Primary empty sella is a herniation of the sellar diaphragm into the pituitary space. It is an incidental finding and patients may manifest neurological, ophthalmological and/or endocrine disorders. Episodes of vertigo, dizziness, and hearing loss, have been reported.
ObjectiveTo determine the conditional probability, as well as the statistical dependency, through the Bayesian analysis in patients with primary empty sella and audiovestibular disorders.
PatientsIndividuals who attended the National Rehabilitation Institute from January 2010 to December 2011, diagnosed with primary empty sella and audiovestibular disorders.
Material and methodsAn analysis was performed on a sample of 18 patients with a diagnosis of primary empty sella confirmed with magnetic resonance studies and who had signs of vertigo, hearing loss and dizziness.
ResultsOf the 18 patients studied, 3 (16.66%) had primary empty sella as the only clinical evidence. In 9 patients (50%) empty sella was associated with vertigo, and 16 patients (88.88%) were diagnosed with hearing loss, with sensorineural hearing loss being the most frequent (77.77%). The intersection between the proportions of primary empty sella with the presence and type of hearing loss was calculated. Thus for sensorineural hearing loss, the calculated ratio was P(AB)=0.6912, and for conductive and mixed hearing loss the value of P(AB)=0.0493 in both cases.
ConclusionsBayesian analysis and conditional probability enables the dependence between two or more variables to be calculated. In this study both mathematical models were used to analyse comorbidities and audiovestibular disorders in patients diagnosed with primary empty sella.
El aracnoidocele selar es una herniación del diafragma selar hacia el espacio hipofisario, es un hallazgo incidental y los pacientes pueden manifestar trastornos neurológicos, oftalmológicos y/o endocrinológicos, así como episodios de vértigo, mareo e hipoacusia.
ObjetivoDeterminar la probabilidad condicional, así como la dependencia estadística por medio del análisis bayesiano en pacientes con aracnoidocele selar y enfermedad audiovestibular.
PacientesIndividuos que acudieron al Instituto Nacional de Rehabilitación entre enero de 2010 a diciembre de 2011, con diagnóstico de aracnoidocele selar y enfermedad audiovestibular.
Material y métodosSe analizó una muestra conformada por 18 pacientes con diagnóstico de aracnoidocele selar, confirmado con estudios de resonancia magnética y que manifestaron vértigo, hipoacusia y mareo.
ResultadosTres (16.66%) pacientes presentaron aracnoidocele selar como única evidencia clínica; en 9 (50%) pacientes se asoció con vértigo; 16 (88.88%) se diagnosticaron con hipoacusia, la sensorineural fue la más frecuente con el 77.77%. Se calculó la intersección entre las proporciones de aracnoidocele selar con la presencia y el tipo de pérdida auditiva, así para la hipoacusia sensorial, la proporción fue P(A∩B)=0.6912 y para la hipoacusia conductiva y mixta el valour de P(A∩B)=0.0493 en ambos casos.
ConclusionesEl análisis bayesiano y de probabilidad condicional permiten calcular la dependencia entre 2 o más variables; en este estudio se utilizaron ambos modelos matemáticos para analizar las comorbilidades y las enfermedades audiovestibulares en pacientes diagnosticados con aracnoidocele selar.
Empty sella syndrome is defined as herniation of the sellar diaphragm, which allows the arachnoid and cerebrospinal fluid to enter the cavity which houses the hypophysis,1 it is also known as primary empty sella.2 Primary empty sella is associated with possible congenital malformation of the sellar and suprasellar diaphragm, when there is no history of a previous pathological condition3; it is also due to intermittent increases of intracranial pressure and to volumetric changes in the pituitary gland, frequently observed during the gestation period.4 Secondary empty sella is more common and is caused by tumours, chiefly adenomas which degenerate into spontaneous necrosis (ischaemia or haemorrhage), and by surgical procedures, infectious processes, autoimmune disease, trauma, drugs, radiotherapy and pharmacological treatments.3,4 It has been reported that primary empty sella presents as an incidental finding in approximately 5.5% of patients when a necropsy is performed,4 with a female to male ratio of 5:1, and predominates in patients between the fourth and fifth decades of life.2
The sellar diaphragm is a deflection of the dura mater which separates the suprasellar cistern from the pituitary fossa (sella turcica); this diaphragm also allows the pituitary stalk to pass through a very small opening in its centre. Increased pressure in the suprasellar subarachnoid space, or a reduction in the size of the pituitary predispose to the development of an intrasellar subarchnoid hernia. When the sellar diaphragm is incomplete, cerebrospinal fluid exerts pressure on the suprasellar cistern, the pituitary gland and the optic chiasm.5
Various factors are associated with changes in the size of the pituitary gland, which cause the suprasellar subarachnoid space to expand or decrease, for example, an increase in the size of the pituitary gland is observed during pregnancy4; in women in the fourth decade of life, involution of the pituitary has been observed associated with the menopause, which explains why this syndrome predominates in women. On occasion, when glands such as the thyroid, the adrenal glands and the gonads hyperfunction, the pituitary gland presents compensatory hypertrophy to rectify the hormonal deficiency, subsequently the pituitary gland involutes leaving an “empty sella” as a sequela.5
Pathological hypopituitarism can occur in Sheehan's syndrome (due to postpartum haemorrhage) or in patients with vascular disease, causing pituitary necrosis in both cases, it has also been associated with pituitary apoplexy due to idiopathic intracranial hypertension, surgery, thrombosis, meningitis, hydrocephaly, Chiari malformation, cranial trauma and adenomas. It is also worth mentioning that the pituitary gland has a considerable blood supply; this provides us with a better understanding of some of the causes of primary empty sella.5–8
Obesity is another cause of primary empty sella; there is a decrease in thoraco-pulmonary distensibility in obese patients, with increased intra-abdominal and intra-thoracic pressure, and hypoxia and hypercapnia present in varying degrees, as a consequence, idiopathic intracranial hypertension presents due to the increased pressure exercised by the cerebrospinal fluid, which influences the primary empty sella.2,3,9,10
Primary empty sella is an incidental radiological finding and may or may not present symptoms. The main clinical manifestations are neurological, ophthalmological and/or endocrinological disorders.
The predominant symptom is headache; several authors report between 60% and 80% of cases, and it is the main reason for imaging tests2,3,11; pain is chronic, asymmetric, moderately intense and chiefly referred to the anterior part of the skull.6 Visual disturbances can be severe, presenting decreased visual acuity, altered visual field, tunnel vision, scotoma, bitemporal hemianopsia and quadrantopia.2 An incidence of visual disturbances which varies between 1.6% and 16% has been reported in patients with primary empty sella.6 Visual disturbances are due to herniation of the subarchnoid space, which causes an alteration in the anatomical relationship between the optic tracts and the sellar region, causing dislocation of the optic chiasm and/or compression of the optic nerve.6,12
In hypopituitarism, as a cause of primary empty sella, the clinical manifestations depend on increased or decreased hormone production, the most common hormones involved are: thyroid stimulating hormone, growth hormone, gonadotropic hormone, adrenocorticotropic hormone, prolactin and antidiuretic hormone13; Guitelman et al.2 reported that 27% of hypopituitarism cases were associated with primary empty sella. Rani et al. in 201314 describe the biochemical and hormonal conditions associated with primary empty sella, such as hypocortisolaemia in 62.5%, hypothyroidism in 50%, hypogonadism 18.75%, hyperprolactinaemia in 18–75%, and growth hormone deficiency 12.5%.
There are 3.5/100,000 women world-wide aged between 15 and 44 with benign intercranial hypertension due to pressure from cerebrospinal fluid (>200mm/H2O) on the pituitary gland and stalk, as a consequence, they present symptoms such as tinnitus, headache and visual disturbances.15
Primary empty sella is an incidental histopathological finding, as mentioned above, and can be associated with audiological and/or vestibular symptoms. In the study by Boleaga-Durán and Guzmán-Nuquez,16 it is reported that 40% of patients with primary empty sella confirmed by magnetic resonance experience episodes of vertigo. Guitelman et al.,2 for their part, demonstrated that 18.4% of patients with primary empty sella experienced dizziness.
Pulsatile tinnitus presents in idiopathic intracranial hypertension associated with primary empty sella, which, in most cases is unilateral with neither side predominating.3,15 In terms of audiovestibular signs, the case of a patient has been reported with hearing loss combined with a diagnosis of empty sella and pituitary adenoma; the hearing loss was initially right-sided and progressed to bilateral hearing loss over the course of 4 years.17
Another study describes the case of a patient with disabling tinnitus, hearing loss and headache; the onset of tinnitus was associated with sudden hearing loss and vertigo, the magnetic resonance images showed adequate integrity of the cochlea and cranial nerves, contrast showed herniation of the suprasellar cistern.18
Other clinical manifestations observed in patients with primary empty sella syndrome are associated with hormonal changes, changes in mood, depression and fatigue.19
Endocrine, neurological, visual, and metabolic disturbances have been widely described in literature in patients diagnosed with primary empty sella, however there a few studies which report findings of audiovestibular symptoms.
The objective of this study is to determine conditional probability, and statistical dependence by Bayesian analysis, in patients with primary empty sella and audiovestibular disease.
Material and methodsStudy typeTransversal, descriptive.
Sample typeGiven the conditions of the study, a census-type sample was taken, selecting patients who attended the Instituto Nacional de Rehabilitación (INR) during the period between 11 January 2010 and 16 December 2011, all the patients had been diagnosed with primary empty sella and audiovestibular disease. The sample size comprised 18 patients.
Study patientsAdult patients of either gender, diagnosed with an audiological otoneurological disease, with the presence or otherwise of concomitant diseases: such as arterial hypertension, diabetes mellitus, suspicion or diagnosis of an endocrinopathy, visual disturbances, headache or depression, with complete electronic patient records which had been evaluated in the Audiology and Otoneurology Department of the INR reporting: dizziness, vertigo, unilateral or bilateral tinnitus, isolated or accompanied by hearing loss, regardless of its cause. Minors, patients with a history of central nervous system or hypothalamus–pituitary disease, who had been under medical or surgical treatment for pituitary disease, for adenomas and ischaemic processes of the pituitary, or for exposure to radiation to the head and neck, were excluded from the study.
ProcedureThe records of 200 patients who attended the Audiology and Otoneurological Department of the Instituto Nacional de Rehabilitación, reporting feelings of vertigo and/or dizziness; all the patients had undergone magnetic resonance imaging in order to confirm that their otoneurological disease was not of central origin. Magnetic resonance was performed using General Electric Systems, Signa HDxt Gemsow scanner, obtaining images of the skull and posterior fossa, and angioresonance and magnetic resonance venography images for the patients who required them. Axial, coronal and sagittal slices were analysed to make a diagnosis of primary empty sella with T1, T2-weighted images, T2-weighted Fluid Attenuation Inversion Recovery Fast Imaging Employing Steady-state Acquisition (FLAIR FIESTA).
Of the 200 patients who underwent MRI scanning, 18 were confirmed with a diagnosis of primary empty sella. Then the following specialised tests were performed on the patients to assess their audiovestibular function: general physical examination, visual acuity tests, ocular movement tests: fixation (spontaneous nystagmus), maintenance (evoked nystagmus), monitoring, convergence, optokinetic nystagmus, suppression of nystagmus, and examination with Fresnel lenses for induced and spontaneous nystagmus, Dix-Hallpike manoeuvre, assessment of cranial nerves (V, VII, VIII, IX, X, XI, XII) and sensory and motor examination, by muscle tone, gait and balance tests, and thermal (caloric) tests. Auditory function was assessed with impedance audiometry and audiometry.
Contingency tables were constructed using the data obtained in order to make an analysis of joint probability and dependence using Bayesian analysis.
ResultsFrom the sample comprising 18 patients, 16 (88.88%) were female with an average age of 55.56±11.79 years and 2 (11.11%) were male with an average age of 68±9.89 years (average±standard deviation), the average age of the entire sample was 61.78±10.77 years.
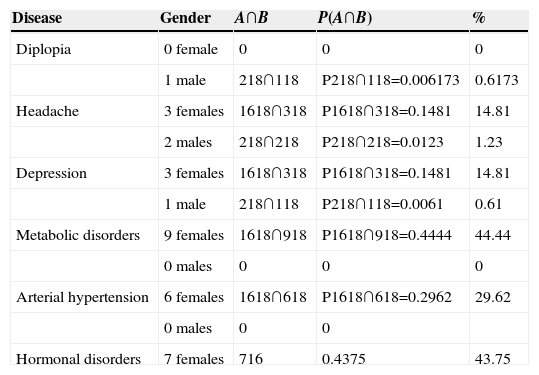
In order to analyse the joint probability between clinical manifestations and pituitary dysfunction in patients with primary empty sella, the intersection of these proportions was calculated P(A∩B)=P(A)·P(B), where A and B were calculated with the proportion to be analysed, for example: gender between the total sample and the disease to be analysed between the sample total as well, in order to establish the probability with respect to gender and disease with respect to the sample studied, thus, for the calculations the male gender proportion was (2/18) 11.11% and the female gender (16/18) 88.88%. The joint probability with respect to some comorbidities was: male patients (A) 11.11% (2/18) with diplopia (B) 5.5% (1/18) and primary empty sella was P(A∩B)=0.0061 or 0.61%; in the case of patients reporting headache (3/18) were female and (2/18) male, and therefore the joint probability for these variables was: P(A∩B)=0.1481 or 14.81% for women and P(A∩B)=0.0123 or 1.23% for men; with regard to episodes of depression (3/18) 16.66% female patients and (1/18) male patients 5.5% reported suffering them, therefore P(A∩B)=0.1481 or 14.81% for women and P(A∩B)=0.0061 or 0.61% for men; moreover, (9/18) 50% of the women were diagnosed with metabolic disturbances, their joint probability being P(A∩B)=0.4444 or 44.44%, on analysing the intersection between gender and hypertension, (6/18) 33.33% women were diagnosed with a probability of P(A∩B)=0.2962 or 29.62%, i.e., female patients with hypertension, finally (7/16) 43.75% women presented hormonal disturbances (Table 1).
Joint probability between gender and reported diseases.
| Disease | Gender | A∩B | P(A∩B) | % |
|---|---|---|---|---|
| Diplopia | 0 female | 0 | 0 | 0 |
| 1 male | 218∩118 | P218∩118=0.006173 | 0.6173 | |
| Headache | 3 females | 1618∩318 | P1618∩318=0.1481 | 14.81 |
| 2 males | 218∩218 | P218∩218=0.0123 | 1.23 | |
| Depression | 3 females | 1618∩318 | P1618∩318=0.1481 | 14.81 |
| 1 male | 218∩118 | P218∩118=0.0061 | 0.61 | |
| Metabolic disorders | 9 females | 1618∩918 | P1618∩918=0.4444 | 44.44 |
| 0 males | 0 | 0 | 0 | |
| Arterial hypertension | 6 females | 1618∩618 | P1618∩618=0.2962 | 29.62 |
| 0 males | 0 | 0 | ||
| Hormonal disorders | 7 females | 716 | 0.4375 | 43.75 |
It can be seen that metabolic disorders and hypertension were only found in females.
On assessing body condition and gender, 15 patients of the sample were overweight, (13/18) 72.22% were female and (2/18) 11.11% were male, their joint probability being P((16/18)∩(13/18))=64.16% for women and P((2/18)∩(2/18))=1.23% for men.
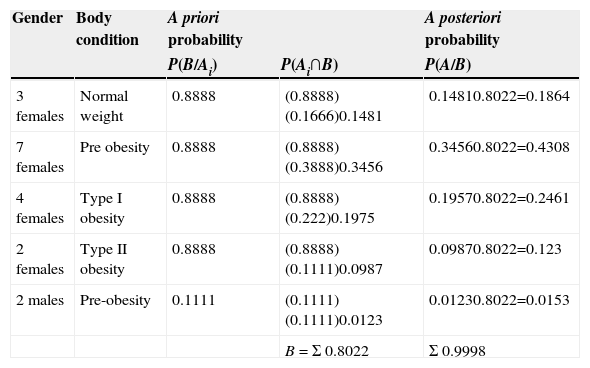
Bayes’ theorem was used to establish the conditional probability between primary empty sella and excess weight in the patients studied, P(Ai/B)=(P(Ai∩B))/(P(B)) as well as for calculating joint probability the value was taken for women of (16/18) and (2/18) for men, thus this probability was calculated by means of the product of gender proportion multiplied by the body condition proportion (normal weight, pre-obesity, type I obesity and type II obesity) with respect to the total sample (n=18); thus, (3/18) 16.66% of the women were of normal weight, and therefore the a posteriori probability was P(A/B)=0.1846, or 18.46% were women of normal weight diagnosed with primary empty sella, in the case of the pre-obese patients (7/18) 38.88% were women, obtaining an a posteriori probability of P(A/B)=0.4308, i.e., 43.08% of the women of the sample with primary empty sella were pre-obese; with respect to the patients with type I obesity (4/18) 22.22% the calculated value for the a posterior probability was P(Ai/B)=0.2461, 24.61%, i.e., of being a woman, with type I obesity and diagnosed with primary empty sella; whereas for the patients with type II obesity (2/18) 11.11% the value obtained was P(Ai/B)=0.123, i.e., 12.3% were women with type II obesity and diagnosed with primary empty sella. With regard to the male patients (2/18) 11.11% were diagnosed with pre-obesity, therefore P(A/B)=0.0153, i.e., 1.53% were pre-obese males diagnosed with primary empty sella. It is worth noting that the largest proportion was found in the pre-obese women with P(A/B)=0.4308 (Table 2).
Expected probability in obese patients. Bayesian analysis.
| Gender | Body condition | A priori probability | A posteriori probability | |
|---|---|---|---|---|
| P(B/Ai) | P(Ai∩B) | P(A/B) | ||
| 3 females | Normal weight | 0.8888 | (0.8888) (0.1666)0.1481 | 0.14810.8022=0.1864 |
| 7 females | Pre obesity | 0.8888 | (0.8888) (0.3888)0.3456 | 0.34560.8022=0.4308 |
| 4 females | Type I obesity | 0.8888 | (0.8888) (0.222)0.1975 | 0.19570.8022=0.2461 |
| 2 females | Type II obesity | 0.8888 | (0.8888) (0.1111)0.0987 | 0.09870.8022=0.123 |
| 2 males | Pre-obesity | 0.1111 | (0.1111) (0.1111)0.0123 | 0.01230.8022=0.0153 |
| B=Σ 0.8022 | Σ 0.9998 |
The a posteriori probability can be seen between body weight and gender with the precondition that they have been diagnosed with primary empty sella, where the highest proportion is in pre-obesity and the female gender.
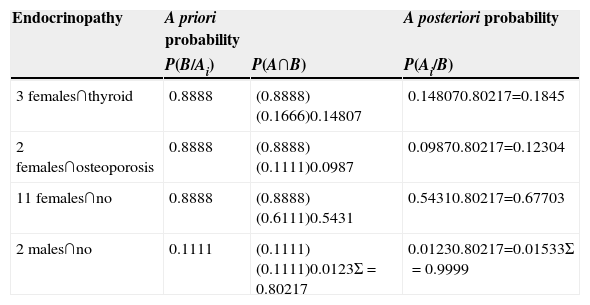
The pituitary gland is directly associated with endocrine function. In patients with primary empty sella the proportion of endocrinopathies was analysed with respect to the number of women in the sample, therefore n=11. Where (2/16) 12.5% presented menstrual disturbances, (3/16) 18.75% thyroid disorders, (2/16) 12.5% osteoporosis and (9/16) 56.25% reported no endocrine disorders.
The a posteriori probability was calculated by Bayesian analysis in order to find out the dependence between the endocrinological diseases and gender with primary empty sella; thus in patients with thyroid disorders (3/8), 16.66% with primary empty sella, the a posteriori probability was P(A/B)=0.1845 or 18.45%; with respect to patients with osteoporosis (2/18) 11.11%, the a posteriori probability obtained was P(A/B)=0.123 or 12.3%, on making the calculation of a posteriori probability for patients not presenting endocrine disorders (11/18) 61.11% it was P(Ai/B)=0.6770 or 67.70%. Finally, (2/18) 11.11% of male patients did not report endocrine disorders, therefore the a posteriori probability was P(A/B)=0.0153 or 1.53% (Table 3).
Bayesian analysis between endocrinopathies, gender and primary empty sella.
| Endocrinopathy | A priori probability | A posteriori probability | |
|---|---|---|---|
| P(B/Ai) | P(A∩B) | P(Ai/B) | |
| 3 females∩thyroid | 0.8888 | (0.8888) (0.1666)0.14807 | 0.148070.80217=0.1845 |
| 2 females∩osteoporosis | 0.8888 | (0.8888) (0.1111)0.0987 | 0.09870.80217=0.12304 |
| 11 females∩no | 0.8888 | (0.8888) (0.6111)0.5431 | 0.54310.80217=0.67703 |
| 2 males∩no | 0.1111 | (0.1111) (0.1111)0.0123Σ=0.80217 | 0.01230.80217=0.01533Σ=0.9999 |
The a posteriori probability can be seen in the patients studied diagnosed with primary empty sella, gender and endocrinopathologies, where the greatest a posteriori probability is not having an endocrinopathology associated with primary empty sella.
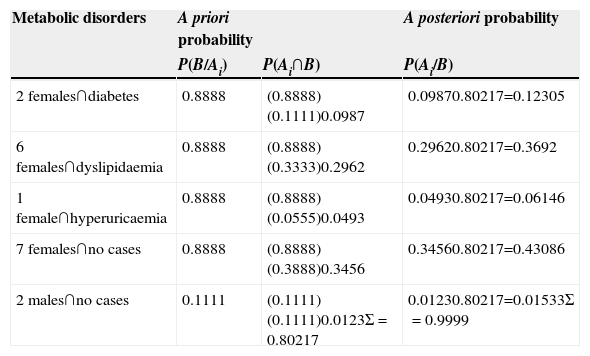
Bayes’ theorem was used to evaluate the a posteriori probability between gender, the presence or absence of metabolic diseases and primary empty sella, obtaining an a posteriori probability of P(A/B)=0.123 for patients with diabetes and primary empty sella manifested in (2/18) 11.11%; (6/18) 33.33% women were diagnosed with dyslipidaemia, obtaining an a posteriori probability of P(A/B)=0.3692 or 36.92%; one female patient (1/18) 5.55% presented hyperuricaemia, her a posteriori probability being P(A/B)=0.0614 or 6.14%; (7/18) 38.88% women did not present metabolic disorders, therefore the conditional probability was P(A/B)=0.43086 or 43.08%. Finally, the male patients (2/18) 11.11% did not present metabolic disorders (Table 4).
Bayesian analysis in patients with metabolic disorders and primary empty sella.
| Metabolic disorders | A priori probability | A posteriori probability | |
|---|---|---|---|
| P(B/Ai) | P(Ai∩B) | P(Ai/B) | |
| 2 females∩diabetes | 0.8888 | (0.8888) (0.1111)0.0987 | 0.09870.80217=0.12305 |
| 6 females∩dyslipidaemia | 0.8888 | (0.8888) (0.3333)0.2962 | 0.29620.80217=0.3692 |
| 1 female∩hyperuricaemia | 0.8888 | (0.8888) (0.0555)0.0493 | 0.04930.80217=0.06146 |
| 7 females∩no cases | 0.8888 | (0.8888) (0.3888)0.3456 | 0.34560.80217=0.43086 |
| 2 males∩no cases | 0.1111 | (0.1111) (0.1111)0.0123Σ=0.80217 | 0.01230.80217=0.01533Σ=0.9999 |
It can be seen that the a posteriori probability between gender, metabolic disorders with primary empty sella and the greatest probability with respect to an associated disease was found in females diagnosed with dyslipidaemia.
Only in 3 patients (16.66% of the cases) did primary empty sella present as a single disorder, and in 15 cases (83.33%) the primary empty sella presented associated with diverse diseases: cortical, subcortical, cerebellar atrophy, vascular anomalies, anatomical variants, cysts and cerebrospinal fluid dynamics associated with hydrocephalus; it is noteworthy that in 9 patients (50%) vertigo was the characteristic symptom. The 18 patients who comprised the sample underwent audiovestibular assessment, of these 16 (88.88%) patients were diagnosed with an auditory disease of some type; 15 (83.33%) were women and there was one man (5.5%). The type of auditory disease was quantified in these patients thus: 16 (77.77%) presented sensory hearing loss, one (5.5%) conductive and one (5.5%) mixed hearing loss; only 2 patients did not present an auditory disorder.
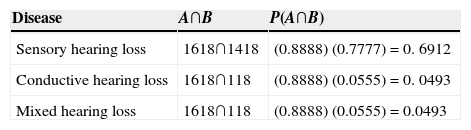
The intersection between the proportions of primary empty sella was calculated, with the presence and type of hearing loss; thus, for sensory hearing loss the proportion was P(A∩B)=0.6912, which means that 69.12% of the patients with primary empty sella presented sensory hearing loss; likewise, the intersection for patients with conductive hearing loss and mixed hearing loss was calculated, where in both cases the value P(A∩B)=0.0493 was obtained, which indicates that 4.93% of the patients with primary empty sella had conductive hearing loss, and sensory hearing loss respectively (Table 5).
Probabilistic intersection between primary empty sella, hearing loss and type of hearing loss.
| Disease | A∩B | P(A∩B) |
|---|---|---|
| Sensory hearing loss | 1618∩1418 | (0.8888) (0.7777)=0. 6912 |
| Conductive hearing loss | 1618∩118 | (0.8888) (0.0555)=0. 0493 |
| Mixed hearing loss | 1618∩118 | (0.8888) (0.0555)=0.0493 |
It can be seen that the probabilistic intersection between primary empty sella, hearing loss and type of hearing loss, and the greatest proportion found was sensory in type in the sample studied.
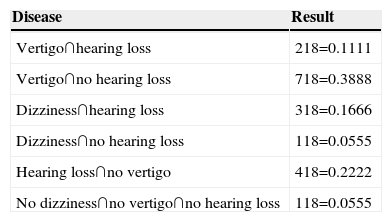
On analysing the joint probability between audiovestibular disorders it was found that 2 (11.11%) patients reported vertigo and hearing loss, 7 (38.88%) patients presented vertigo with no hearing loss, 3 (16.66%) dizziness and hearing loss, one (5.55%) dizziness with no hearing loss, 4 (22.22%), hearing loss with no manifestations of vertigo and one (5.55%) presented no disorder (Table 6).
Joint probability between primary empty sella and audiovestibular disorders.
| Disease | Result |
|---|---|
| Vertigo∩hearing loss | 218=0.1111 |
| Vertigo∩no hearing loss | 718=0.3888 |
| Dizziness∩hearing loss | 318=0.1666 |
| Dizziness∩no hearing loss | 118=0.0555 |
| Hearing loss∩no vertigo | 418=0.2222 |
| No dizziness∩no vertigo∩no hearing loss | 118=0.0555 |
It can be seen that 38.88% of the patients diagnosed with primary empty sella reported vertigo.
It is worth mentioning that 9 (50%) of the patients reported vertigo, 8 (44.44%) were female and one (5.55%) male; 7 (38.88%) patients reported tinnitus, 6 (33.33%) females and one male (5.55%); and finally, dizziness presented in only 6 (33.33%) of the women.
DiscussionPrimary empty sella causes both neurological, endocrine, and audiovestibular signs due to the anatomical location of the pituitary gland, the sellar region and the structures adjacent to this area of the skull. However, because of the precision of current imaging tests combined with clinical data, diagnosis and treatment has improved for patients presenting this disorder.
Based on the nature of pituitary function, several studies have been undertaken to describe endocrine symptoms due to sellar diaphragm herniation over the pituitary gland2,14; it is known that there is an association between the extent of herniation, whether partial or total, and the extent of hypopituitarism.4,20 The imbalance caused by cerebrospinal fluid on the brain structures involved alters their function; the situation of the sellar region and nearby structures, such as the brainstem, from which diverse cranial nerves emerge, can influence how a set of signs present associated with the nuclei and with the apparent origin of the cranial nerves. It is also known that increased intracranial pressure and the pressure exerted by cerebrospinal fluid leads to herniation of the sellar diaphragm.21,22 Saindane et al.23 report that 96% of patients with idiopathic intracranial hypertension or “pseudotumour cerebri” have some degree of incidental empty sella turcica; they mention that the main findings in their patients were: diplopia, papilloedema, headache, dizziness, behavioural changes, dementia, epilepsy, hearing loss, ataxia, tinnitus, weakness, nystagmus and taste and smell disorders.
Some of these findings coincide with this study. Unlike other abovementioned studies the a posteriori conditional probabilities are reported with respect to audiovestibular disease associated with primary empty sella.
It is reported in the literature that the most frequent symptom is headache in patients with primary empty sella; Saindane et al.23 mention that 32.6% of patients report headache, 93.3% of patients who present idiopathic intracranial hypertension plus primary empty sella also report headache; De Marinis et al. report headache in 47.88%4 and Guitelman et al. 35%2; in our results we report that 14.81% of the women presented headache together with primary empty sella according to the joint probability analysis.
Likewise, the joint probability in relation to excess weight in females and primary empty sella was 64.16%.
Other authors, such as De Marinis et al.,4 report that 73% of patients with primary empty sella are overweight, Guitelman2 reports 67.6% and Guinto et al.12 mention that 13 out of 19 women with excess weight present primary empty sella. In Maira et al.’s study21 52% presented obesity. With this association the percentages were always greater than 50%, which indicates that excess weight is a factor present in more than half of patients with primary empty sella. With regard to metabolic disorders, it was found that dyslipidaemia was present in 36.92% of the female patients with primary empty sella, whereas this was 18.75% in Rani et al. study.14 With reference to audiovestibular symptoms, there are few studies which report patients with primary empty sella and audiological and vestibular assessment; however, it is probable that intracranial hypertension, fluctuations in cerebrospinal fluid, the anatomical disposition of the sellar region, neurovascular architecture, and metabolic disorders influence the presentation of symptoms, such as hearing loss, vertigo, tinnitus and dizziness. Fourteen (77%) cases of patients with primary empty sella are reported in this study, who were diagnosed with sensorineural hearing loss, which suggests a high rate of presentation of hearing loss in these patients. Therefore it is important that patients reporting vertigo, dizziness, tinnitus or any form of hearing loss should have a differential diagnosis in order to rule out primary empty sella.
ConclusionsThe use of Bayesian analysis to assess conditional probability, based on a priori and a posteriori values, is a statistical tool which can help to understand the dependence between 2 or more variables. These mathematical models were used in this study to analyse the possible association of comorbidities and audiovestibular diseases in patients diagnosed with primary empty sella; in the sample studied the greatest incidence of comorbidities were found in females. It is apparent that primary empty sella can be highly associated with audiovestibular diseases. On the basis that the proportion found was 0.09 (18/20), with respect to patients reporting audiovestibular problems, these types of study should be continued increasing the population size, in order to determine categorically the dependence between the different audiovestibular diseases and primary empty sella.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Delgado-Hernández A, Verduzco-Mendoza A, Luna-Reyes FA, Márquez-Palacios S, Arch-Tirado E. Análisis de la probabilidad conjunta y a posteriori entre aracnoidocele selar primario, sus comorbilidades y enfermedad audiovestibular. Cirugía y Cirujanos. 2015;83:459–466.