The World Health Organization has emphasized the importance of a multidisciplinary approach between professionals to promote cooperation among professionals and improve health care.1 The purpose of this study was to evaluate the effect of a 2-day multidisciplinary boot camp on healthy lifestyle habits, health markers, and disease knowledge, and on mental health in patients with metabolic syndrome (MetS), over for a 6-month follow-up period.
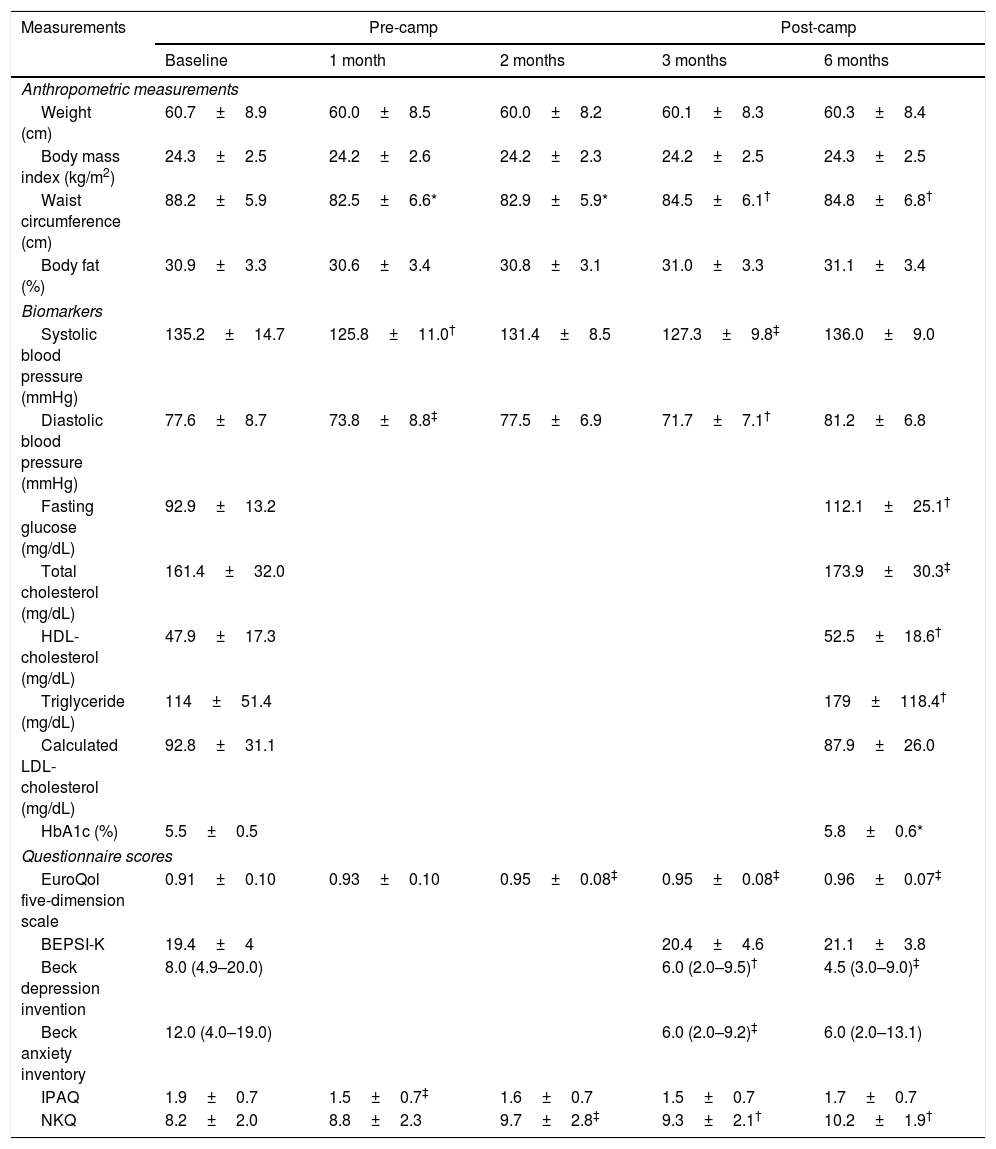
Twenty-nine participants with MetS patients attended at a 2-day multidisciplinary boot camp held on May 23–24, 2015. Our team comprised of doctors, nurses, dieticians, exercise instructors, health administrators, and social workers participated in a multidisciplinary education program for the prevention and management of MetS. It consisted of lectures, hands-on exercises, group discussions, exercise, cooking classes, and quiz tests. Blood tests and questionnaires shown in Table 1 were assessed pre-camp and 1-, 2-, 3-, and 6-months post-camp.
Changes in measurements pre- and post-camp.
| Measurements | Pre-camp | Post-camp | |||
|---|---|---|---|---|---|
| Baseline | 1 month | 2 months | 3 months | 6 months | |
| Anthropometric measurements | |||||
| Weight (cm) | 60.7±8.9 | 60.0±8.5 | 60.0±8.2 | 60.1±8.3 | 60.3±8.4 |
| Body mass index (kg/m2) | 24.3±2.5 | 24.2±2.6 | 24.2±2.3 | 24.2±2.5 | 24.3±2.5 |
| Waist circumference (cm) | 88.2±5.9 | 82.5±6.6* | 82.9±5.9* | 84.5±6.1† | 84.8±6.8† |
| Body fat (%) | 30.9±3.3 | 30.6±3.4 | 30.8±3.1 | 31.0±3.3 | 31.1±3.4 |
| Biomarkers | |||||
| Systolic blood pressure (mmHg) | 135.2±14.7 | 125.8±11.0† | 131.4±8.5 | 127.3±9.8‡ | 136.0±9.0 |
| Diastolic blood pressure (mmHg) | 77.6±8.7 | 73.8±8.8‡ | 77.5±6.9 | 71.7±7.1† | 81.2±6.8 |
| Fasting glucose (mg/dL) | 92.9±13.2 | 112.1±25.1† | |||
| Total cholesterol (mg/dL) | 161.4±32.0 | 173.9±30.3‡ | |||
| HDL-cholesterol (mg/dL) | 47.9±17.3 | 52.5±18.6† | |||
| Triglyceride (mg/dL) | 114±51.4 | 179±118.4† | |||
| Calculated LDL-cholesterol (mg/dL) | 92.8±31.1 | 87.9±26.0 | |||
| HbA1c (%) | 5.5±0.5 | 5.8±0.6* | |||
| Questionnaire scores | |||||
| EuroQol five-dimension scale | 0.91±0.10 | 0.93±0.10 | 0.95±0.08‡ | 0.95±0.08‡ | 0.96±0.07‡ |
| BEPSI-K | 19.4±4 | 20.4±4.6 | 21.1±3.8 | ||
| Beck depression invention | 8.0 (4.9–20.0) | 6.0 (2.0–9.5)† | 4.5 (3.0–9.0)‡ | ||
| Beck anxiety inventory | 12.0 (4.0–19.0) | 6.0 (2.0–9.2)‡ | 6.0 (2.0–13.1) | ||
| IPAQ | 1.9±0.7 | 1.5±0.7‡ | 1.6±0.7 | 1.5±0.7 | 1.7±0.7 |
| NKQ | 8.2±2.0 | 8.8±2.3 | 9.7±2.8‡ | 9.3±2.1† | 10.2±1.9† |
Results are presented as means±SDs or median (95% confidence interval for the median).
HDL, high density lipoprotein; LDL, low density lipoprotein; EQ-5D, BEPSI-K, Korean version of the Brief Encounter Psychosocial Instrument; IPAQ, International Physical Activity Questionnaire; NKQ, nutritional knowledge questionnaire
Twenty-two participants (75.9%) completed a 6-month post-camp follow-up surveys. Our study results showed that exercise levels increased 1 month after camp attendance compared to pre-camp levels, and that body mass index (BMI), waist circumference (WC), and body fat percentage decreased significantly. However, these changes were not sustained. The participants had been intensively educated in terms of the importance of exercise and nutrition while attending the camp, they undertook a considerable amount of physical activity following the camp. However, after this initial period of training, it appears that they gradually lost their incentive to exercise. BP levels significantly decreased compared to pre-camp BP levels at 1 month and 3 months. Laboratory analysis results indicated no positive changes at 6 months compared to pre-camp levels except that high-density lipoprotein-cholesterol (HDL-C) levels had increased compared to pre-camp HDL-C levels at 6 months. Quality of life and depressive mood scores had improved compared to pre-camp scores, and nutritional knowledge was sustained for 6 months (Table 1).
The beneficial effects of camp-based health programs have been reported in several previous studies. Participants sharing experiences at a camp with other participants of similar ages with similar illnesses, and having an improved understanding of their illness, has been reported to lead to an increase in life satisfaction and an improvement in anxiety and depression.2 In a previous study, after a 5-day diabetes boot camp where participants with diabetes were followed up for 6 months, HbA1c levels were significantly decreased at 3 months post-camp but had increased again at 6 months. However, knowledge gained from the camp and psychological well-being persisted for up to 6 months, which was similar to our findings.3 Another study involved a 12-month follow-up of a 7-day diabetes camp for children with type 1 diabetes, and showed that HbA1c levels were significantly reduced at the 12-month post-camp follow-up compared to pre-camp levels.4 In that study, the authors reported that they provided motivation for each visit. Therefore, it appears that ongoing education and motivation are essential to maintain lifestyle modifications and to promote regular exercise, although camp-based programs are effective as a means of patient education.
In summary, the 2-day multidisciplinary boot camp had long-term positive effects on WC, quality of life, depressive mood, and nutritional knowledge in patients with MetS. However, physical activity, BMI, and WC improved in the short term after the camp, but these improvements were not sustained. In this study, patient education was provided only during the camp, and no further education or goals were offered during the follow-up period. Ensuring that motivation is enhanced and sustained is necessary through additional education to maintain healthy lifestyle changes, following on from physical exercise training and education sessions.5 Further research on the long-term efficacy of ongoing motivation is needed.