Ureterocele is a cystic dilation of the distal ureteral segment. The incidence in women ranges from 1/5000 to 1/12,000. In adults, they are poorly diagnosed and are asymptomatic. Prolapse through the urethra is uncommon, and involves acute urine retention and a reducible vulvar tumour.
Clinical caseWoman of 24 years old, two previous caesarean and two abortions. She had incomplete bladder emptying, intermittent voiding, bladder straining and tenesmus, three months before admission. After the voiding effort she presented with acute urine retention with sudden onset of tumour in the vulva. The tumour was manually reduced under regional anaesthesia. A cystoscopy was performed, finding an ischaemic de-roofing of the anterior wall of the ureterocele, causing vesicoureteral reflux grade IV. Surgical correction was performed with Cohen re-implantation and insertion of a double-J catheter. The catheter was removed 30 days later, with a successful post-operative course.
DiscussionIts aetiology is unclear, and most are diagnosed by ultrasound in the prenatal period. The clinical presentation is variable, from urinary tract infection to prolapse. Despite its size, it may cause complications such as ischaemic de-roofing, which if diagnosed soon may be resolved successfully, as with this patient.
ConclusionThe results and treatment may be favourable when no renal impact or concomitant anatomical changes are present, as is the case of this patient.
Ureterocele es la dilatación quística de la porción distal del segmento ureteral. La incidencia en mujeres varía entre 1/5,000 a 1/12,000. En adultos, son poco diagnosticados, permanecen asintomáticos y su prolapso a través de la uretra es poco común, condicionando en la mujer retención aguda de orina y un tumor vulvar reducible.
Caso clínicoMujer de 24 años, con 2 cesáreas y 2 abortos. Presenta, 3 meses antes de su ingreso, sintomatología urinaria baja, vaciamiento vesical incompleto, intermitencia miccional, pujo y tenesmo vesical; posterior al esfuerzo miccional cursó con retención aguda de orina y aparición súbita de tumoración vulvar. Acude a la unidad médica que le corresponde, donde se le reduce manualmente dicha tumoración bajo anestesia regional, se regional, así mismo se le realizó cistoscopia encontrando destechamiento isquémico de la pared anterior de ureterocele lo cual condicionó reflujo vesicoureteral derecho grado IV, por lo que se le realizó reimplante ureteral tipo Cohen y colocación de catéter doble-J ipsilateral; a los 30 días se retira el catéter doble-J y la evolución fue satisfactoria.
DiscusiónSu etiología no es clara, la mayoría son diagnosticados a través de ultrasonido prenatal. Los cuadros de presentación son muy variables, desde infección de vías urinarias de repetición hasta el prolapso, que a pesar de su reducción puede ocasionar complicaciones como reflujo vesicoureteral secundario al destechamiento isquémico, que de ser diagnosticado y manejado oportunamente no altera la función renal de los pacientes.
ConclusiónEl tratamiento y los resultados son favorables cuando no hay repercusión renal, ni alteraciones anatómicas concomitantes, como en el caso de esta paciente.
Ureterocele is a cystic dilation of the distal ureteral segment. The majority of ureteroceles are ectopic and are associated with duplicated collecting systems. The incidence of ureterocele in women ranges from 1/5000 to 1/12,000, and there is a rising tendency due to the generalised use of ultrasound in prenatal screening.1 Ureteroceles in adults are rarely diagnosed and generally asymptomatic. Prolapse through the urethra is uncommon and involves acute urine retention and a reducible vulvar tumour in women.2
We are reporting a case of ureterocele in a young adult woman: its evolution, complication and treatment.
Clinical caseA 24 year old woman, from Puebla, Mexico. She was single, educated to a low level, and was a housewife. She had previously had 2 caesarean sections and 2 abortions, the reasons for which were unknown. She started having periods at the age of 12, with irregular menstrual cycles and the date of her last menstruation had been a month prior to admittance. The contraceptive method she was using was a copper type T intrauterine device.
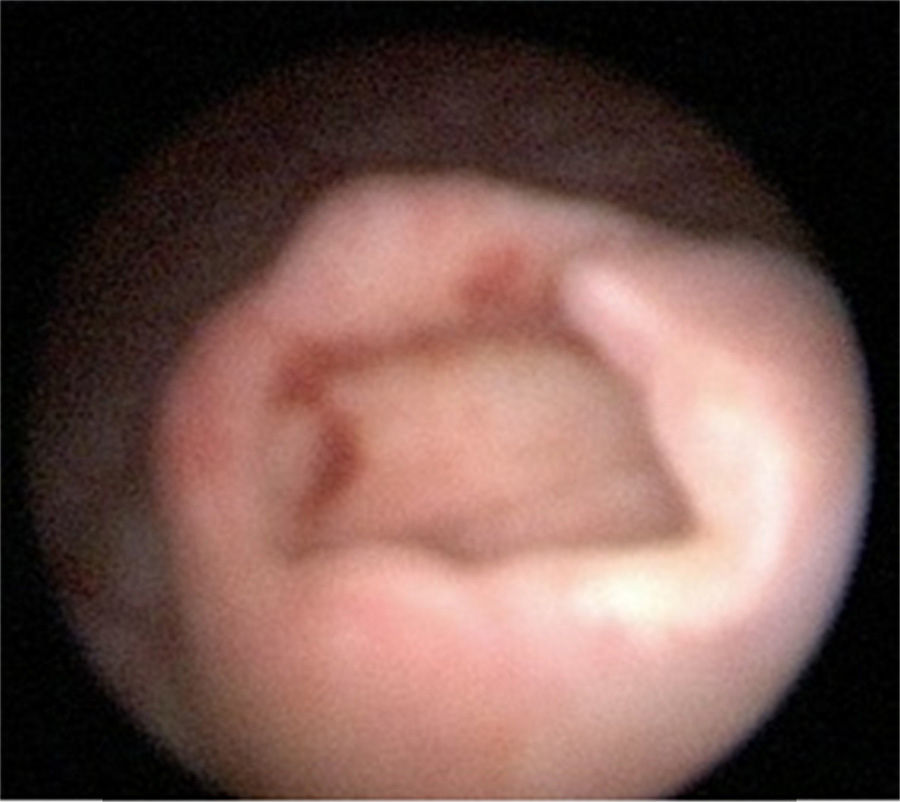
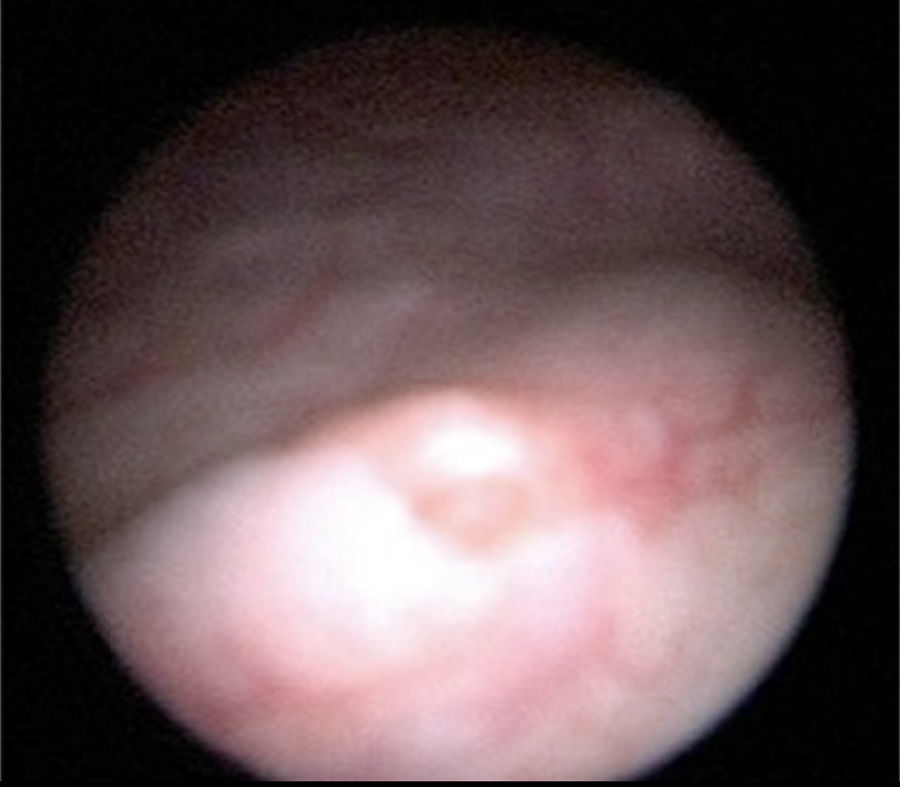
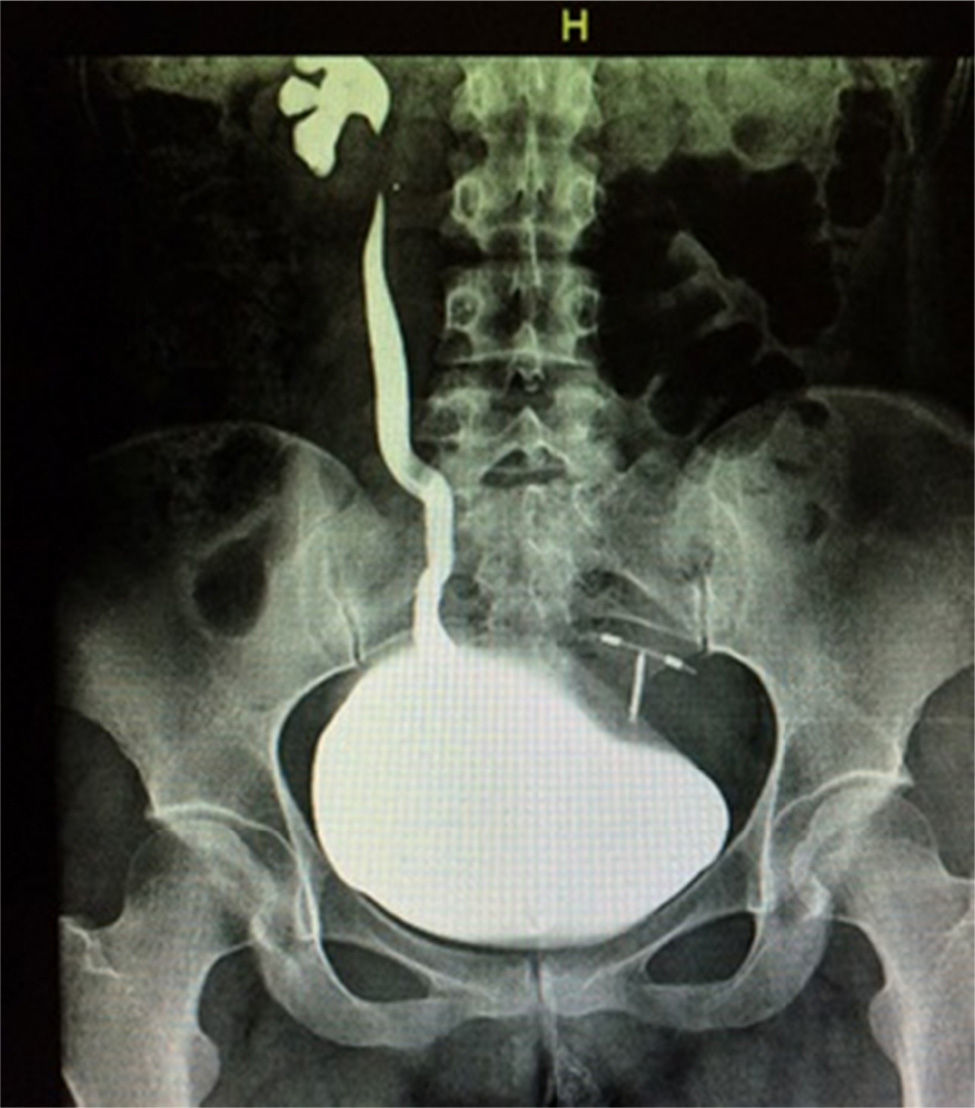
She presented with lower urinary tract symptoms 90 days prior to admittance, characterised by symptoms of incomplete bladder emptying, intermittent voiding, bladder straining and tenesmus. After the voiding effort she presented with acute urine retention with sudden onset of tumour in the vulva, which persisted for 20h, and was the reason why she decided to go to the emergency services. Physical examination revealed: patient with painful facies, low abdominal pain with palpable vesical globe, and a tumour 5×7×3cm diameter at vulvar level which was dark red in colour, ischaemic in appearance, painful when moved, of rubbery, renitent consistency and which protruded from the urethra. The tumour was manually reduced under regional anaesthesia and a Foley No. 16Fr catheter was inserted, which led to the obtaining of cloudy, residual, concentrated and foetid urine (Fig. 1).
The patient was admitted to hospital for medical attention with antibiotic, antispasmodic and anticholinergic drugs and so that a urotomography could be performed. The latter showed a giant right ureterocele with no additional anatomic changes. The patient evolved satisfactorily, and was therefore discharged with her Foley catheter, and 8 days later a cytoscopy was performed which showed ischaemic detachment of the anterior wall of the right ureterocele (Fig. 2), a normal contralateral ureter (Fig. 3) and right vesicoureteral reflux grade IV which was confirmed by cystourethrogram (Figs. 4 and 5). Surgical correction was performed with Cohen re-implantation and insertion of a double-j catheter. The catheter was removed one month later. After 3 months the patient was asymptomatic and urine culture and general examination tested normal.
DiscussionThere are many classifications for ureteroceles, but the most useful one for clinical practice is to divide them into intravesical and extravesical. The intravesical ones are found completely inside the bladder and above the vesical neck, as in the case presented. Aetiology is unclear, but there is a relationship of ectopic ureter pathogenesis with or without ureterocele, the development of the trigonal ureteral and renal residues. The majority of ureteroceles and ectopic ureter are diagnosed through prenatal ultrasound. Presentation may be very varied, from urinary tract infection, urinary incontinence, tenesmus, bladder straining, incomplete bladder emptying, supra-pubic pain, up to the prolapsed of the ureterocele, similar to that reported in this case. Diagnosis by imaging may be made with ultrasound, multislice axial tomography and nuclear magnetic resonance.3–6
The secondary ischaemic de-roofing which presented in our patient at the time of evolution conditioned the vesicoureteral reflux grade IV as a complication. This did not permanently affect kidney function, since surgical treatment (right ureteral reimplantation) was successfully performed.
ConclusionThe outcome and appropriate treatment of the ureterocele may be favourable when no renal impact or concomitant anatomical changes are present, as was the case of this patient. She was able to maintain renal function and there were no signs of urinary tract infection.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Villagómez-Camargo R, Chopin-Gazga M, Saucedo-Bravo J, García-Cano E, Montiel-Jarquín Á. Retención aguda de orina secundaria a prolapso de ureterocele gigante en una mujer adulta joven. Informe de un caso. Cir Cir. 2016;84:336–339.