Intramural duodenal haematoma is a rare entity that usually occurs in the context of patients with coagulation disorders. A minimum percentage is related to processes such as pancreatitis and pancreatic tumours.
Clinical caseThe case is presented of a 45 year-old male with a history of chronic pancreatitis secondary to alcoholism. He was seen in the emergency room due to abdominal pain, accompanied by toxic syndrome. The abdominal computed tomography reported increased concentric duodenal wall thickness, in the second and third portion. After oesophageal-gastro-duodenoscopy, he presented with haemorrhagic shock. He had emergency surgery, finding a hemoperitoneum, duodenopancreatic tumour with intense inflammatory component, as well a small bowel perforation of third duodenal portion. A cephalic duodenopancreatectomy was performed with pyloric preservation and reconstruction with Roux-Y.
DiscussionTreatment of a duodenal haematoma is nasogastric decompression, blood transfusion and correction of coagulation abnormalities. Surgery is indicated in the cases in which there is no improvement after 2 weeks of treatment, or there is suspicion of malignancy or major complications arise.
ConclusionsDuodenal intramural haematoma secondary to chronic pancreatitis is rare, although the diagnosis should be made with imaging and, if suspected, start conservative treatment and surgery only in complicated cases.
El haematoma duodenal intramural es una rara entidad que ocurre en pacientes con alteraciones de la coagulación; un mínimo porcentaje ocurre en procesos como los tumores pancreáticos o la pancreatitis.
Caso clínicoPresentamos el caso de un varón de 45 años, con antecedentes de pancreatitis alcohólica que acudió a Urgencias por dolor abdominal y síndrome tóxico. La tomografía computada abdominal evidenció un aumento de la segunda y la tercera porciones duodenales. Después de la esofagogastroscopia presentó choque hemorrágico. Se realizó cirugía urgente, que evidenció hemoperitoneo, tumour duodenopancreático con intensa reacción inflamatoria, así como perforación de la tercera porción duodenal. Se realizó duodenopancreatectomía cefálica con preservación pilórica y reconstrucción en Y de Roux.
DiscusiónEl tratamiento de esta entidad debe ser conservador; consiste en sonda nasogástrica, reposo digestivo y corrección de las anomalías de la coagulación. Solamente está indicada la cirugía ante el fracaso del tratamiento médico, sospecha de malignidad o complicaciones.
ConclusionesLos hematomas intramurales duodenales secundarios a pancreatitis crónica son excepcionales, si bien su diagnóstico debe realizarse con pruebas de imagen, y si se sospecha se debe iniciar tratamiento conservador, y realizar cirugía solo en los casos complicados.
The duodenal intramural haematoma is a very uncommon entity which involves a generally self-limited haemorrhage located on the submucosal layer of the wall.1 The production mechanism usually has a traumatic origin in 70–75% of the cases.2 Spontaneous haematomas appear in patients with coagulation disorders or anticoagulant therapy.3 A small percentage is related to pancreatic processes, such as pancreatitis4 and tumours.
In this clinical case, an emergency cephalic duodenopancreatectomy was performed for the treatment of an haemoperitoneum compatible, in principle, with perforated and bleeding duodenal neoplasia. We have conducted our bibliographic review based on duodenal haematoma cases, both complex and non-complex, for the assessment of the current trend regarding the choice of diagnostic tests and the approach, both conservative and surgical, adopted for their management.
Clinical caseThe patient is a 45-year old male with the following personal history: smoker of 40 cigarettes/day and drinker (4–5 beers per day and distilled drinks during the weekend), pernicious anaemia, chronic pancreatitis secondary to alcoholism. He received no anticoagulant treatments.
The patient attended the Emergency Department due to pain in the right hypochondrium with fatigue, accompanied by anorexia and weight loss by 10kg in the last 3 months. The physical examination showed icteric pigmentation of the skin and mucosas, pain upon palpation of the right hypochondrium, without peritoneal reaction.
The study conducted in the Emergency Department showed leukocytosis of 16,690μl, neutrophilia and amylase of 1003U/l. The only remarkable finding of the ultrasound scan was the presence of biliary sludge in the gallbladder and moderate dilatation of the biliary pathways (Fig. 1).
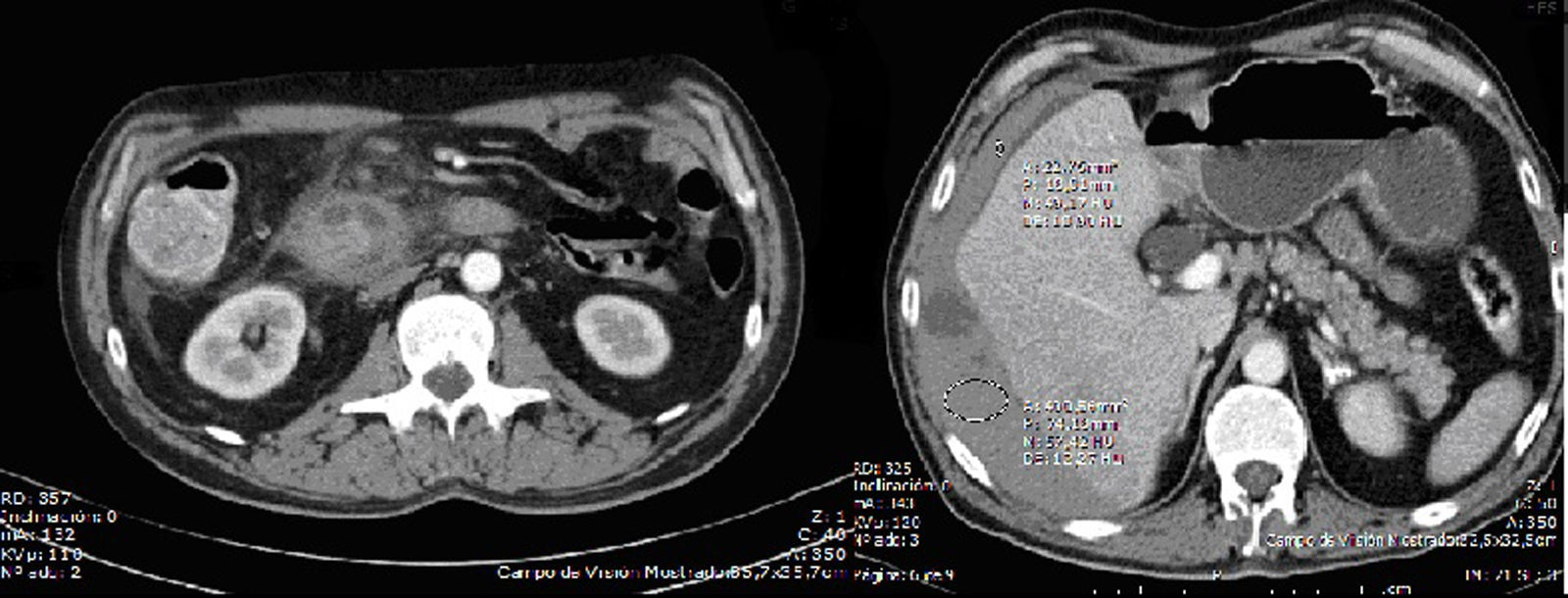
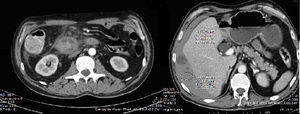
An abdominopelvic computed tomography was suggested, which confirmed the dilatation of the biliary pathways and showed an increase in the concentric thickness of the duodenal wall in the second and third segments, as well as a tumour of 2.5cm located on its main axis, which seemed to derive from Vater's ampulla, compatible with an inflammatory or neoplastic process of the pancreas; locoregional, retroperitoneal interaortocaval and left para-aortic adenopathies; rarefaction of the periduodenal fat and head margin, with uncinate process (Fig. 2).
Upon suspicion of duodenal tumour, the patient was admitted to the Digestive Department to complete the study. An oesophagogastroduodenoscopy was conducted, which showed a reduction of the calibre in the duodenum from the first to the third knee, congestion and mucosal oedema with erythematous stippling and extensive ulcers. Samples were collected for a histological study, which showed the presence of chronic duodenitis with epithelial regenerative changes and focal gastric metaplasia.
After the test, the patient worsened progressively and presented low blood pressure, tachycardia, cutaneous pallor, oliguria (200cc). Laboratory tests showed an increase in acute-phase reagents (CRP 13.6, leukocytes 20,420μl, with 86% neutrophilia). The patient presented hypovolemic shock on the third day after hospital admission. He was admitted to the Intensive Care Unit and another emergency computed tomography was conducted. This showed massive haemoperitoneum with active bleeding, which could derive from an iatrogenic perforation of the duodenal tumour.
The patient underwent an emergency intervention, which showed massive haemoperitoneum greater than 2500cc, duodenopancreatic tumour with intense inflammatory component, small bowel loops filled with blood and perforation of the third duodenal segment. The surgeon, upon suspicion of malignant duodenal tumour, although not histologically confirmed, decided to conduct a definitive surgery: cephalic duodenopancreatectomy with pyloric preservation and Roux-Y reconstruction.
The patient returned to the Intensive Care Unit, where the treatment with supportive measurements was provided. From an abdominal point of view, the progression was favourable, with drainage and suture material removal during his stay in the Intensive Care Unit (15 days).
Then, he was transferred to the Digestive System and General Surgery Department, and was discharged from the hospital eighteen days after his admission.
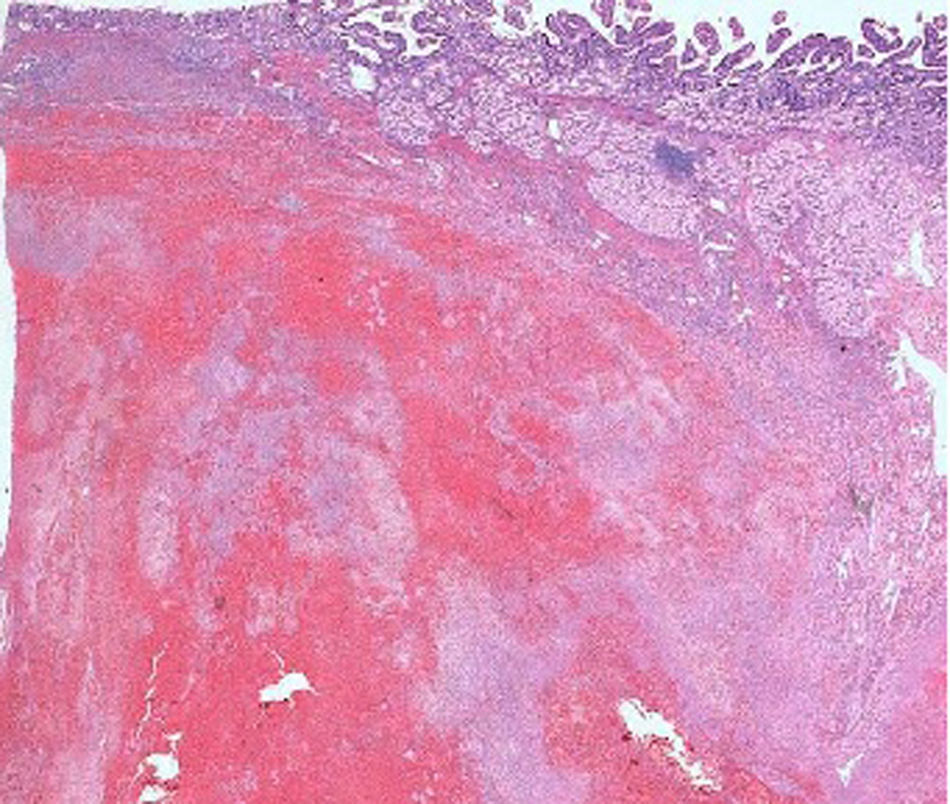
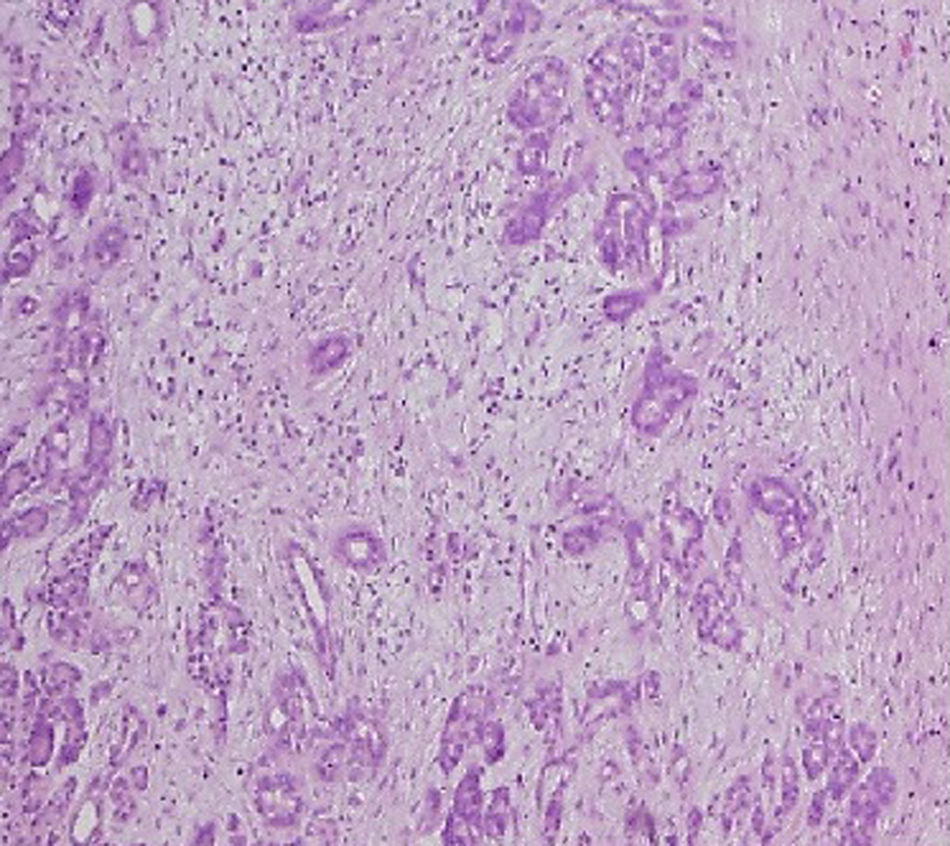
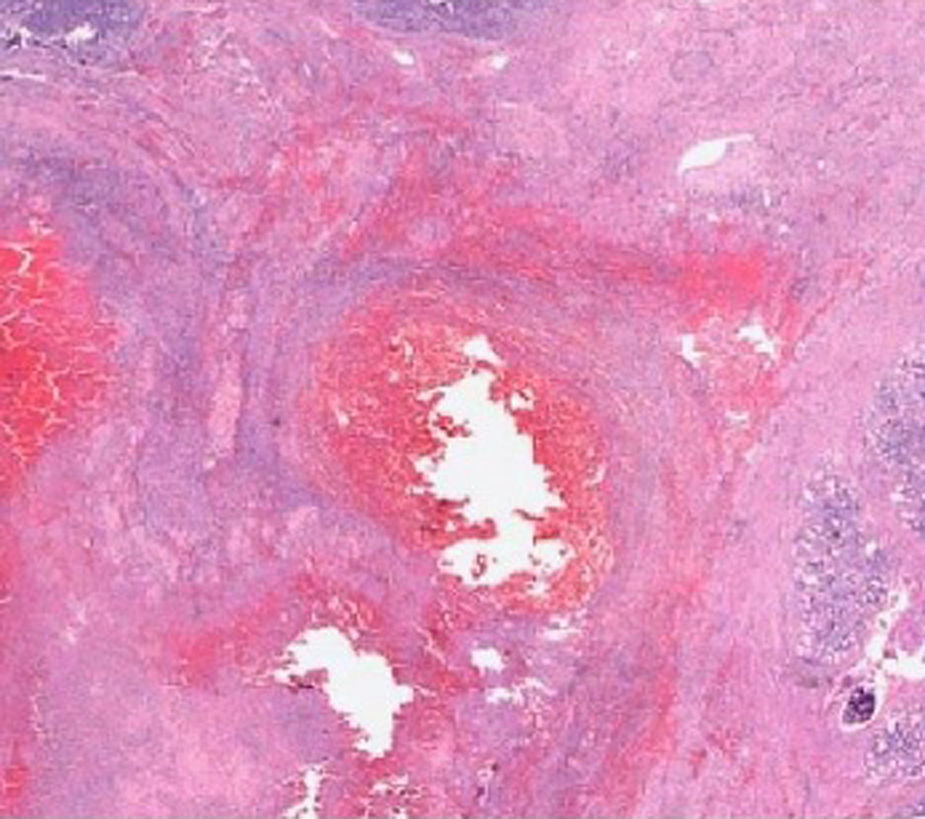
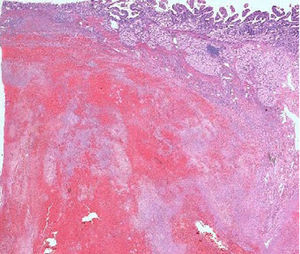
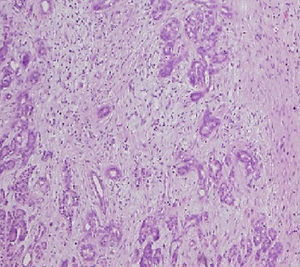
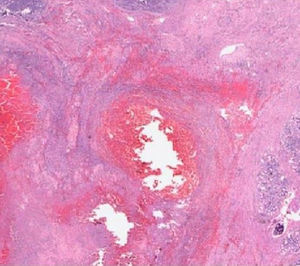
The pathological anatomy assessment indicated the presence of a greyish-brown duodenal tumour with solution of continuity (perforation), with considerable submucosal haematic collection, of 10cm long×4.5cm wide. No neoplastic processes were observed and all adenopathies were of an inflammatory nature. On a microscopic level, an organised haematoma with haemorrhage dissecting through the muscle layer, chronic pancreatitis and reactive lymphadenitis of peripancreatic lymph nodes (Figs. 3–5).
DiscussionThe first described case of duodenal haematoma was diagnosed during an autopsy by MacLauchan in 1838. The first non-traumatic case was described in 1904 by Henoch-Schönlein, in a case of blood dyscrasia. In 1908, Von Khautz diagnosed this disease in a patient with haemophilia.
Non-traumatic haematomas such as the one described are increasingly related to the consumption of anticoagulants and coagulation disorders, as well as malignant diseases, chemotherapy and inflammatory and autoimmune processes.5
Until now, the exact mechanism for how the pancreas induces a duodenal haematoma has not been discovered. There are 2 hypotheses on the subject: firstly, the presence of ectopic pancreatic tissue inside the duodenum wall can develop a severe inflammation, followed by necrosis and haematoma formation; secondly, the release of pancreatic enzymes in pancreatitis can damage duodenal blood vessels.5
The clinical presentation is variable, and it may start with: abdominal pain of different intensities, mechanical ileus, intestinal obstruction6 and, on some occasions, with hypovolemic shock due to hemoperitoneum, as in the case at hand.7
For its diagnosis, a certain degree of suspicion is required in the first place; imaging tests such as computed tomographies or echoendoscopies add information that helps confirm it, although there are no findings that can be qualified as pathognomonic.8
Computed tomography studies show a circumferential thickening of the duodenal wall, the narrowing of the lumen and the obstruction of intestinal transit.8
In our patient, the fact that he began with obstructive jaundice, weight loss by 10kg, asthenia and anorexia, as well as the findings from the computed tomography which showed an image compatible with duodenal tumour, led to the initial suspicion of a neoplastic process. It is difficult to obtain a diagnosis of certainty in these cases because, on one hand, pancreatitis may produce changes in the duodenal wall that may simulate a neoplastic process9 and, on the other hand, duodenopancreatic neoplasias are not uncommon in patients with chronic pancreatitis.10 Sometimes, lesions are ulcers, mucosal oedema or haemorrhage stippling. In these cases, some authors contraindicate biopsies to avoid secondary complications and allow the progression of the clinical symptoms to determine the therapeutic approach to be adopted.11
The therapeutic approach will depend on the progression of the clinical symptoms. The fact that this evidenced a neoplasia justified the collection of biopsy samples during the endoscopy and, judging by the progressive sequence of the patient, this may have led to duodenal perforation.
In principle, the treatment of a duodenal haematoma, even with an obstruction, is medical and consists of digestive rest, nasogastric decompression, blood transfusion and correction of existing coagulation anomalies. Surgery is indicated in cases in which there is no improvement after two weeks of treatment, suspicion of neoplasia, or occurrence of major complications.12 In our case, two of these circumstances were present, since the suspected diagnosis was a malignant tumour and there was perforation.
The surgical technique to be conducted is also controversial. Some authors currently choose endoscopic drainage.13 The cephalic duodenopancreatectomy is a difficult technique which presents a high morbidity and mortality if conducted as an emergency procedure. Asensio et al.14 advocate a damage control surgery and, afterwards, a definitive one; in their series about 18 emergency cephalic duodenopancreatectomies due to duodenopancreatic traumatism, the mortality rate amounted to 44.5% (6 deaths on the operating table and 2 deaths occurring 48h later), although this series involved patients with severe duodenopancreatic traumatisms. For this patient, a duodenal suture with serous patch, drainage of the perforation using a Pezzer-type tube or another more conservative approach could have been implemented, apart from controlling the haemorrhage and conducting a washout of the cavity. However, uncertainty about the reason for the bleeding and the possibility of neoplasia led to definitive surgery as our first choice.
ConclusionsDuodenal intramural haematomas secondary to chronic pancreatitis are very uncommon. Although their diagnosis must be confirmed through imaging tests, the first step is to suspect their presence. The initial management of this disease, as described in the medical literature, must involve a conservative approach, and surgery must only be conducted in the presence of complications.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Molina-Barea R, Pérez-Cabrera B, Hernández-García MD, Navarro-Freire F, Jiménez-Ríos JA. Abdomen agudo por haematoma duodenal intramural complicado. Presentación de un caso y revisión en la literatura. Cir Cir. 2015; 83: 146–150.