Introducción: La mortalidad neonatal es una de las prioridades de la salud pública, por lo que se debe revisar cómo la inestabilidad fisiológica del recién nacido después de un traslado contribuye al incremento de la mortalidad neonatal. El objetivo de este trabajo fue determinar si el índice de estabilidad fisiológica (TRIPS) en los recién nacidos trasladados a la Unidad de Cuidados Intensivos Neonatales de un hospital de segundo nivel sirve como factor predictivo de mortalidad neonatal temprana.
Métodos: Se valoró el índice de estabilidad fisiológica de la escala de TRIPS para predecir la muerte neonatal en los primeros 7 días del ingreso de los pacientes.
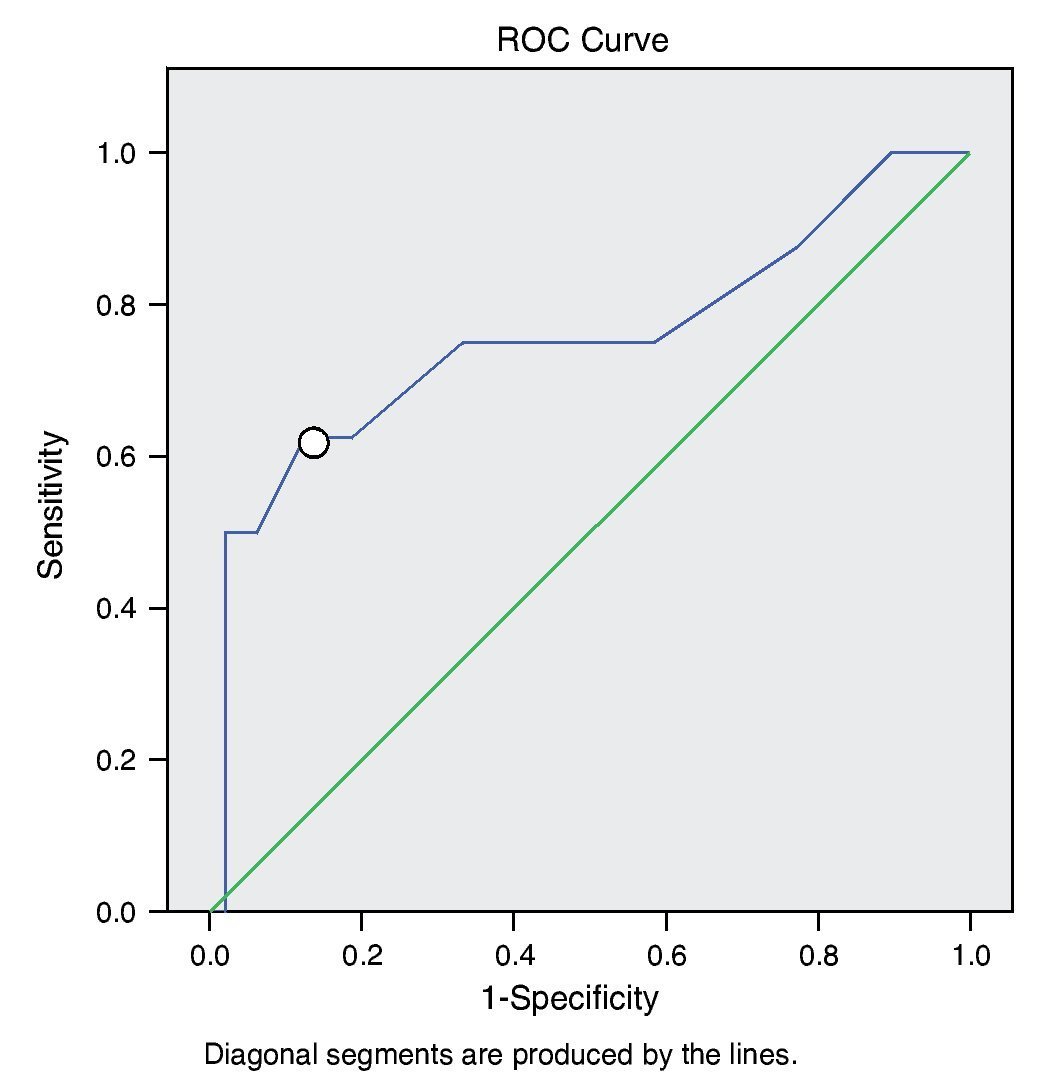
Resultados: Se encontró que la mortalidad neonatal a los 7 días del ingreso está relacionada con la puntuación de la calificación TRIPS. La puntuación de los sobrevivientes y las defunciones presentaron una diferencia significativa (p = 0.009). Para una puntuación de 16 se determinó una sensibilidad del 62% y una especificidad de 84%, con un área bajo la curva de 0.757.
Conclusiones: La ponderación del índice de estabilidad fisiológica de TRIPS es un buen predictor de la mortalidad neonatal. Es importante establecer medidas para mejorar la estabilidad fisiológica de los recién nacidos antes, durante y después del traslado, con la finalidad de disminuir la mortalidad neonatal.
Background: Neonatal mortality is a public health priority. We review the physiological stability of the newborn after a transfer, which contributes to increased neonatal mortality. The objective of this work was to determine whether the Transport Risk Index of Physiologic Stability (TRIPS) in newborns transferred to the Neonatal Intensive Care Unit of a secondary hospital serves as a predictor of early neonatal mortality.
Methods: We use the TRIPS to predict neonatal death in the first 7 days after patients’ admission.
Results: Neonatal mortality at 7 days after admission is related to the TRIPS rating. The score of the survivors and neonatal deaths show a significant difference (p: 0.009). For a score of 16, a sensitivity of 62% and a specificity of 84%; area under the curve of 0.757 was determined.
Conclusions: Physiological index weighting using TRIPS is a good predictor of neonatal mortality. It is important to establish measures to improve physiological stability of the newborn before, during and after the transfer in order to reduce neonatal mortality.
1. Introduction
Maternal and child health is one of the main objectives of the Millenium Development Goals of the World Health Organization (MDG-WHO). Reduction of infant mortality is the fourth objective of the MDG of the United Nations (MDG-4). To meet the target of the MDG-4, a substantial reduction in the rate of neonatal mortality in countries with high mortality is required. Reduction in the deaths that occur in the first week of life is essential to show progress in the reduction in the rates of mortality. Many of the initiatives have been directed to the first-contact health systems (prenatal care) and to hospitals (care of labor and of the newborn), with little or no attention to the impact that the transport of sick newborns (NB) has on neonatal mortality and the influence to reach the objectives established for 2015.1-5
Despite the regionalization of neonatal care services where transport of the mother-child before birth is the ideal condition for the best outcomes in morbidity and mortality, especially of the NB, very little attention has been paid to the emergency transport services and the impact they may have on decreasing neonatal mortality. There is no evaluation system that allows one to identify the clinical conditions of the NB before, during and at the end of the transport that contribute to neonatal mortality.1,3,6
During the last century, developed countries have implemented four strategies in the care of maternal health: prenatal care (in the 1930s); indications for cesarean section (in the 1950s); technology for perinatal care (in the 1970s); and the organization of perinatal health centers with transport services preferably prenatal (in the decade of the 1980s). Currently, one cannot determine which strategy has the greatest impact in influencing a decrease in perinatal mortality.7-11
Survival and its long-term health implications of the premature NB have increased over the years. This emphasizes the importance of a high quality of neonatal care which means, in the first place, regionalization of the neonatal services with the creation of specialized neonatal care centers for timely referral of the pregnant female and decrease in acute transfers (first 24 hours of life) of critically ill NB. In second place, the increase of delayed transfers (1 to 28 days of life), which ensures that the seriously ill NB are first stabilized and then transferred at the appropriate moment. There is a well-recognized association between an acute transfer of a premature NB due to a postnatal emergency and the increase in mortality and morbidity. The intent should always be to transfer the mother before labor, if the clinical conditions allow, so that the baby is born in an appropriate manner in a hospital with staff experienced in neonatal resuscitation, stabilization and specialized procedures. The increase in mortality and morbidity is seen especially in NB with a birthweight of < 1000 g.12-17
It is considered that ~5-10% of pregnancies will require specialized care, whether due to maternal condition or because of the health of the fetus. Faced with this situation there is a wide consensus that a pregnant female be admitted to a hospital with the ability to resolve pregnancy-associated problems. However, 40% of perinatal problems are unpredictable and the NB is born in institutions without the necessary resources for adequate care. In these cases it is the NB who requires transfer and admission to special care units. Care of the sick newborn requires human resources and equipment that should not, and cannot, be administered in all public maternity hospitals because of the enormous and inefficient use of resources that this would require. For this reason there are reference units of care with greater care capacity, with human and technological resources geared towards care of the NB who require specific technology or multidisciplinary care through different pediatric specialists.18,19
In developing countries, from 15-20% of NB are born in locations where the structure for adequate care does not exist and they require transfer to hospital centers with greater care capacity. The majority of the studies that analyze the results related with the perinatal level of care indicate that the morbidity of premature NB or seriously ill newborns rises when births take place in hospital centers without adequate experience for neonatal medical care. Successful transfer depends on the quality of care at the labor room, continuous and adequate care of the NB at the birth hospital, choice of transport, the transport team and the quality of the transport. Any of these basic points that does not receive special and careful care could result in irreparable damage because of the deterioration suffered by the NB and may even lead to death.20,21
Transfer of the NB to the neonatal intensive care unit (NICU) represents an indicator of morbidity that can be used for the design and implementation of interventions directed towards improving the health and survival of the neonate. The referrals could be divided into two categories: 1) self-referral where the mother and her NB, accompanied by a family member, present to the hospital for care; and 2) those coming from another hospital. The most common type of referral is the first type in 70% of the cases. Transfer of a NB to an NICU is classified into three categories: a) due to sociodemographic factors; b) maternal health factors; and 3) neonatal factors. The neonatal factors basically include low Apgar score, prematurity, low birth weight (< 1800 g) or weight > 4000 g, congenital malformations and suspected infection.22
The period close to birth is a critical moment for the NB who will transition from fetal life to life outside the uterus. The health personnel responsible for the care of the NB should have expertise in neonatal resuscitation and stabilization. In the hospital, it is important that the personnel and physicians have a planned transport algorithm so that the transfer can be done in efficiently. The algorithm components should include the name and address of the hospital, telephone number of the transport so as to establish a direct line to the NICU, system for gathering medical information of the mother and the off-spring including results of all tests performed at the place of birth, maternal blood samples, cord blood sample, and ideally, the placenta. Key factors for stabilizing an ill NB are the following:23
Respiratory support
Cardiac output and blood pressure
Temperature stabilization
Establishing a permeable venous access
Initial laboratory tests
Orogastric tube placement for emptying the stomach
The transport team generally consists of a physician, neonatal nurse, general nurse, and respiratory therapist. They should bring the necessary equipment and medications to ensure a safe transport. Recent studies have suggested that neonatal transfers are commonly carried out incorrectly for the following reasons: 1) there is no clinical evaluation before the transfer or on arrival at the referral facility and 2) the personnel responsible for the transport do not have the necessary experience in the care of seriously ill newborns. The transfer should be seen as an integral part of the continuous process of care that the child requires. It is important that at the conclusion of the transfer of the NB the patient’s clinical condition is not worse. Stabilization of the NB before the transfer is paramount because adequate physiological conditions are associated with better survival rates. Stabilization before transfer has two phases: a) initial care during the hospital stay; and b) care during the transfer itself. The goal of the two phases is to resuscitate and stabilize the patient during the entire referral process.24
Providing an effective neonatal transport requires an accurate assessment of the severity of the disease and the prognosis so as to facilitate a proper triage and allocation of resources. Unfortunately, the scores developed for evaluation of the NB during the transport process have used data obtained after the transport team has arrived at the hospital and not before. The Transport Risk Index of Physiological Stability (TRIPS) is useful to predict mortality at 7 days post-transport and the occurrence of severe periventricular bleed. It helps to evaluate how the neonatal transport took place, allows to detect avoidable problems (e.g., hypothermia), can be used to evaluate the quality of care in primary and secondary care hospitals and aids in establishing protocols to improve stabilization prior to transport. It has four elements: temperature, respirations, blood pressure and neurological status.25-27
The TRIPS scale, like other physiological stability scales, is used to predict mortality within 7 days of the NB admission. TRIPS is used to detect changes in the physiological state of the NB, which should ideally be evaluated before the transfer and upon admission to the referral hospital. Changes in the evaluation of the TRIPS before and after transport are associated with changes in mortality. For example, for all categories of the TRIPS, the decrease in the value of the measurement was associated with lower mortality, unlike when the value remained unchanged. An increase in the value of the scale was associated with increased mortality. The risk of mortality in the category of 0 to 10 points is very low, for which some difference in the evaluation before and after transport is not significant.26
There are various models for assigning personnel in charge of neonatal transfers. These generally include a combination of nurses, neonatal nurses, paramedical staff, resident physicians and specialist physicians. Currently, it has been accepted that specific preparation in neonatal transport is essential for best results. Team members should have the ability to diagnose and treat neonatal problems and to identify the most frequent causes of deterioration. Principles of transport medicine should be included as well as pathophysiology of the most common congenital anomalies and a high level of experience for procedures that may be required during transport such as cardiopulmonary resuscitation, invasive monitoring, fluid management, venous and arterial access, endotracheal intubation and ventilatory management.27-29
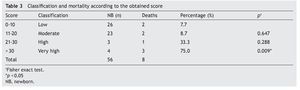
TRIPS has been used to measure the physiological consequences that can potentially be caused by neonatal transport. It is based on four components of physiological stability that are easily recorded: temperature (0-8 points), blood pressure (0-26), response to stimuli (0-17) and respiratory status (0-14). In the original validation it was classified into four categories according to the measured values (the higher value, greater severity): low score (0-10), moderate score (11-20), high score (21-30) and very high score (> 30). Pre- and post-transport measurements allow for detection of changes in the clinical condition during transfer. Increase in the score during the transfer is associated with greater mortality.30-32
The need for neonatal transport has increased recently due to the regionalization of the Neonatal Care Units. Neonatal transport requires experienced personnel and demands the capacity to provide complex intensive care in a difficult environment.33-36
For all of the above, the overall objective of this work was to determine if the physiological stability index in newborns transferred to the NICU of the Regional Hospital of Río Blanco, Veracruz, Mexico, serves as a predictor of early neonatal mortality.
2. Methods
We designed an observational, cross-sectional and retrospective study. The population was comprised of NB transferred to the NICU of a second-level hospital from another hospital during 2010, 2011 and up to October 2012. Newborns were identified in the admission log of the NICU and the clinical records were requested.
2.1. Description of the process
NB sent from another hospital were identified from the log of admissions to the NICU. With the identification number the clinical records were requested to gather the variables to be studied. For this study, only medical records with complete information were included for evaluation by TRIPS.
2.2. Inclusion criteria
NB admitted to the NICU, transferred from another hospital, clinic or sanatorium, between January 2010 and October 2012, were included in the study.
2.3. Exclusion criteria
Those NB whose medical record was not found and those whose medical records did not have scores for the four TRIPS parameters were excluded.
2.4. Operationalization of variables
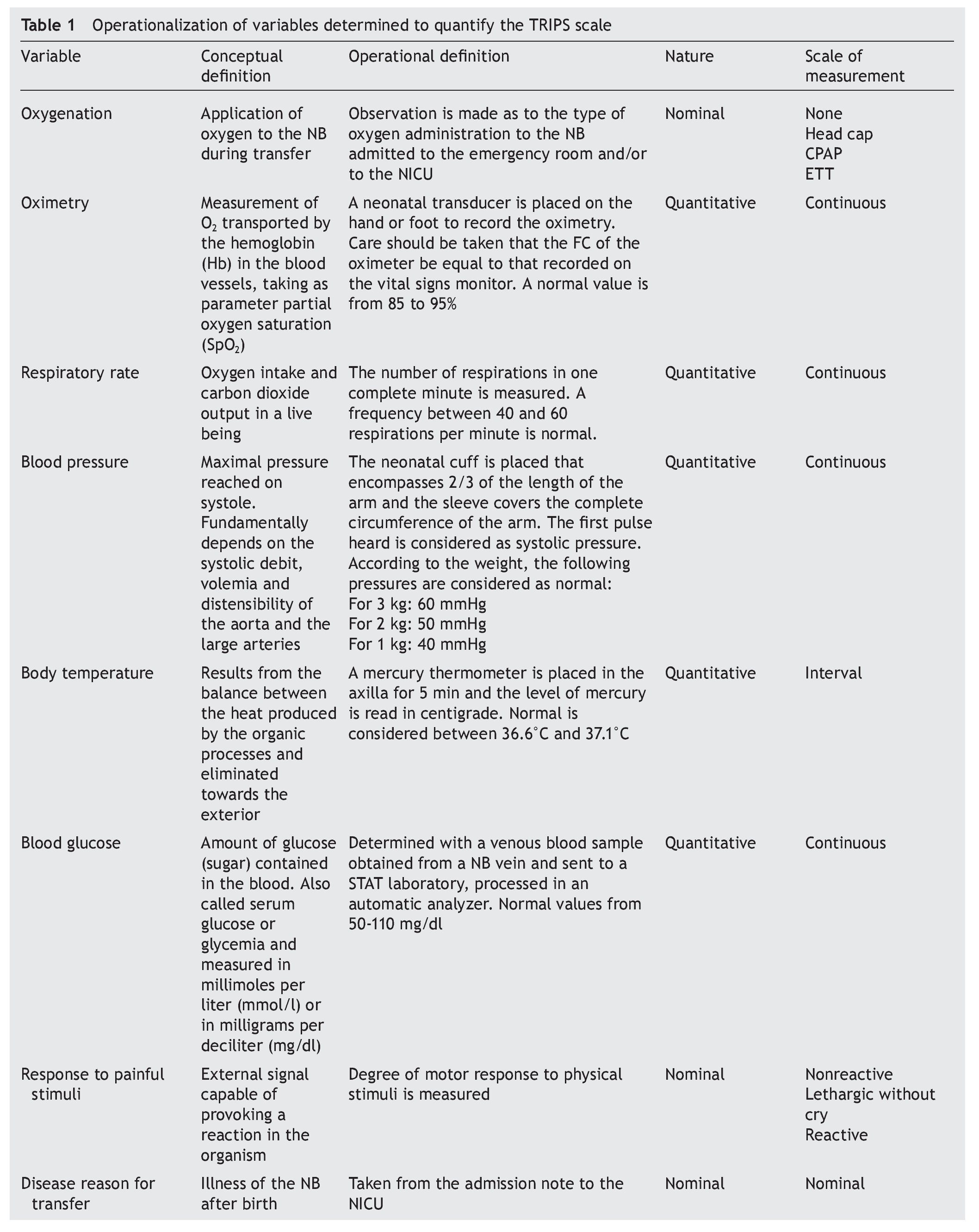
Variables that were taken into account were evaluated according to the criteria described in Table 1.
3. Results
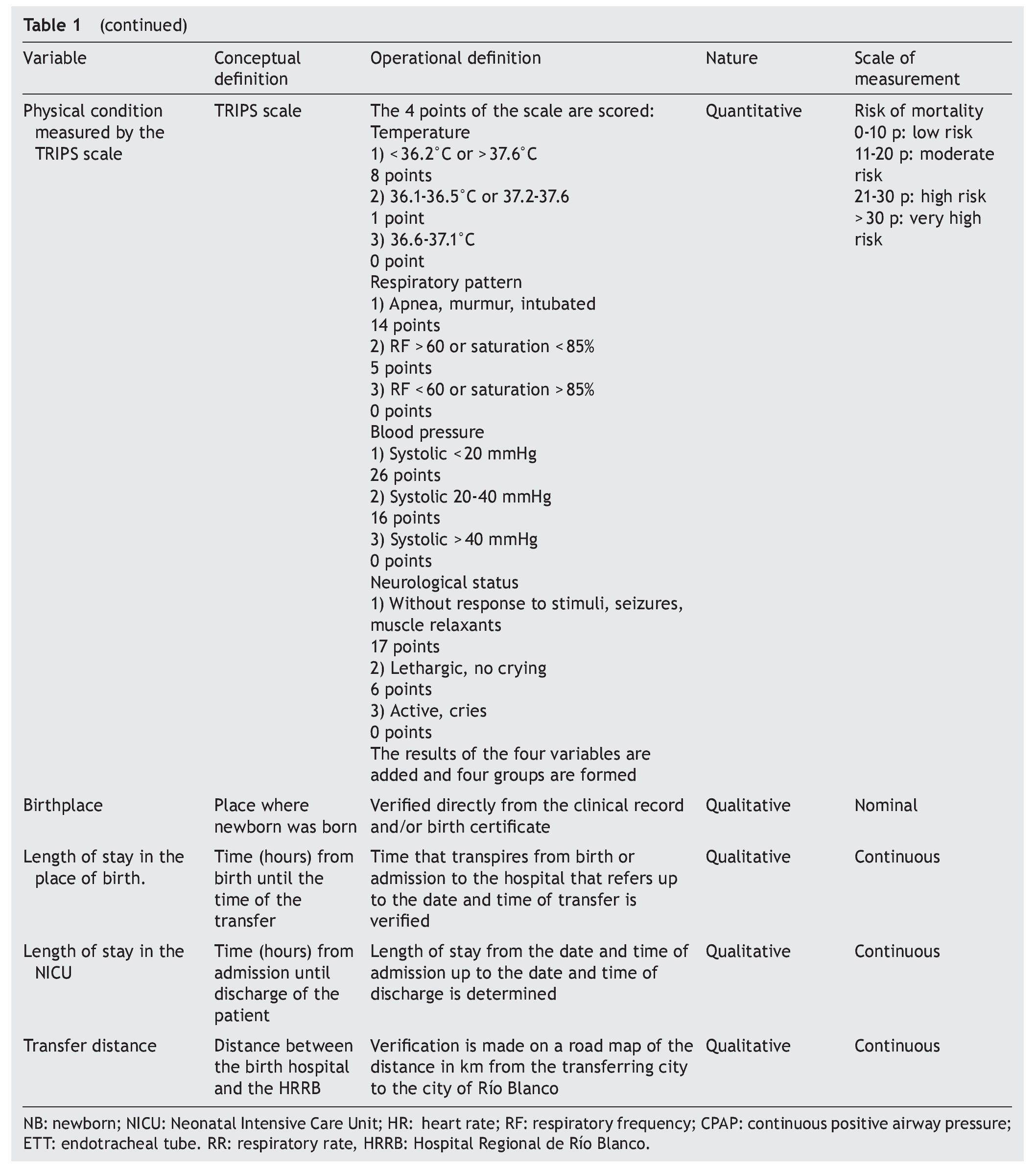
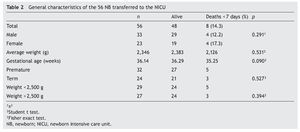
Fifty-six clinical records were found that contained complete information of the four parameters measured by the TRIPS scale. The number of NB with complete TRIPS evaluation increased with the passage of time; 59% of the patients transferred were males (n = 33). Mortality was 12% in males (n = 4) and 17% in females (n = 4), without significant difference (p = 0.291). The weight range for all NBs was 0.950–4.11 kg. The average weight for the survivors was 2383 g and for those who were deceased was 2126 g (p = 0.531). As there was no significant difference, it was considered that weight had no relation with the probability of death at 7 days. Gestational age of live NB was 36.29 weeks of gestation (WG) and for deceased 35.25 WG (p = 0.090) (Table 2).
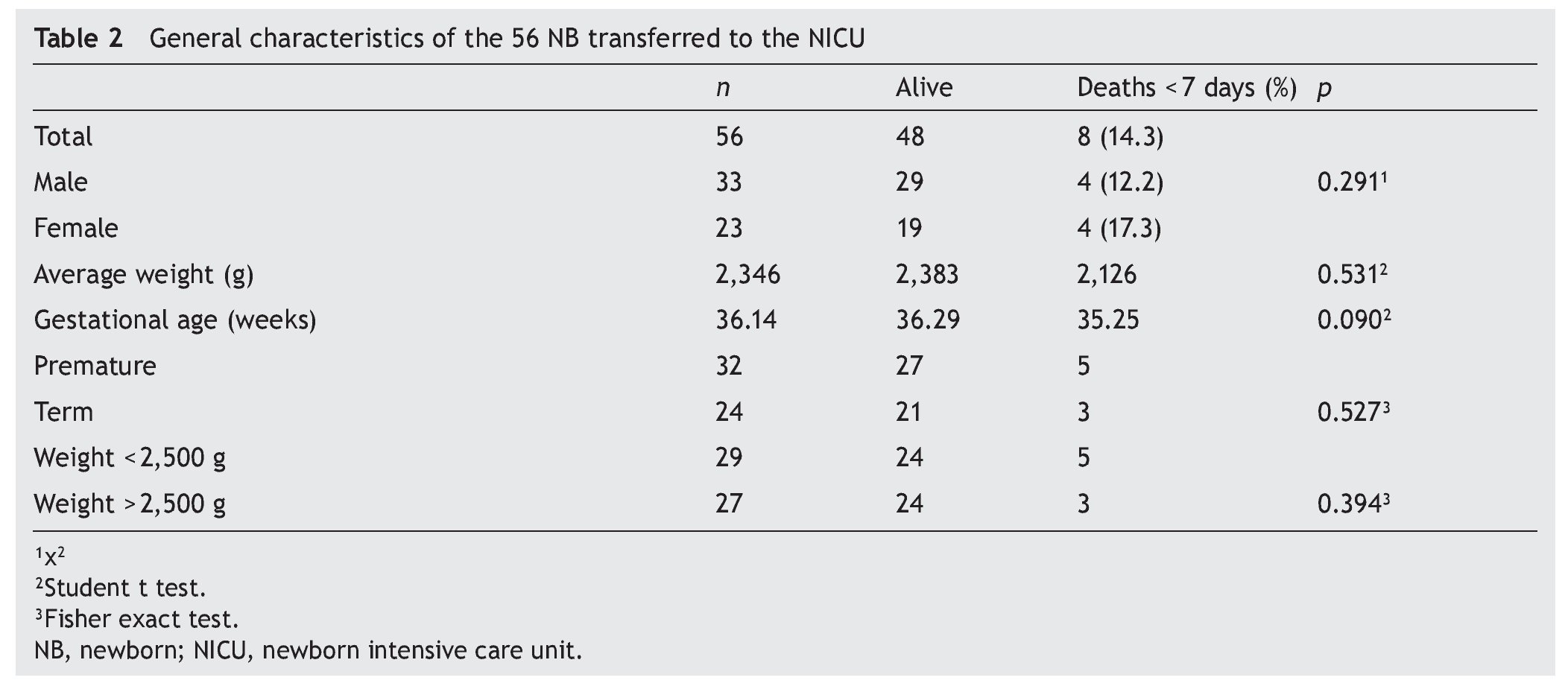
According to the total points upon adding the parameters of the TRIPS scale, it was observed that, in effect, the lower the score, the lower was the mortality. In the low-risk category, the mortality was 7.7% (n = 2). In the very high-risk group with > 30 points, mortality was 75% (n = 3). With these results it can be said that the scale is a good indicator of neonatal mortality at 7 days of admission and that it agrees with what is reported in the literature. The low-risk group was taken as a reference for the statistical tests, comparing it with the other groups. Statistical significance was found (p = 0.009) only when compared with the very high-risk group (Table 3).
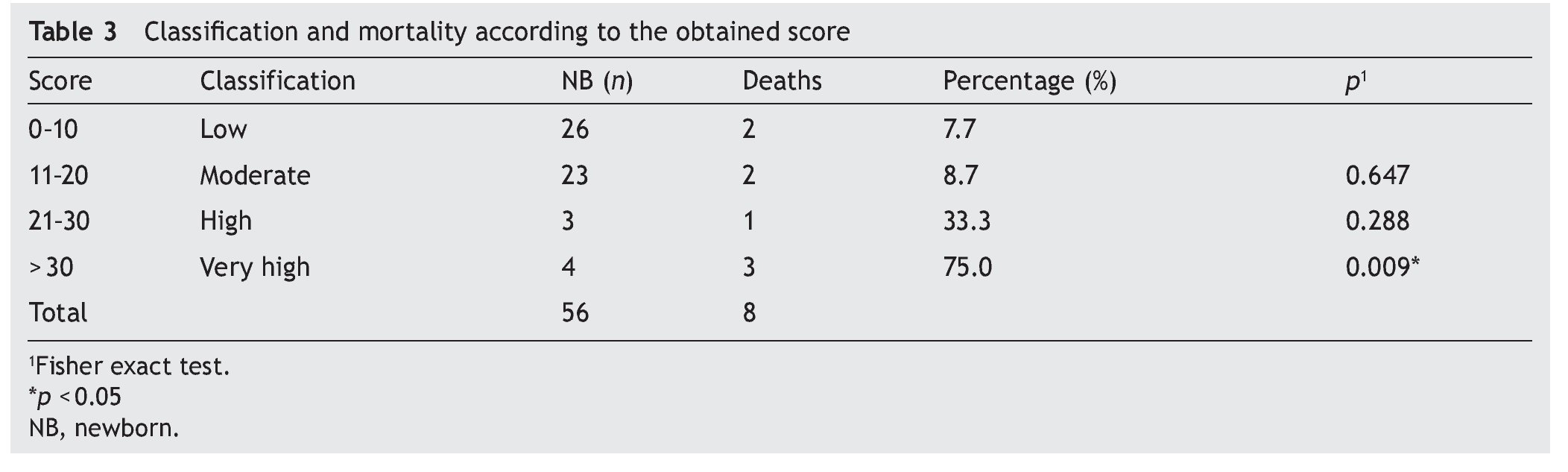
If the TRIPS score is considered to predict the possibility of death at 7 days of admission, taking as positive the death, a ROC curve is obtained with values for sensitivity and 1-specificity. It was observed that the type of curve is considered of moderate value, with area below the curve of 0.757 (Figure 1).
Figure 1 ROC curve of the qualification of TRIPS.
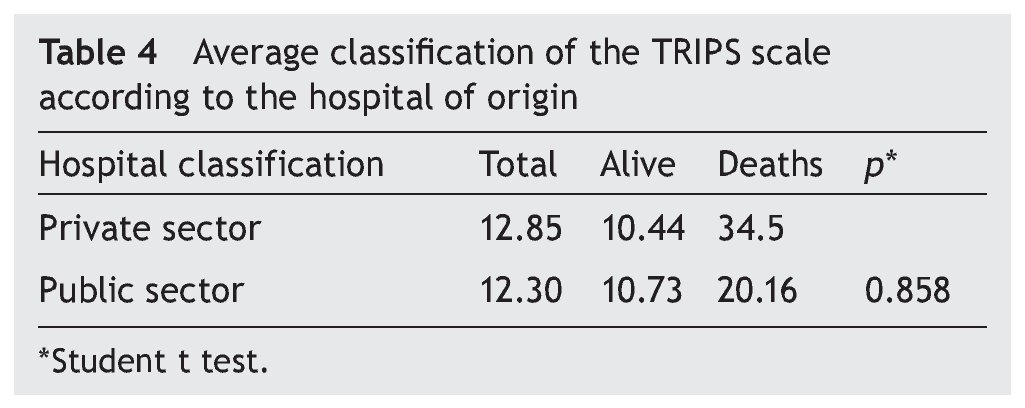
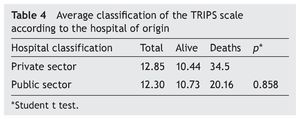
Even though the average rating of the TRIPS is 4% higher in the private sector hospitals, indicating more seriously ill patients or with less care during the transfer, there is no difference when compared with the scores of the NB of hospitals in the public sector (Table 4).
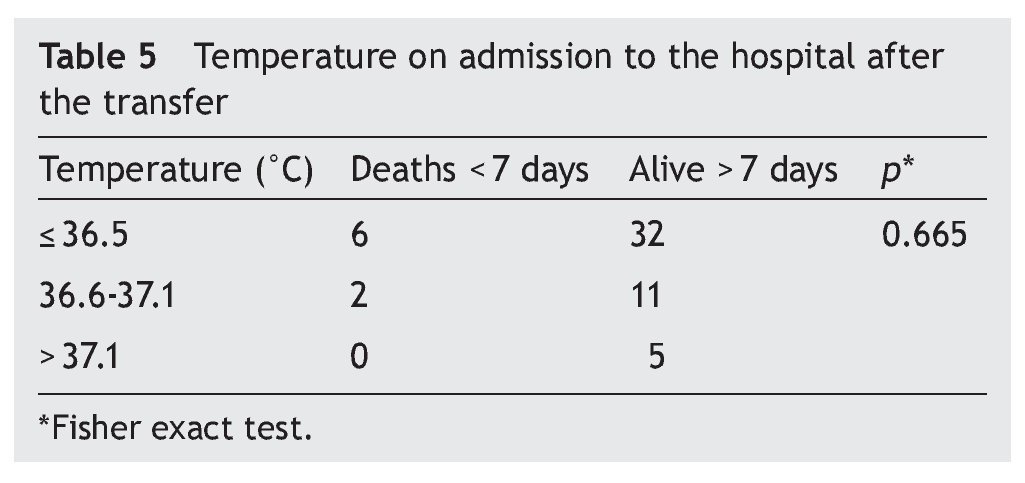
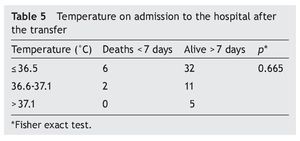
Of the four criteria scored by the TRIPS scale, temperature was the least controlled parameter during the transfer. It was found that 68% (n = 38) of the NB presented hypothermia, 23% (n = 13) were recorded with a temperature considered normal and 9% (n = 5) presented temperature elevation. In comparing the group of the hypothermic NB with the NB with normal temperatures, a statistical relationship was observed (p = 0.665) (Table 5).
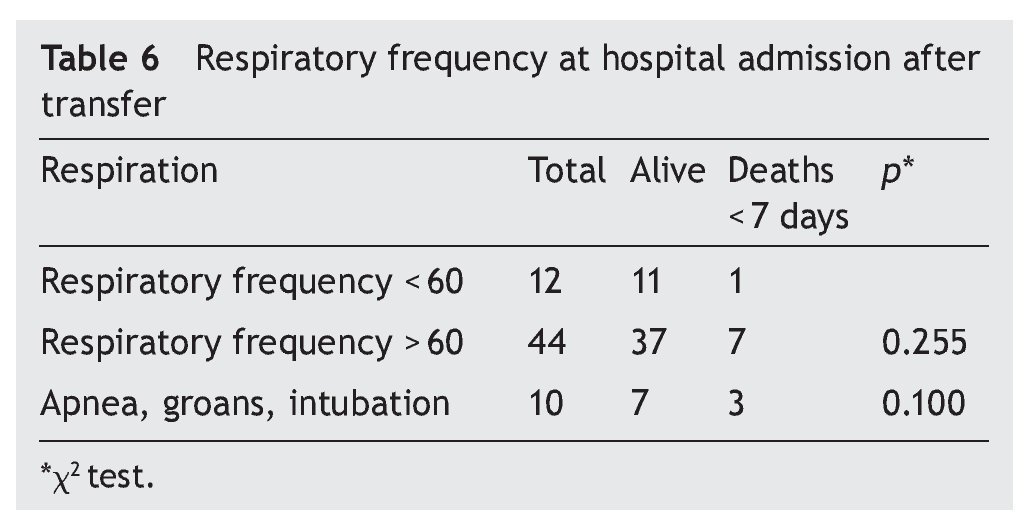
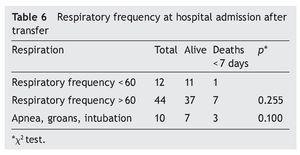
For assessment of respiratory function, the criterion to weigh was the respiratory rate (RR), recorded in all the records. However, there was no significant difference when the normal RR was compared against the increase in frequency. For this reason, it was decided to compare it with the presence of apnea, murmur or endotracheal intubation, although there were no statistically significant differences found (Table 6).
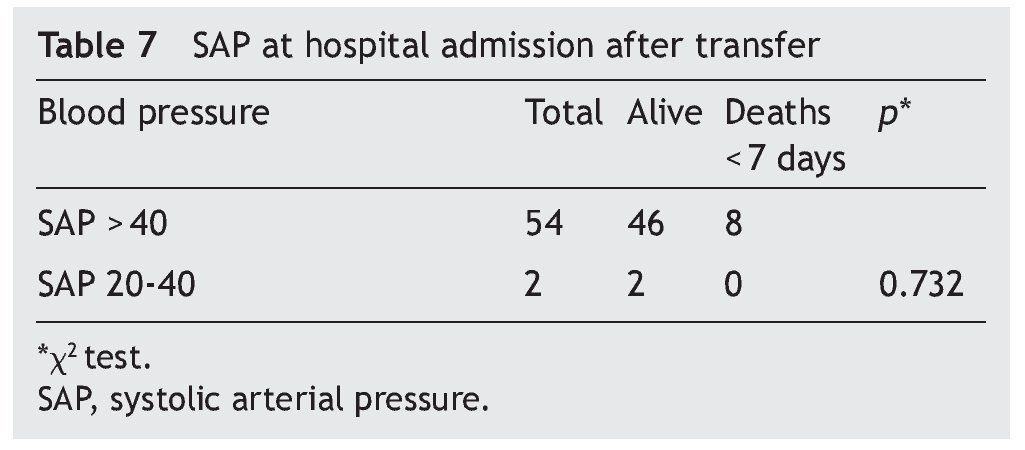
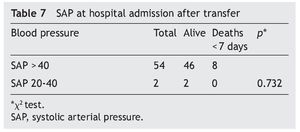
Blood pressure of the NB was considered as normal in 96% (n = 54) of the transfers. It is of note that, on admission, the eight NB who died had normal blood pressure. None of the patients received vasopressors during transfer (Table 7).
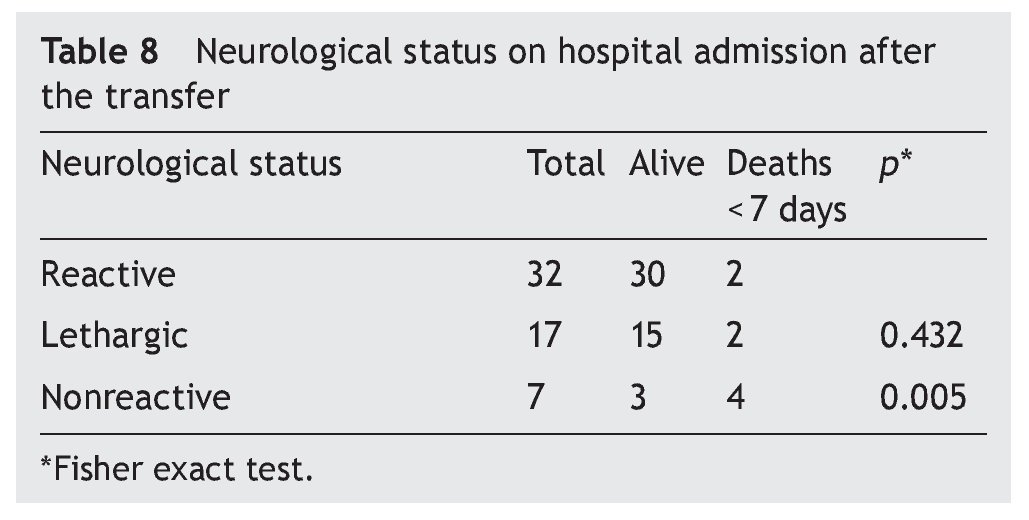
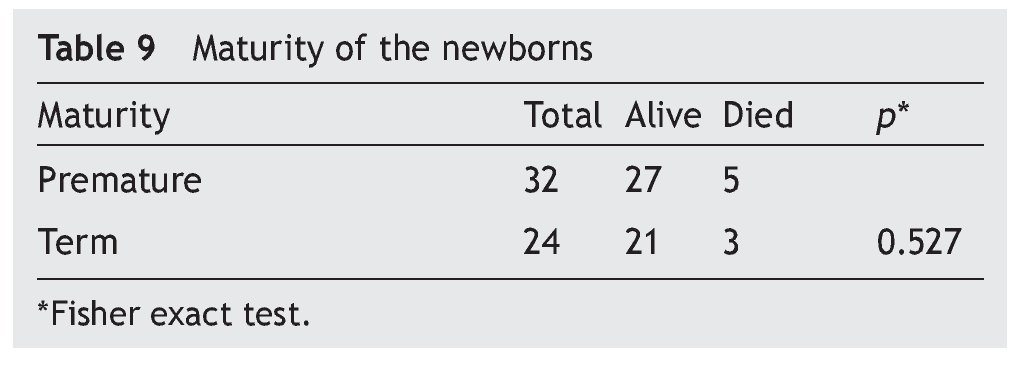
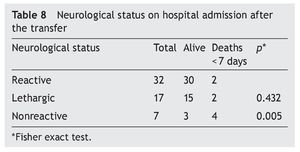
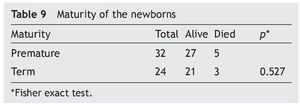
Neurological status was considered as normal or reactive in 57% (n = 32) of the NB transferred to the hospital. A non-reactive neurological state was present in 12.5% (n = 7), and it had a close relationship with the deaths (Table 8). With regard to gestational age, mortality was 16% (n = 5) in premature infants and 12.5% (n = 3) in term NB, without a significant difference (Table 9).
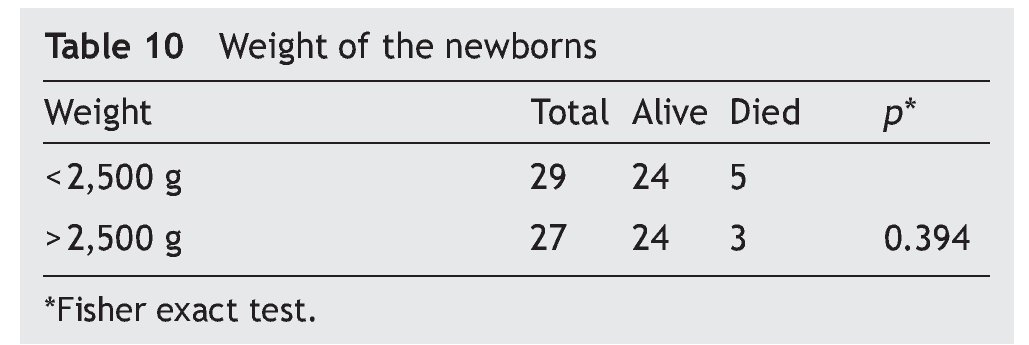
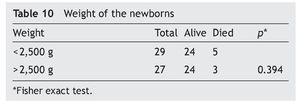
The influence of weight on mortality is not evident. In NB with weight < 2500 g, mortality was 17% (n = 5). In NB with weight > 2500 g, mortality was 11% (n = 3) (p = 0.394) (Table 10).
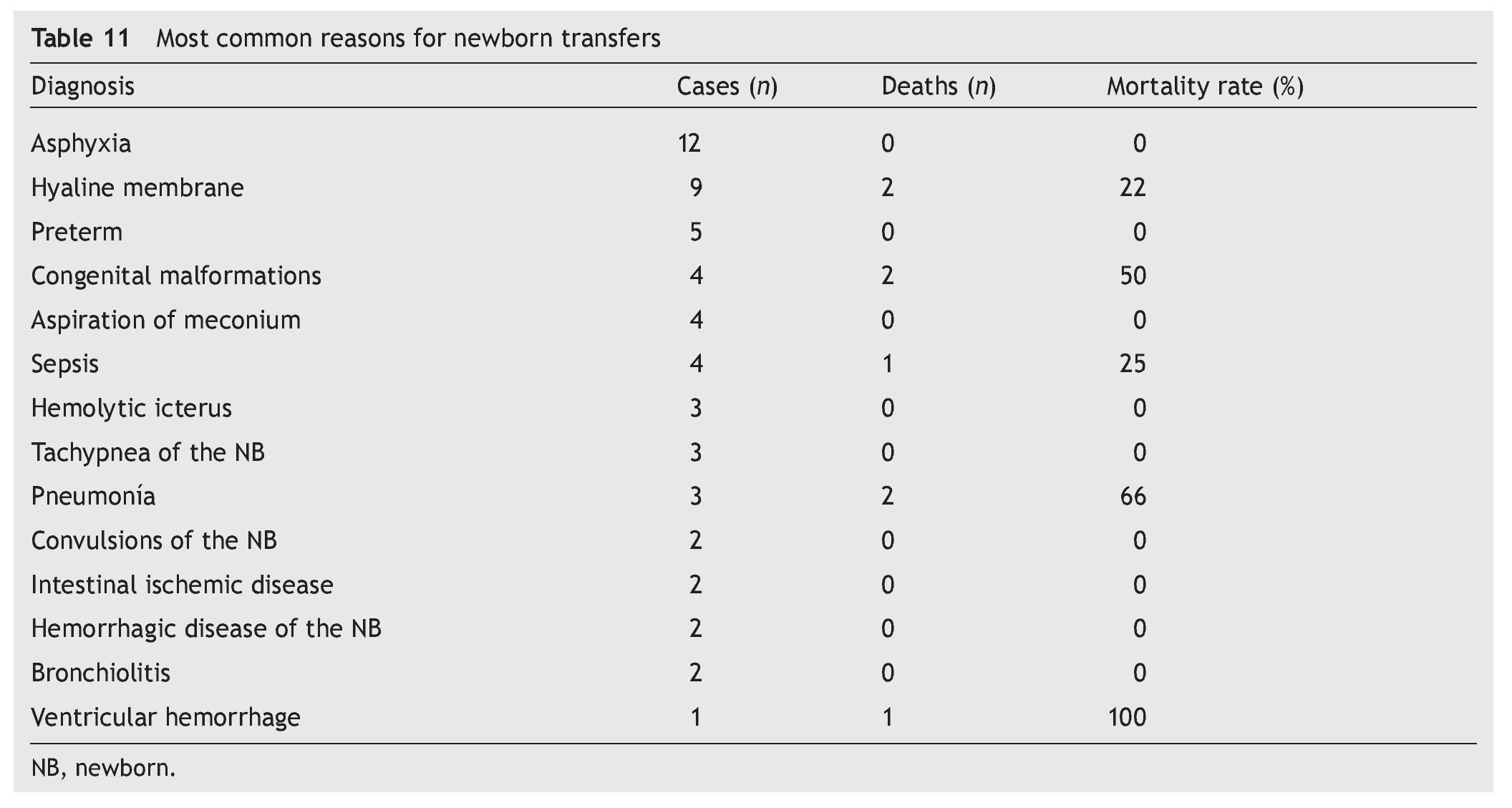
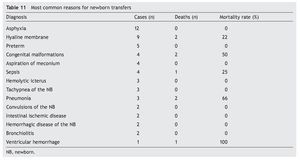
The reasons for transfer were variable. Fourteen ailments were counted of which asphyxia, hyaline membrane, prematurity, and congenital malformations stand out, explaining 53% of the transfers (Table 11).
4. Discussion
The results obtained in this study demonstrate that the TRIPS scale is a good predictor of neonatal mortality within 7 days of admission of NB transferred for medical care.
Although the hospital where the present study was done is not the only concentration facility in the area, it indirectly reflects that the rate of transfers of seriously ill NB is from 7-16/1000 births. Another interesting finding is that 34% (n = 19) of the transfers were done in the first 24 h of life, considered to be “non-programmed” or “acute”. The rate of mortality was 21% (n = 4) as opposed to the rate of mortality of the NB who were transferred with > 24 h of life, which was 11% (n = 4). A difference of p = 0.257 was observed between these groups. This confirms that adequate stabilization at the place of birth before transfer results in lower mortality.
As shown in other studies,20,21 transport services present serious defects in the care of the NB. It was observed that a high percentage of NB had hypothermia. Although a statistical relationship was not able to be demonstrated between hypothermia and mortality, it is evident that it is a serious deficiency in the quality of care of the NB. A limitation of this study was the number of medical records eliminated by not having sufficient information to complete the TRIPS score. Only 21% of the records were analyzed (n = 56). It should be noted that the information recorded, both the records with complete data as well as those with incomplete data, was similar; therefore, it was decided to publish the findings of the complete records.
Conflict of interest
The authors declare no conflicts of interest.
Funding
No external sources of funding are declared.
Received for publication: 9-29-14;
Accepted for publication: 1-27-15
http://dx.doi.org/10.1016/j.bmhimx.2015.01.008
Correspondence:
Gerardo Luna Hernández
E-mail: gerardo_luna57@yahoo.com.mx