La depresión constituye un grave problema de salud pública que requiere mayor y mejor atención. En el presente ensayo revisamos el panorama epidemiológico de la depresión en adolescentes de México y discutimos algunas estrategias para su detección temprana y atención oportuna.
La sintomatología depresiva es prevalente en jóvenes y adultos en México, como en muchos otros países, con una mayor proporción de casos entre las mujeres. Los jóvenes en condiciones socio-urbanas más conflictivas muestran tasas más elevadas de depresión.
Si bien los trastornos depresivos son más prevalentes en las mujeres, en los hombres sus consecuencias pueden tener repercusiones de gravedad aún mayores que en las mujeres. El estigma hacia la depresión en los hombres puede conducir a que se intente enmascarar los síntomas mediante conductas de alto riesgo. Las mujeres tienen mayores tasas de intento de suicidio, pero en los hombres los intentos son más letales. Las tasas de suicidio consumado en varones son más altas en la mayoría de los países del mundo, y México no es la excepción. Pese a las barreras y escasos recursos en las instituciones de salud y educación, será necesario continuar desarrollando alternativas que permitan una mejor atención de la problemática de salud mental en la población joven, aun cuando sus necesidades no puedan ser expresadas directamente o que los motivos de consulta sean ‘‘otros’’, frecuentemente enmascarados por conductas problemáticas, como la violencia y las adicciones, entre otras.
Depression is an important public health problem that requires more and better attention. In the present work we review epidemiologic studies of depression among adolescents in Mexico and discuss strategies that may help in earlier identification and referral of potential cases for timely care.
In summary, depressive symptoms are prevalent among adolescents and adults in Mexico as in many other countries, with a higher ratio of female cases. Young people experiencing the most challenging socio-urban situations have higher rates of depression.
Even though depressive disorders are more prevalent among females, consequences may be even worse for males. The authors posit that, among males, stigma attached to depression might lead to attempts to hide depressive symptoms by masking them through high-risk behaviors (e.g., alcohol, drug use, and violence, among others). Women may have higher rates of suicide attempts, but the case-fatality rate of suicide attempts is higher among males. Despite barriers and resource scarcity among healthcare and educational institutions, it is necessary to continue to develop alternatives that will lead to better attention of mental health issues among the youth, even when their mental health needs are not expressed directly or their chief complaints are in regard to ‘‘other’’ health issues.
Pagina nueva 1
1. What is depression?
Disorders commonly referred to as depressive include a number of clinical entities related to problems of varying intensity and duration such as major depressive disorder (MDD) and dysthymia which, according to the DSM-5, are mood disorders. They refer to syndromes formed by different behavioral patterns of clinical significance, which do not conform to conventional responses and whose unique feature focuses on a mood disorder associated with discomfort and disability as well as the risk of losing life, suffer pain or lose freedom.1,2
Thus, these disorders are characterized by their impact on the mood and affection of people, linked to changes or problems in other areas of life such as appetite, fatigue, sleepiness, cognitive difficulties, excessive guilt, and suicidal ideation, among others. Whereas scientific research provides new elements to better understand the etiology of depressive disorders, there are still fundamental questions to be resolved. For example, some studies identify individual factors such as genetics, psychological trauma and/or strokes,3-5 whereas others stress the importance of psychosocial factors such as life events and economic and political crises, among others6-9 or the interaction of various factors in complex ways that can hardly be resolved with approaches focused exclusively on the individual.10-12 Marked differences in the incidence of depressive disorders among countries and regions show that these, like many others health problems, are not distributed randomly.8 Relative lack of knowledge does not necessarily mean that the approach is inadequate, but only the need to further develop methods and research to refute or clarify the etiology of the problem.
This discussion is important because it specifically impacts the identification and treatment of depression in adolescents. For example, a recent study found significant differences in symptoms of depression among teenagers and older adults, with higher rates of suicidal ideation among adolescents and higher rates of somatic symptoms in older adults.5 However, beyond the particular manifestations that are yet to be better understood, depression is a serious public health problem due to its impact on individuals and society, requiring more and better attention. In this essay the epidemiological picture of depression in Mexican adolescents is reviewed and some of its characteristics and impact are discussed. The literature tends to further analyze depression among adult females and adolescents. In this study, attention is focused on teenage boys and the differences with females.
2. Sociostructural determinants of health
Income distribution, public policies, and investment in education and health are examples of structural social factors that affect the health of populations. Health and disease are not distributed randomly among the population, but according to various individual, family and social factors.13 However, beyond the importance of individual behavior aimed at protecting health and life, various reports compiled by the WHO concluded that there are structural factors that ultimately determine the health status of populations.14 Although personal hygiene and health knowledge are of fundamental importance in individual welfare, the fact is that the so-called sociostructural determinants of health govern most health situations. The epidemiological transitions realize how sociohistorical factors impact the health profiles of populations.15,16
For example, let us consider data from the National Survey of Household Income and Expenditure conducted by the National Institute of Statistics and Geography (INEGI) in 2010 17 of which investigative journalist Lorenzo Meyer notes that in Mexico the wealthiest 20% received 50.1% of the national income, whereas the poorest 20% received only 5%, i.e., one tenth. This disparity in income distribution can be more easily understood if one considers that in 2009 the share of national income for wage earners was 32.5%, whereas the profits from commercial enterprises accounted for 68.2%.18
These marked inequalities are important in themselves as they directly affect opportunities and access to shelter, food, education and health services, which impacts not only adults but also children, adolescents, and older adults and generates an inadequate social environment for the needs of the general population. For example, data reported by journalist Ricardo Rocha showed that >7 million young people in Mexico neither attend school nor work. It draws attention to the marked increase in the rate of youth crime and imprisonment in recent years, contrasting that “...we close schools to our youth due to lack of space, but we opened prisons despite the overcrowding.”19 This is the macrosocial context in which emotional disturbances occur in Mexico and, as we shall see, has specific consequences in all areas of life.
3. Epidemiology of depression in Mexico
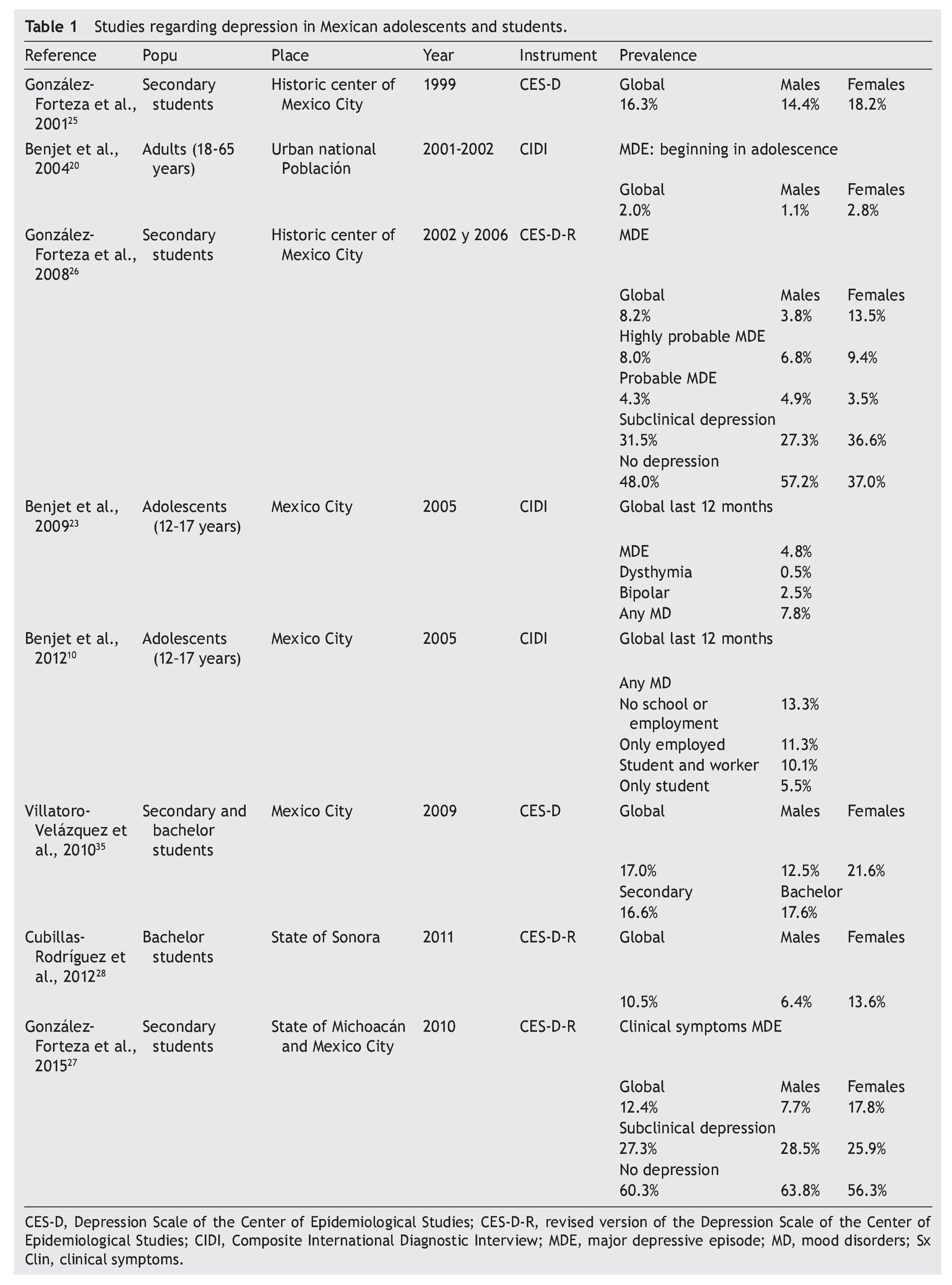
Between 2001 and 2002, the National Survey of Psychiatric Epidemiology (ENEP) was conducted, which is representative of the urban population between 18 and 65 years old.20 Subjects were interviewed in their homes with the Composite International Diagnostic Interview (CIDI), which is a computerized diagnostic instrument aligned with the criteria of the WHO and the American Psychiatric Association in the DSM-IV.1,21,22 The results indicated that the prevalence of MDD ever in life was 7.2% with a ratio of two females to each male (9.8% and 4.4%, respectively). The analysis to identify the age of onset of the disorder showed that 2% of the adult Mexican population had suffered a MDD during childhood and/or adolescence with a predominance of females of almost 3:1 (2.8% and 1.1%, respectively). From another angle, among all adults who have had a MDD sometime in their life, 27.5% experienced it before 18 years of age. Note that the probability of having a next MDD was 1.8 times higher among those whose episode was initiated in childhood or adolescence. Episodes among people with early MDD were twice throughout their life compared to those whose onset was in adulthood (6.8 vs. 3.1 episodes, respectively). It is obvious that if subjects received treatment during the first MDD, they would be less likely to suffer from another. In fact, results of the ENEP showed that most chronicity of depression with early start was due to the lack of early detection and timely treatment, not only because it began in childhood or adolescence.
In 2005, the Survey of Adolescent Mental Health was conducted in Mexico City using the same method as the ENEP. MDD prevalence over the past year in adolescents was 4.8%,23 higher than that reported by the ENEP in adults: 1.1% in males and 2.8% for females. On the other hand, the prevalence of all mood disorders in adolescents during the past year was 7.8%.23 When analyzing this information in regard to the occupation of adolescents (studies and/or work, or none10) it was observed that the prevalence of mood disorders was lower in those who only studied (5.5%) and was increasing in those who were studying and working (10.1%), those who were only working (11.3%), and even higher among those who neither studied nor worked (13.3%).
As noted, data reported here have been obtained from the CIDI diagnostic instrument whose mode of application is by an interview in computerized format, which requires a trained and previously certified staff. This eliminates certain biases that affected previous research.
A review of the results obtained in an adolescent population in Mexico with the Depression Scale of the Center for Epidemiologic Studies (CES-D) occurs.24 This is a screening tool originally designed to detect probable cases of depression in adults, which is currently used in various populations from around the world. As a screening tool, it is economical in material and time of application (consisting of 20 items) and is self-administered. In addition, it allows detection of elevated depressive symptoms or depressive distress.
A first study applied in Mexico in 1999 with high school students from 12-15 years old using the CES-D24 identified a prevalence of 16.3% of high depressive symptoms (‘depressive distress’, according to the conceptual definition of Angold6 and whose cutoff is established for each sex according to the mean ± standard deviation, with a slightly higher proportion in females (18.2%) than males (14.4%).25
Subsequently, other studies were conducted with two cohorts (2002 and 2006), also with high school students between 12 and 15 years old from the Historic Center of Mexico City. The revised version of the CES-D (CES-D-R26) was applied, another screening instrument that incorporated 15 additional reagents to the original version of the CES-D and extended the evaluation period to 2 weeks to assess according to the MDD diagnostic criteria established on the DSM-IV via a computer algorithm. Results showed that 8.2% of students had a probable MDD, predominantly females with a ratio of 5:1 (13.5% and 3.8%, respectively). The categories of “highly probable MDD” and “probable MDD” combined showed 12.3% overall, with a male/female ratio close to 1:1 (12.9% and 11.7%, respectively). The category of “subclinical depression” was identified in almost one third of the school population (31.5%), with a prevalence of 36.6% for females and 27.3% for males. These figures revealed noticeable symptoms of depression that did not exceed the clinical threshold needed to establish a diagnosis of MDD but indicated the presence of significant emotional problems that require prevention.
Upon analyzing the information of high school students on campuses throughout the state of Michoacan and the Historic Center of Mexico City, it was observed that the prevalence of clinical symptoms of MDD was 12.4%, with a female predominance (17.8%) and 7.7% in males. The prevalence of students with symptoms at a subclinical threshold requiring a type of preventive care was >25% of the school population (27.3%), with a close 1:1 ratio between males and females (28.5% and 25.9%, respectively).27
In a survey with high school students in the state of Sonora, a prevalence was identified of depressive distress (10.5%) with a 2:1 female/male ratio for every male (13.6% and 6.4%, respectively).28
To elaborate on the data, Table 1 provides a summary of the features and results of various studies using the CIDI and the CES-D/CES-DR. In short, the depressive problem occurs in young adults and, in Mexico as in many other countries, with a higher proportion of cases among females. Most young people living in troubled socio-urban conditions show higher rates of depression.
4. Implications of depression among adolescents
MDD may occur with other disorders. Those who suffered from these in childhood and/or adolescence were more likely to have agoraphobia, social phobia, oppositional defiant disorder, conduct disorder, and drug dependence, compared to depression with onset in adulthood. In addition, those who suffered depression from an early age were 50% more likely to have attempted suicide.29
It is important to understand the differences in rates of depression according to sex. Sex is biologically different from the genre, which corresponds more to the socialization of the role and refers to the behaviors, attitudes, emotions, knowledge and values socially defined and, in that sense, the stereotypes that define masculinity and femininity. For example, the male social role is associated with instrumental behaviors (express anger but not sadness), whereas in females it is associated with emotional aspects (express sadness but not anger). One area of great current interest is how the characteristics of biological sex meet socialized gender role, either exacerbating or mitigating the risk of depression and its associated symptoms.
In this regard, the conceptual framework developed by Raffaelli and Ontai,30 which include notions like familism, machismo and Marianism, could be productive to understand the impact of the intersection between biological sex and gender in the study of depression. Differentiating adaptive aspects from maladaptive ones regarding the role of socialized gender could help prevent and treat depressive symptoms as aspects related to gender roles are much more malleable than biological sex. For example, whereas depressive disorders are more prevalent in females, males can have consequences even more serious than females. Among other factors, the stigma of depression in males can lead to the attempt to conceal or mask symptoms with high-risk behaviors such as engaging in violent acts, recklessness, or attempting suicide while legitimizing their ‘masculinity’ at a high cost. It is true that females have higher rates of suicide attempts, but it is also true that the attempts by males are more lethal.31
Empirical evidence suggests, with relative amplitude, that females are affected in a major way by depression in all its manifestations. However, it is worth pondering whether this marked difference is due to how the assessment, screening and diagnosis tools are built. It is probable that the manner in which some components of depression are evaluated underestimate the most typical male depressive responses. A study showed that after adjusting for levels of depression, adult males were less likely to report symptoms of sadness than females of the same age, even according to level of depression.32 However, a recent study found no evidence that the difference in rates of depression by sex were due to males in general (not only the elderly) and are less likely to report depressive symptoms when they do.33 Could it be that males feel less sadness? Is it that depression is expressed differently by gender or that as “good males,” men deny their pain and find it difficult to acknowledge their sadness?
The finding that mood disorders are more common among adolescents who do not work or attend school underlines that the occupational role has implications on the emotional state. Considering that during this age student occupation is the most prevalent in urban areas such as Mexico City and that the additional condition of work or only work is closely related to the lack of economic resources means that, in this order of ideas, to not study or work highlights a social problem that permeates emotional wellbeing. Therefore, the responsibility lies with both the health sector and others, which also modulate the development of young persons and their environment: educational, mass media, labor, and legal, among others. Approaching the problem from multiple sectors may allow ‘the full picture’ and thus, efforts can be more fruitful.
While adolescents and youth are still students, the school system is configured as a window of opportunity for promoting wellness, early detection of mental health problems and timely referral to treatment. However, it is essential to combine efforts of the educational system and the health system to optimize the quality of life for students34, at least from one perspective. Schools inserted in their social context cannot accomplish this alone and require support of the resources responsible for safeguarding the surrounding areas and socioeconomic quality of its inhabitants.
It should be noted that children and teenagers often do not seek help for themselves. In Mexico, it is required to be accompanied by at least the adult parent or adult guardian for health care problems, including emotional ones. Unlike behavioral disorders or attention deficit hyperactivity disorder that often cause inconvenience to parents and/or teachers, children and adolescents with depressive disorders often go unnoticed. The challenge is to establish surveillance systems for early monitoring of mental health needs and to establish appropriate care campaigns, promoting and maintaining mental health. There is sufficient evidence to consider the appropriateness of the use of the CES-D to detect elevated depressive symptoms/depressive discomfort as well as the CES-D-R as a diagnostic screening tool for detection of probable cases of MDD due to their adequacy and effectiveness in addition to being practical, economical and easy to apply instruments.
It is also worth considering the relevance of incorporating some changes in health policies to expand and facilitate immediate access to hospitals and case follow-up, community centers, among others, to receive effective treatment. This is where multidisciplinary collaboration and interagency work will yield the greatest results. As mentioned above, epidemiologic research shows the presence of the problem in the general population. It is also known that the prevalence is higher in populations with unfavorable psychosocial situations and among users of health services. The problem of depression occurs in clinical practice in organizations such as children’s hospitals or general medical clinics. Despite the traditional barriers and limited resources, it is necessary to continue developing alternatives to better care for mental health problems in patients, even when the needs cannot be expressed directly by them or that the original reasons for medical consultation have been for other reasons, for example, somatic.
Ethical responsibilities
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Funding
U.S. National Institute for Minority Health and Health Disparities (Grant R24 MD002803) to Dr. Fernando A. Wagner.
Conflict of interest
The authors declare no conflict of interest of any nature.
Acknowledgments
The authors acknowledge the National Institute for Minority Health and Health Disparities of the U.S. for financial support for the study.
Received 18 March 2015;
accepted 9 April 2015
http://dx.doi.org/10.1016/j.bmhimx.2015.05.006
* Corresponding author.
E-mail:fernando.wagner@morgan.edu (F.A. Wagner).