonic pupil in the postinfectious context of COVID 19. Brain magnetic resonance imaging and laboratory tests were normal, a 0.125% pilocarpine test confirmed the diagnosis.
La última amenaza para la salud a nivel mundial es el continuo brote de la enfermedad respiratoria, que recibió el nombre de COVID-19 y desde entonces se han reportado múltiples complicaciones neurológicas que están en constante evolución. Presentamos el caso de un paciente con pupila tónica bilateral en el contexto posinfeccioso de COVID 19. La resonancia magnética cerebral y los estudios analíticos fueron normales, una prueba de pilocarpina al 0,125 % confirmó el diagnóstico.
In late December 2019, Chinese public health authorities reported several cases of acute respiratory syndrome in Wuhan City, Hubei Province, China.1 A new coronavirus was soon identified as the main causative agent. The virus was officially called “Severe Acute Respiratory Syndrome Coronavirus 2” (SARS-CoV-2), it is highly contagious and has quickly become a global health risk, and due to its rapid expansion, it was declared a pandemic by the WHO on March 11th, 2020. In our country, the first case was reported on March 6th of the same year.2 Different related neurological symptoms have been reported, such as headache, dizziness, impaired consciousness and anosmia, along with some related syndromes such as Miller-Fisher, Guillain-Barré (GBS) syndrome, mono or cranial polyneuritis, which have broadened the neurological spectrum.3 We introduce the case of a bilateral tonic pupil which arose in the post-infectious context of CoVid 19. After explaining to the patient, written informed consent was obtained.
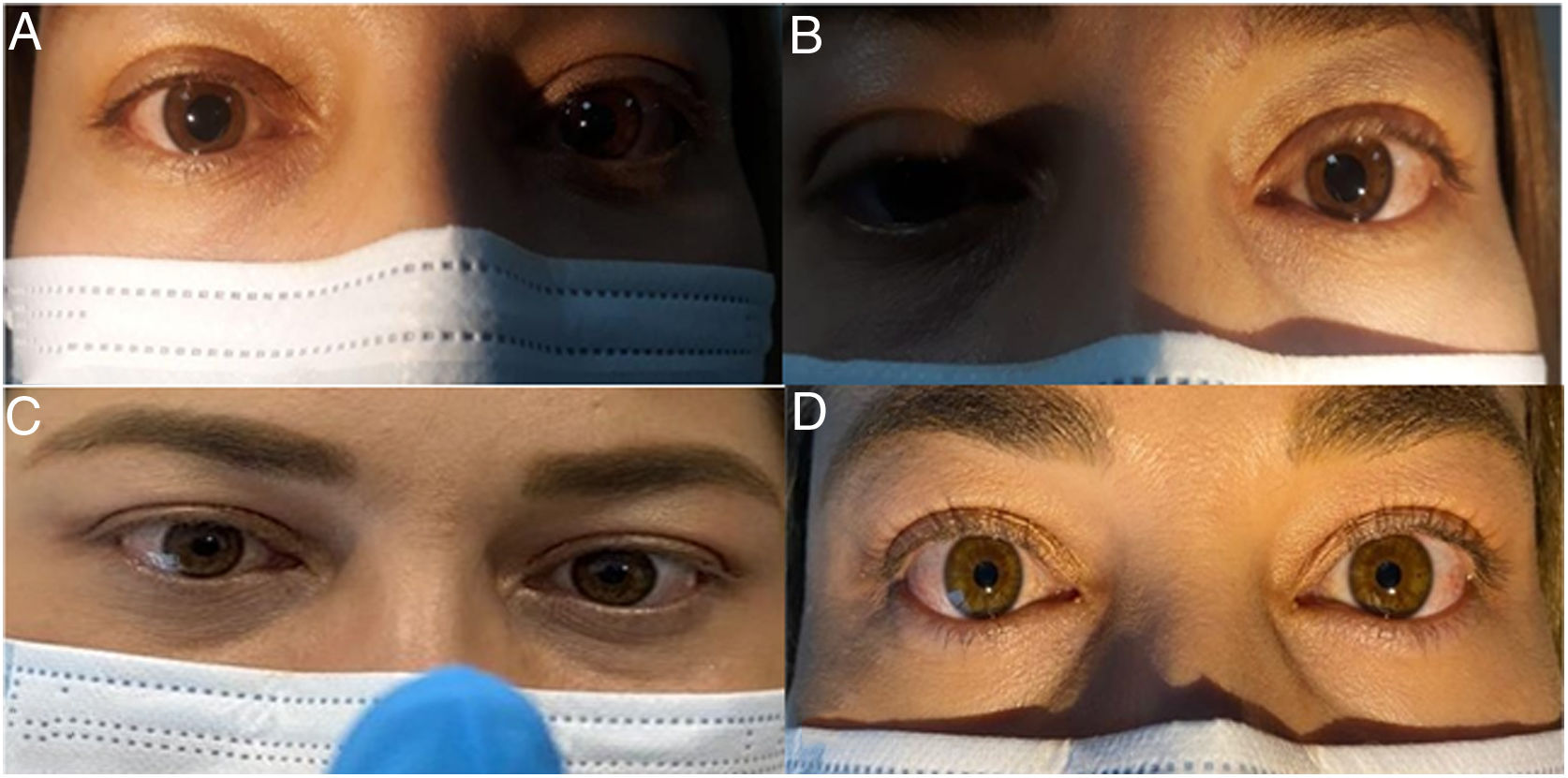
Case report36-year-old female patient who was admitted to our ophthalmology service, reporting a 3-day picture of pupillary dilation in both eyes and blurred vision. She did not report pain with eye movements or alteration of color vision. The patient was in the recovery phase from an infection documented with a positive molecular test by PCR for SARS-CoV-2 17 days ago and presented neurological sequelae due to peripheral vertigo, persistent anosmia and headache. Her brain MRI was normal. The ophthalmological examination revealed visual acuity: OD SC 20/400 CC 20/30 OS SC 20/200 CC 20/20; in addition, it showed a bilateral mydriatic pupil of approximately 8 mm in diameter, not reactive to light, but slowly reactive to convergence. Her neurological exam, including deep reflexes, balance, strength, and tone were normal. Blood tests were normal, including thyroid, kidney, liver function, serology for syphilis, HIV, and Lyme disease; and the severity criteria for Covid 19 showed values within normal ranges. CSF analysis was normal. A 0.125% diluted pilocarpine test was performed, which showed pupillary constriction after the first instillation with a marked effect at 15 min, both pupils becoming equal in size and confirming the diagnosis of a tonic pupil (Fig. 1).
DiscussionAdie's pupil is the result of an injury to postganglionic parasympathetic neurons, which are found from the ciliary ganglion to the pupil sphincter muscle and the ciliary muscle, resulting in the absence of the photomotor reflex, but with a tonic response of the pupil to near vision.4
Patients may also show decreased deep tendon reflexes in complete Holmes-Adie syndrome, as well as autoimmune diseases, paraneoplastic entities, connective tissue diseases, and post-infectious conditions (i.e., syphilis, Lyme disease, or the virus family herpes).5 In most cases the commitment is unilateral. Bilateral tonic pupils have been observed in patients with diabetes, alcoholism, syphilis, dysautonomia associated with cancer, and amyloidosis.5
Several reports have emerged on Guillain-Barré syndrome and Miller Fisher syndrome, pointing to an antibody-mediated postinfectious mechanism for associated cranial neuropathies. Acute cerebrovascular disease appears to be the most common severe neurological manifestation of COVID-19 and occurs in 2.8% of patients, mainly ischemic stroke, but intracerebral hemorrhages and venous sinus thrombosis also occur. An initial study of the neurological manifestations of COVID-19 in China described a high prevalence of neurological symptoms: 30.2% overall, including nonspecific viral symptoms, such as myalgia, but also vision changes. Three presumed main mechanisms of neurological injury have been proposed: direct viral invasion of the central nervous system, endothelial dysfunction, and a neurotoxic effect due to excessive inflammation and cytokine release.6
Our case presents a bilaterally compromised tonic pupil and is interpreted as secondary to an immune-mediated manifestation of COVID-19 infection that was confirmed by pupillary constriction after administration of 0.125% pilocarpine. As reported in the first reported case of trochlear mononeuropathy and tonic pupil that occurs shortly after a SARS-CoV-2 infection with a supposed immune-mediated mechanism,7 we believe that after the systemic inflammatory compromise triggered by the virus and the window period There is a characteristic immunological reaction with certain antigenic determinants of the organism that leads us to consider an immune-mediated manifestation related to COVID-19.
In conclusion, we present the case of the bilateral tonic pupil after a SARS-CoV-2 infection with a presumed immune-mediated mechanism. Post-infectious complications that can also affect vision should be monitored to examine in a close manner the mechanisms by which the infection triggers neuro-ophthalmic manifestations.
Financial supportNone.
Conflicts of interestNo conflicting relationship exists for any author.
Please cite this article as: Quijano-Nieto BA, Córdoba-Ortega CM. Pupila tónica después de la infección por COVID-19. Arch Soc Esp Oftalmol. 2021;96:353–355.