Orbital cellulitis is an infectious disease that is very common in pediatric patients, in which severe complications may develop. Etiological agents related to this disease are Haemophilus influenzae B, Staphylococcus aureus, Streptococcus pneumoniae and Moraxella catarrhalis, 95% of the cases. Streptococcus beta-hemolytic and anaerobic microorganisms may also be present and cause <5% of the cases. We present an uncommon case of orbital cellulitis complicated by a subperiosteal abscess caused Streptococcus pyogenes.
Case ReportA 9-year-old male patient with a history of attention deficit disorder and hyperactivity disorder since he was five years old. His illness started with erythema on the outer edge of the right eye, increase in the peri-orbicular volume with limitation of eyelid opening, progression to proptosis, pain with eye movements and conjunctival purulent discharge. Image studies reported a subperiosteal and pre-septal right abscess with extraocular cellulitis. Empirical antibiotic treatment was started, surgical drainage was performed, and Streptococcus pyogenes was isolated from the culture of the obtained purulent material.
ConclusionsDue to the implementation of vaccination schemes against H. influenza and S. pneumoniae since the 90s, the cases by these pathogens have decreased, causing new bacteria to take place as the cause of the infection. The importance of considering S. pyogenes as an etiology of orbital cellulitis comes from its rapid progression to abscess formation, and the few cases described in the literature.
La celulitis orbitaria es una enfermedad infecciosa muy frecuente en la edad pediátrica que puede provocar el desarrollo de severas complicaciones. Los principales microorganismos involucrados son Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae y Moraxella catarrhalis, que juntos corresponden al 95% de los casos. También se pueden presentar Streptococcus beta hemolíticos y microorganismos anaerobios, que corresponden a menos del 5% de los casos. Se presenta un caso poco frecuente de celulitis orbitaria complicada por absceso subperióstico ocasionado por Streptococcus pyogenes (estreptococo beta hemolítico del grupo A).
Caso clínicoPaciente masculino de 9 años de edad con antecedente de trastorno por déficit de atención e hiperactividad desde los 5 años de edad. Inició su padecimiento actual por presentar eritema en canto externo del ojo derecho; posteriormente, aumento de volumen periorbicular con limitación de apertura palpebral, progresión a proptosis, dolor a los movimientos oculares y secreción conjuntival purulenta. Los estudios de imagen reportaron absceso subperióstico y preseptal derecho con celulitis extraocular. Se inició manejo empírico con antibióticos, drenaje quirúrgico y cultivo del material purulento. De este, se aisló Streptococcus pyogenes.
ConclusionesDebido a la implementación de los esquemas de vacunación desde la década de los 90 contra H. influenza y S. pneumoniae, los casos por estos patógenos han disminuido, provocando que nuevas bacterias tomen su lugar como causantes de la infección. La importancia de considerar a S. pyogenes como etiología de celulitis orbitaria radica en la rápida progresión para la formación de abscesos, así como los pocos casos descritos en la literatura.
Orbital cellulitis is an infectious disease that usually occurs in children between 5 and 12 years old, predominantly in men, and especially during the cold months. The most frequently involved microorganisms are Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis. Together, they cause 95% of cases. Beta hemolytic Streptococcus and anaerobes correspond to less than 5% of cases.1 The cases of orbital cellulitis occur with a frequency of 6 to 27%, and the incidence of orbital abscesses as a complication of sinusitis is between 1 to 2%. The Haemophilus influenzae type b and pneumococcus vaccines have been associated with a decrease in the frequency of cases caused by these bacteria. This has caused a change in frequency of the isolated pathogens in cultures from patients with orbital cellulitis, increasing the frequency of rare bacteria such as group A Beta-hemolytic Streptococcus.
Streptococcus pyogenes is considered one of the major human pathogens because of its exceptional ability to colonize and infect. Orbital cellulitis cases associated with S. pyogenes are characterized by a progressive and rapid evolution and the onset of complications which may be fatal. These primarily affect vision when subperiosteal and orbital abscesses occur. The more severe complications are cavernous sinus thrombosis, parameningeal irritation, subdural empyema, blindness and even death.2 The aim of this study was to report a case of orbital cellulitis by S. pyogenes, which is rare in the Mexican pediatric population.
2Clinical vignetteA 9-year-old male patient with a history of attention deficit hyperactivity disorder (ADHD) since he was five years old and who had a vaccination schedule complete for his age.
Arrived at the emergency department after a 3-day course of illness, which had started at night with erythema on the outer edge of the eye, with no previous history of blunt trauma, laceration or insect bite. Referred ocular and lower eyelid pruritus were referred; He had no fever, ocular discharge or catarrhal symptoms. The next day, he presented an increase in the right peri orbicular volume, conditioning a limitation to eyelid opening of approximately 30%. He went to a doctor who, integrated the diagnosis of acute conjunctivitis and prescribed ophthalmic eye drops. The patient did not present clinical improvement; the progression of the edema continued, now with the limitation of the ocular movements, right proptosis, localized pain in the jaws and frontal and ocular region of moderate to high intensity that conditioned prostration, as well as purulent conjunctival secretion.
Physical examination revealed an occlusion of the eyeball of 80%, forced palpebral aperture with digital support, and moderate pain to manipulation and ocular movements. There was no lesion of the appendages, but there was a respected sclera, light clear yellow discharge predominantly in the ipsilateral internal canthus, isochoria, and normoreflexia. In the left eye, visual acuity was 20/20. However, in the affected eye was not assessable. He presented halitosis, deviated nasal septum to the right, congestive nasal mucosa, edema, scarce rhinorrhea and posterior pharyngeal discharge with green secretion.
When he arrived, his vital signs were within normal ranges. Laboratory tests reported hemoglobin 13.5g / dl, hematocrit 38.6%, leukocytosis 19.1×10 3 /μL, lymphocytes 2.32×10 3 /μL, neutrophils 15.1×10 3 / l, platelets 244×10 3 /μL and C-reactive protein of 2.1mg / l.
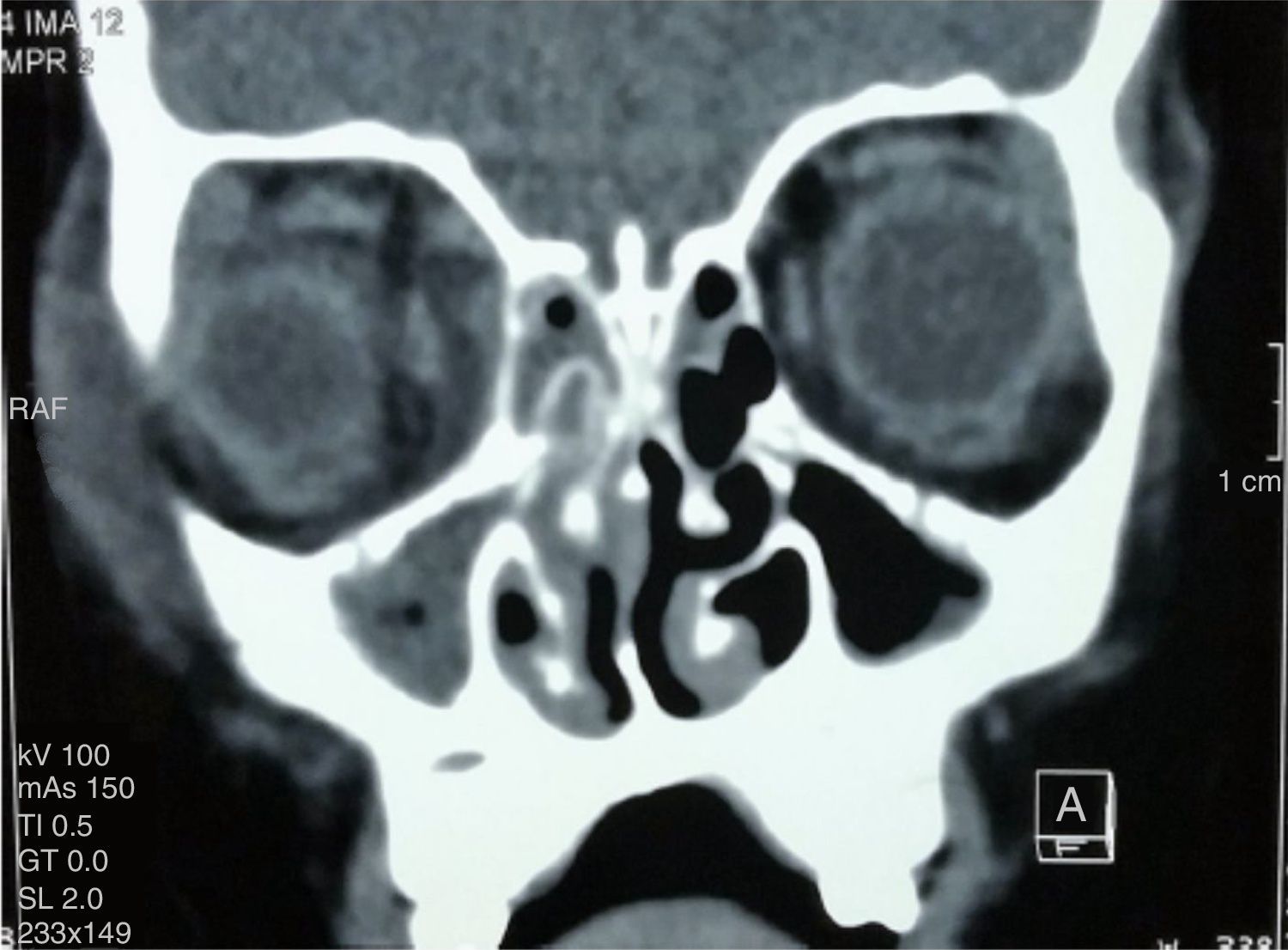
A computerized axial tomography (CT) of the orbits and soft tissues, showed a subperiosteal and right preseptal abscess with extraocular cellulitis, in addition to the occupation of the maxillary, right ethmoidal and left anterior sinuses (Figures 1 and 2).
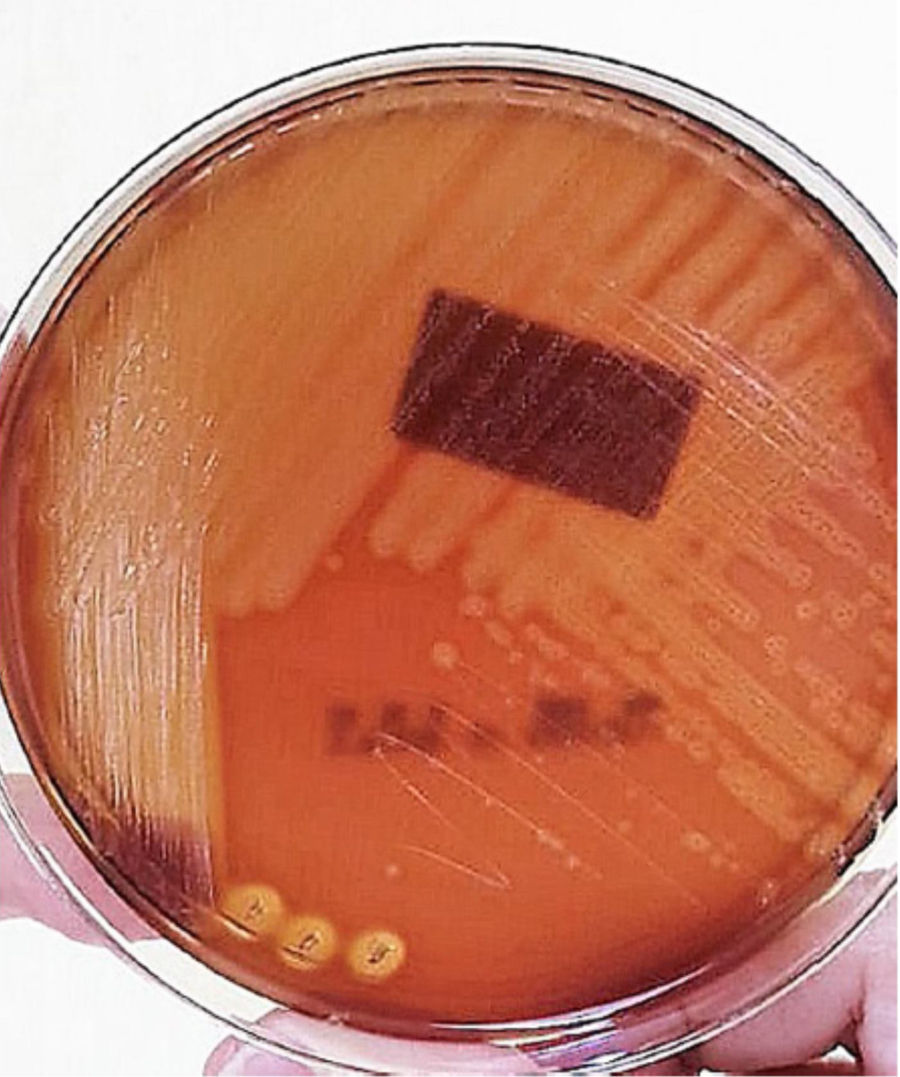
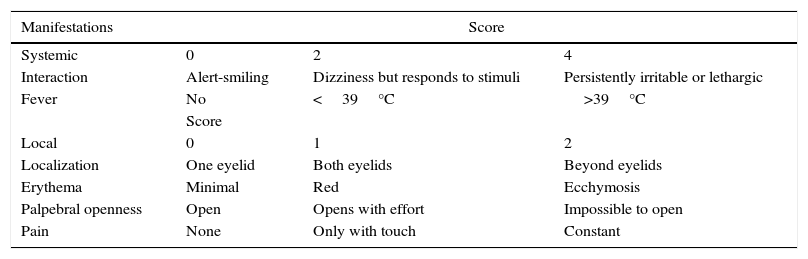
Based on the clinical features and CT findings, the diagnosis of orbital cellulitis and Chandler's grade III subperiosteal abscess was integrated, with six points in the VU severity index. Empiric antibiotic regimen with ceftriaxone (15mg / kg / day every 12h), oral vancomycin (420mg every 6h) and metronidazole (40mg / kg / day every 8h) was implemented for 4 days. The patient was approached surgically through transnasal endoscopy. The abscess was drained through the lamina papyracea. Gram staining and culture of the purulent material were performed on sheep blood agar.
Secretion abscess culture showed circular, translucent and smooth surface beta hemolytic colonies with an entire margin and variable diameter, from were Streptococcus pyogenes (Figure 3) was isolated. Gram staining showed cocci grouped in pairs and chains of varying diameter and length. The bacterial antibiogram showed sensitivity to benzylpenicillin (MIC ≤0.06), so the antibiotic scheme was changed to amoxicillin/sulbactam (90mg/kg/day every 12h for 14 days).
At discharge, laboratory tests showed a decrease of leukocytes to 14.2×10 3 / μL, 6.16 lymphocytes×10 3 / l, neutrophils 7.07×10 3 /μL, hemoglobin 14.2g / dl and 40% hematocrit. The patient was discharged after for clinical improvement and resolution of the subperiosteal abscess without complications. He continued with an oral antibiotic regimen with amoxicillin / clavulanic acid after medical discharge (2 tablets every 12hours for seven days). His follow-up in the following months has been favorable.
The patient's guardian gave consent for the publication of the case and images of the case.
3DiscussionOrbital cellulitis (post septal) is an infectious disease that occurs most frequently in the pediatric age. The most common underlying factor for its development is ethmoidal sinusitis.1 In contrast, in periorbital cellulitis (preseptal) lesions are direct to the eyelid due to trauma, insect bites or skin lesions (chickenpox, bites); predisposing causes may occur secondary to an infectious or inflammatory process, such as the case of conjunctivitis and dacryoadenitis.2
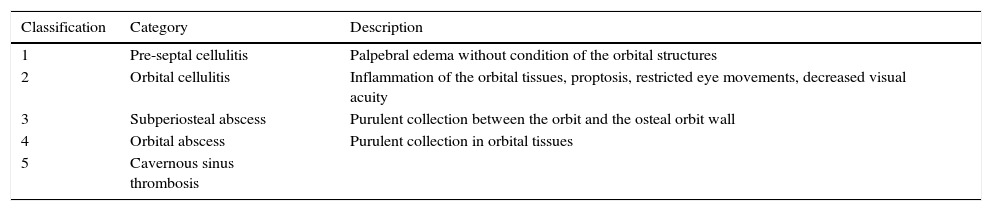
The first classification of peri or orbital cellulitis was described by Hubert in 1937, later revised by Smith and Spencer in 1948 and modified by Chandler et al. in 1970. These researchers classified orbital complications of sinusitis into five categories (Table 1). This classification is used as an indicator of the severity of the disease.3 The subperiosteal abscess and clinical characteristics classify the present case as a type 3 of this scale.
Chandler classification of orbital disease.
| Classification | Category | Description |
|---|---|---|
| 1 | Pre-septal cellulitis | Palpebral edema without condition of the orbital structures |
| 2 | Orbital cellulitis | Inflammation of the orbital tissues, proptosis, restricted eye movements, decreased visual acuity |
| 3 | Subperiosteal abscess | Purulent collection between the orbit and the osteal orbit wall |
| 4 | Orbital abscess | Purulent collection in orbital tissues |
| 5 | Cavernous sinus thrombosis |
The involved microorganisms in orbital cellulitis commonly are bacteria associated with respiratory infections such as Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae and Moraxella catarrhalis and other streptococci species and anaerobe microorganisms.1
The introduction in Mexico of the conjugate vaccine against Haemophilus influenzae type b (Hib) in 1995, and subsequently the PCV7 which was introduced in 2006 and since 2011 gradually replaced by the PCV13, has caused a decline in the number of cases by these microorganisms, allowing a breach for the infection of other pathogens that once were infrequent.4,5
Staphylococcus aureus is the causative agent in at least 30% of patients; the incidence of methicillin-resistant strains varies from 23-72%. The incidence of this agent in the orbital and sinus cultures has been approximately 20% of all isolates reported in the literature.6
It has been found that the etiology of cellulitis is different according to the origin. In cases secondary to dental infection it is related to anaerobic bacteria and Streptococcus spp.; in infections or trauma to the skin, with S. aureus and Beta hemolytic Streptococcus; Finally, those secondary sinus infections are caused by Haemophilus influenzae type b (Hib), Moraxella catarrhalis, and Streptococcus spp.7
A retrospective study conducted over a 5-years period in Colorado, USA, in a population between 2 and 18 years, identified 94 patients with orbital infections confirmed by CT scan, whose only predisposing cause was sinusitis. The most frequently identified pathogen was Streptococcus anginosus (15%) followed by S. aureus (9%), and less frequently S. pyogenes (6%).4
Beta hemolytic streptococcus has been associated with cellulitis in patients with a history of facial trauma or recent oral or sinus surgery.8 The patient reported in this study denied insect bites, trauma or any laceration. In the CT scan, the occupation of the maxillary and ethmoidal sinuses could be observed; Therefore, the route of entry of the bacterium was related to a respiratory tract infection that, as a consequence, generated sinusitis.
Many disseminated infections by Streptococcus pyogenes have been associated with the M protein.9 The M protein encoded by the emm gene, protein is the major virulence protein in this bacteria and is responsible for the production of a specific type of antibodies in humans. There may be an association between emm types and different clinical manifestations, although this continues to be controversial.10 More than 220 emm types have now been identified. In Europe and North America, a small number of emm types account for the majority of the isolates, while in Africa and Pacific regions has been found a great diversity.11
Orbital cellulitis is a potentially serious infection in the pediatric age because of the low bone thickness that separates periorbital tissues from orbital and cerebral structures, as well as various nerves and vessels that pierce the finer portion of the medial wall of the orbit, the lamina papyracea.12 There is also a more frequent pattern of seasonal occurrence during cold months and a slight predominance of infection on the left side over the right.
The diagnosis is based on a clinical examination that identifies fever, poor general state, pain, edema, erythema and chemosis of the eyelids, signs of orbital affection such as proptosis, decreased visual acuity, ophthalmoplegia, pain with ocular movements and diplopia.
Vu and colleagues developed a severity index for orbital cellulitis that evaluates systemic and local signs and correlates them with the management of oral or intravenous antibiotics based on the score obtained (Table 2). Children who required intravenous antibiotic therapy scored six points, while the oral therapy group scored two points. Although this index correlates well with the general state of the child and it is highly sensitive to changes in severity, more evidence of its real utility is required to determine the need for hospitalization, the route of delivery of antibiotic therapy, and its effectiveness.13
Vu's score to assess the severity of orbital and periorbital cellulitis.
| Manifestations | Score | ||
|---|---|---|---|
| Systemic | 0 | 2 | 4 |
| Interaction | Alert-smiling | Dizziness but responds to stimuli | Persistently irritable or lethargic |
| Fever | No | <39°C | >39°C |
| Score | |||
| Local | 0 | 1 | 2 |
| Localization | One eyelid | Both eyelids | Beyond eyelids |
| Erythema | Minimal | Red | Ecchymosis |
| Palpebral openness | Open | Opens with effort | Impossible to open |
| Pain | None | Only with touch | Constant |
Paranasal sinus radiography helps confirm the presence of sinusitis. This comprises four standard projections: lateral, base, Waters and Caldwell.14 The characteristic finding is the opacification of the sinuses. More often, the ethmoidal sinus is affected, followed by the maxillary sinus; the affection of the frontal sinus is infrequent, and very rarely the sphenoid sinus is affected.15
Simple computed tomography in axial and coronal projections is essential to staging the disease, besides it is the imaging study of choice to evaluate patients with acute sinusitis and suspected orbital disease. The presence of an abscess is suggested by a low-density mass effect, the medial displacement of the medial rectus muscle or the movement of the periosteum away from the lamina papyracea, whereas inflammation of the medial rectus muscle usually indicates orbital cellulitis.16 In this patient, tomography was the method that was used to evaluate possible ocular or intracranial complications. A subperiosteal and right preseptal abscess was localized.
Isolation of bacteria was performed by blood culture. The collection of the sample can be through the aspiration of wounds, the culture of purulent material that from a fistula or that has been obtained by drainage of abscesses.8 The culture medium of choice for the growth of Beta-hemolytic Streptococcus pyogenes is the ram blood agar. However, the efficacy of alternative culture media has been evaluated: human blood agar with washed red blood cells (ASHGL), human blood agar washed with red blood cells plus sodium azide (ASHGLA), and human blood agar with non-washed red blood cells (ASH). The results have shown that ASHGL, because of its excellent sensitivity, specificity, and predictive values, is as effective as ram blood agar.17 The culture medium that was used for this case was ram blood agar and isolated Streptococcus pyogenes.
Orbital cellulitis is frequently a complication related to acute sinusitis in children; in the literature3 it has an estimated 74 to 85% prevalence. Complications of cellulitis, in a significant part, are secondary to an increase in intraorbital pressure. Blindness occurs in approximately 1% of patients with orbital cellulitis. The most important complications are the formation of subperiosteal and orbital abscesses, cavernous sinus thrombosis with the involvement of the III, IV and VI cranial pair, parameningeal irritation, subdural empyema or even death.3
Regarding the treatment of this disease, two aspects must be taken into account: the choice of a medical treatment and the need for surgical treatment. As an initial approach, it is necessary to administer antibiotics empirically, based on bacteria most frequently involved and suspected route of infection, which guarantees coverage against staphylococci, streptococci, and anaerobes.2
Empirically, the most commonly used antibiotics are amoxicillin / clavulanic in cellulitis secondary to respiratory infections, and the combination of cloxacillin plus a cephalosporin (cefuroxime or cefotaxime) in cases of cutaneous infections. If poor clinical evolution develops or if it is suspected methicillin-resistant Staphylococcus aureus (MRSA), vancomycin may be used 40mg/kg/day.12 Also, treatment for anaerobes and its coverage by using metronidazole (30mg/kg/day every eight hours) should be considered, especially if there is intracranial affection.2
One of the newest treatment regimens suggests the empirically prescription of ampicillin/sulbactam (100-200mg/kg/day divided every six hours). If the patient is not allergic to penicillin, a regimen of ceftriaxone (50-75mg/kg/day every 12-24h) may be initiated, or if penicillin allergy is known, it may be instituted with moxifloxacin (10mg/kg / every 24hours). We recommend adding vancomycin to patients with a history of MRSA if there is evidence of an abscess or bone affection, orbital trauma to a recent eye surgery or a severe infection.18,19
For oral treatment, it is recommended to start amoxicillin / clavulanic (80-90mg/kg/day every 12hours). If there is no allergy to penicillin, cefpodoxime (10mg/kg/day every 12hours) can be used, and in cases of allergy to penicillin, it should be initiated moxifloxacin. The duration of treatment scheme varies depending on the severity of the disease, lasting between seven days to 3 weeks if there is involvement of bony structures.18,19
We have studied the effectiveness of penicillin and other antibiotics for S. pyogenes. The high activity of penicillin G confers 100% of susceptibility; additionally, cephalosporins and amoxicillin are almost equally effective. With a sensitivity of 97%, clindamycin can be used as a second line. Furthermore, vancomycin and levofloxacin have 100% sensitivity, so they can be an option if there is an allergy to penicillin or macrolide resistance which also have a sensitivity of 95%.20 The result of the antibiogram in this patient showed an excellent sensitivity towards benzylpenicillin, so it was decided to change the treatment scheme to amoxicillin/sulbactam. Good clinical response to this scheme regimen was observed.
One of the most debated aspects is the need for surgical treatment. Orbital abscesses should be drained without any delay. Intravenous antibiotics can penetrate the abscess, but without draining, antibacterial activity within the abscess is poor, probably because the purulent medium protects microorganisms from the antibiotics enzymatic degradation21. However, the decision to drain a subperiosteal abscess is complex and involves many factors such as the response to the antibiotic management, age, size and location of the purulent collection. Traditionally, drainage is achieved primarily through an external ethmoidectomy. However, currently, this technique is being displaced by the endoscopic approach.16 The transnasal endoscopic technique provides quick and safe drainage for the paranasal sinuses, the orbit and anterior skull base, offers better results, less surgical trauma and postoperative discomfort and speeds up the recovery period providing a shorter hospital stay.9 The location of the abscess, its size and the age of the patient, were evaluated. A surgical approach was chosen through the transnasal endoscopic technique, which also has a low contamination potential for the sample required for culture.
The development of vaccines to prevent infections by S. pyogenes has been an objective for many years. There are many vaccines in development in clinical or preclinical stages, mainly vaccines based on M protein such as the 26-valent and 30-valent vaccine. The first underwent phases clinical trial phases I and II with adult volunteers and was shown to be safe, well tolerated and immunogenic. The main obstacle to the full development of these vaccines is the high global complexity of the group A streptococcal infections epidemiology.22
Currently, due to the implementation in the 90s decade of vaccination against H. influenza and S. pneumoniae, cases by these pathogens have decreased, causing new bacteria to take their place as a cause of these infections. The importance of considering S. pyogenes as an etiology for orbital cellulitis relies on its rapid progression to the formation of abscesses and the few cases described to date in the literature. Due to the high susceptibility of this pathogen for G penicillin, this should be the treatment of choice, although, in the case of allergies, cephalosporins and amoxicillin are equally effective.
Orbital cellulitis in the pediatric age is a pathology that must be diagnosed quickly and opportunely, before the development of intracranial complications that can potentially cause fatal consequences that would modify the quality of life of the patient. Therefore, a multidisciplinary approach involving pediatricians, ophthalmologists and otorhinolaryngologists is vital for a comprehensive management that reduces the intracranial complications that may endanger the life of the patient.
4Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
5FundingNone.
6Conflict of interestThe authors declare no conflicts of interest
We would like to thank all the team that collaborated in the approach of this case: infectologists, pediatricians, ophthalmologists, and otorhinolaryngologists. In the same way, we would to the microbiology laboratory for their process and keeping of the bacterial specimens.
Please cite this article as: Ruiz-Carrillo JD, Vázquez GE, Mercado UMC. Celulitis orbitaria complicada por absceso subperióstico debido a infección por Streptococcus pyogenes. Bol Med Hosp Infant Mex. 2017;74:134–140.