The most common cause of anal sphincter injuries in women is vaginal birth. Endo-anal ultrasound is currently used for the diagnosis of anal sphincter defect. However, due to the inconvenience caused, it is not an applicable technique during the immediate postpartum.
The aim of this study was to determine whether transperineal ultrasound in 3/4D is a useful diagnostic method for the assessment of anal sphincter during the immediate postpartum.
Material and methodsA prospective study was conducted on the vaginal deliveries performed between September 2012 and June 2013 in the Valme University Hospital (Seville). Obstetric and foetal parameters that could influence the onset of perineal tears were studied. The patients underwent a transperineal 3/4D ultrasound and a multislice study (48h after birth).
ResultsThe study included 146 puerperal women. The sphincter complex was assessed in all of them during the immediate postpartum. External anal injuries were observed in 10.3% of the cases. In 8.2% of cases, the primary suture of the external anal sphincter was detected during ultrasound examination, and 2.1% of asymptomatic lesions were diagnosed only with postpartum ultrasound. None of the patients reported discomfort or pain.
ConclusionsThe 3-dimensional transperineal ultrasound is helpful in determining the primary repair of the anal sphincter during the immediate postpartum, with no discomfort for patients, as well as for establishing those early sphincter injuries that go unnoticed during vaginal delivery.
La causa más frecuente de lesiones del esfínter anal en mujeres es el parto vaginal. Actualmente el diagnóstico del defecto del esfínter anal es la ecografía endoanal. Sin embargo, debido a las molestias que ocasiona, no es una técnica aplicable durante el posparto inmediato.
El objetivo que nos planteamos es establecer si la ecografía transperineal en 3/4D es un método de diagnóstico útil para la valoración del esfínter anal durante el posparto inmediato.
Material y métodosSe realizó un estudio prospectivo de los partos vaginales atendidos entre septiembre del 2012 y junio del 2013, en el Hospital Universitario de Valme (Sevilla). Se estudiaron parámetros obstétricos y fetales que pudiesen influir en la aparición de desgarros perineales. A las pacientes se les realizó una ecografía transperineal en 3/4D y estudio multicortes ecográfico (48 h tras el parto).
ResultadosSe analizó a 146 puérperas y en todas se valoró el complejo esfinteriano durante el posparto inmediato. El 10.3% presentaron lesiones del esfínter anal externo. En el 8.2% de los casos se detectó la sutura primaria del esfínter anal externo durante la exploración ecográfica y en el 2.1% de las pacientes se observaron lesiones asintomáticas diagnosticadas solamente con la ecografía posparto. Ninguna de las pacientes refirió molestias ni dolor.
ConclusionesLa ecografía transperineal 3D es útil para determinar la reparación primaria del esfínter anal durante el posparto inmediato sin molestias para las pacientes, además de establecer precozmente aquellas lesiones esfinterianas que pasan desapercibidas durante el parto vaginal.
The most common cause of anal sphincter lesions in women is vaginal birth.1 This has a major affect on the quality of life of these patients, as approximately one-third of them develop anal incontinence in spite of repair of the lesion following birth.2 The majority of symptomatic patients have mild incontinence,3,4 so that many of them do not consult their doctor about it.
The diagnosis of external and internal anal sphincter defect is currently by means of endoanal ultrasound scan. This is due to the good sensitivity and specificity of this test.5 Nevertheless, this technique cannot be used to evaluate anal sphincter suture during the immediate postpartum period because of its intrinsic discomfort and the need for staff who know the technique and how to use it. This is why some authors recommend reserving it solely for research purposes.6 We therefore have the aim of establishing whether 3/4D transperineal ultrasound scan is a useful diagnostic tool during the immediate postpartum period, to evaluate the anal sphincter and its repair after giving birth.
Material and methodsA prospective study was carried out from 1 September 2012 to 30 June 2013, in patients admitted to the Maternity Unit of Valme Hospital Universitario (Seville). This included those patients with the gestation of a single foetus to term, with no history of previous pregnancy or previous surgical operations to correct pelvic floor disease, in the active phase of the birth, with the foetus in head presentation, and having given their written acceptance of the informed consent. Pregnancies with severe disease of the mother or foetus were excluded.
Births were attended by the staff of the Maternity Unit, with at least 3 years’ experience in obstetric practice.
The following obstetric parameters were studied: gestational age, induction of birth, epidural anaesthesia, instrumentation, duration of the second phase of the birth, episiotomy and perineal tears. The foetal parameters quantified after birth are head perimeter and foetal weight.
For ultrasound evaluation a Toshiba Aplio 500® (Toshiba Medical Systems Corp., Tokyo, Japan) ultrasound scanner was used, with a PVT-675MV 3D abdominal probe. The probe was enclosed in a powder-free cover for reasons of hygiene.7
The postpartum ultrasound scan was performed by the same examiner who was specifically trained in transperineal 3/4D ultrasound scanning. The images were recorded within the first 48h postpartum; they were acquired when the patients were lying in dorsal lithotomy on a gynaecological examination table with an empty bladder and rectum.8,9 The transducer was placed on the perineum carefully, with as little pressure as possible, with the main axis of the transducer placed in the introitus in the central saggital plane.
Study of the echographic volume of the anal sphincter permits access to the axial plane. This analysis used what is known as the plane of minimum dimensions described in previous studies.9–13 Slices were taken at intervals of 2.5mm after the plane of minimum dimensions, studying 3 slices under this plane and 4 slices above it, obtaining a total of 8 slices equivalent to a thickness of 12.5mm. The anal sphincter was evaluated in 6 central slices, and the existence was determined of undiagnosed lesions which had been produced during birth, or sutures made in the context of a major tear.
The descriptive statistical analysis of the quantitative variables is summarised in the form of averages and typical deviations or, in the case of asymmetrical distributions, with medians and percentiles (P25 and P75) while qualitative variables are shown as percentages. The statistical analysis was performed using version 15 of the SPSS program (SPSS, Chicago, IL, USA).
Results166 expectant mothers with no previous vaginal birth were evaluated during birth. 16 cases were considered to have been lost: 10 patients terminated pregnancy with an intrapartum cesarian section (4 due to the suspicion of foetal discomfort and 6 due to lack of progression), while ultrasound study was not performed in 5 patients due to a fault in follow-up by the researcher (one case was ruled out because of defects in image capture and 4 cases were excluded as following processing of the axial image not all of the structures within the sphincter complex were identifiable due to intense perineal oedema).
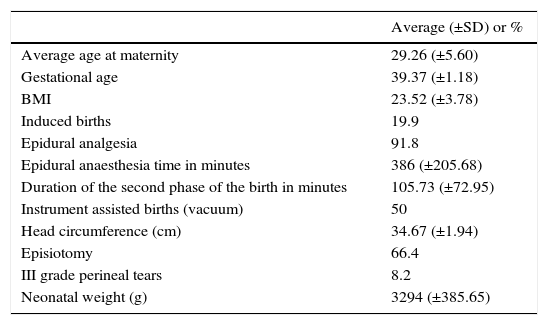
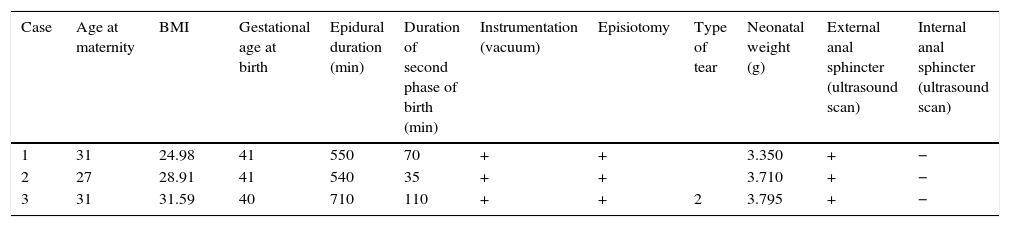
Table 1 shows the general and intrapartum obstetric characteristics of the population that was finally studied.
General obstetric and intrapartum characteristics of the 146 patients studied.
| Average (±SD) or % | |
|---|---|
| Average age at maternity | 29.26 (±5.60) |
| Gestational age | 39.37 (±1.18) |
| BMI | 23.52 (±3.78) |
| Induced births | 19.9 |
| Epidural analgesia | 91.8 |
| Epidural anaesthesia time in minutes | 386 (±205.68) |
| Duration of the second phase of the birth in minutes | 105.73 (±72.95) |
| Instrument assisted births (vacuum) | 50 |
| Head circumference (cm) | 34.67 (±1.94) |
| Episiotomy | 66.4 |
| III grade perineal tears | 8.2 |
| Neonatal weight (g) | 3294 (±385.65) |
BMI: body mass index.
Lesions occurred to the external anal sphincter in 10.3% (15 cases) of the births. In 8.2% (12 patients) of the cases a primary suture of the external anal sphincter was detected during the ultrasound scan, and in 2.1% of these (3 cases) they were not diagnosed during birth but were detected in the subsequent ultrasound scan.
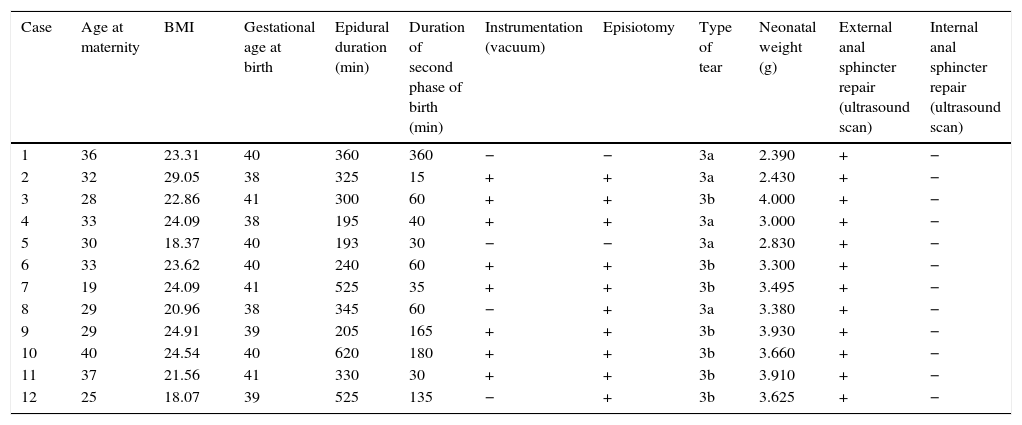
Table 2 shows the data corresponding to the 12 patients who were diagnosed with perineal tears in the anal sphincter during birth. All of the tears were of the 3a or 3b types, according to the classification established by the Royal College of Obstetricians and Gyneacologists.14 Type 3a tears in the external anal sphincter were repaired by end to end technique, while those of type 3b were sutured using the overlap technique. After the surgical repair of these high-grade tears a check was performed to ensure that they had been made correctly by means of bi-digital palpation of the suture, inserting the index finger into the anal channel and the thumb into the vaginal region. This check of the primary repair of the sphincter was performed by 2 independent examiners, and suture of the tear did not continue until both gynaecologists agreed that the external anal sphincter had been correctly repaired. A total of 4 of the cases which had presented high-grade tears were assisted births, and of these only 2 patients had not received episiotomy. The lesions of these 2 patients were of the 3a type, justified by precipitated expulsion that did not permit perineal protection during birth.
Patients diagnosed with high grade tear during birth.
| Case | Age at maternity | BMI | Gestational age at birth | Epidural duration (min) | Duration of second phase of birth (min) | Instrumentation (vacuum) | Episiotomy | Type of tear | Neonatal weight (g) | External anal sphincter repair (ultrasound scan) | Internal anal sphincter repair (ultrasound scan) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 36 | 23.31 | 40 | 360 | 360 | − | − | 3a | 2.390 | + | − |
| 2 | 32 | 29.05 | 38 | 325 | 15 | + | + | 3a | 2.430 | + | − |
| 3 | 28 | 22.86 | 41 | 300 | 60 | + | + | 3b | 4.000 | + | − |
| 4 | 33 | 24.09 | 38 | 195 | 40 | + | + | 3a | 3.000 | + | − |
| 5 | 30 | 18.37 | 40 | 193 | 30 | − | − | 3a | 2.830 | + | − |
| 6 | 33 | 23.62 | 40 | 240 | 60 | + | + | 3b | 3.300 | + | − |
| 7 | 19 | 24.09 | 41 | 525 | 35 | + | + | 3b | 3.495 | + | − |
| 8 | 29 | 20.96 | 38 | 345 | 60 | − | + | 3a | 3.380 | + | − |
| 9 | 29 | 24.91 | 39 | 205 | 165 | + | + | 3b | 3.930 | + | − |
| 10 | 40 | 24.54 | 40 | 620 | 180 | + | + | 3b | 3.660 | + | − |
| 11 | 37 | 21.56 | 41 | 330 | 30 | + | + | 3b | 3.910 | + | − |
| 12 | 25 | 18.07 | 39 | 525 | 135 | − | + | 3b | 3.625 | + | − |
BMI: body mass index.
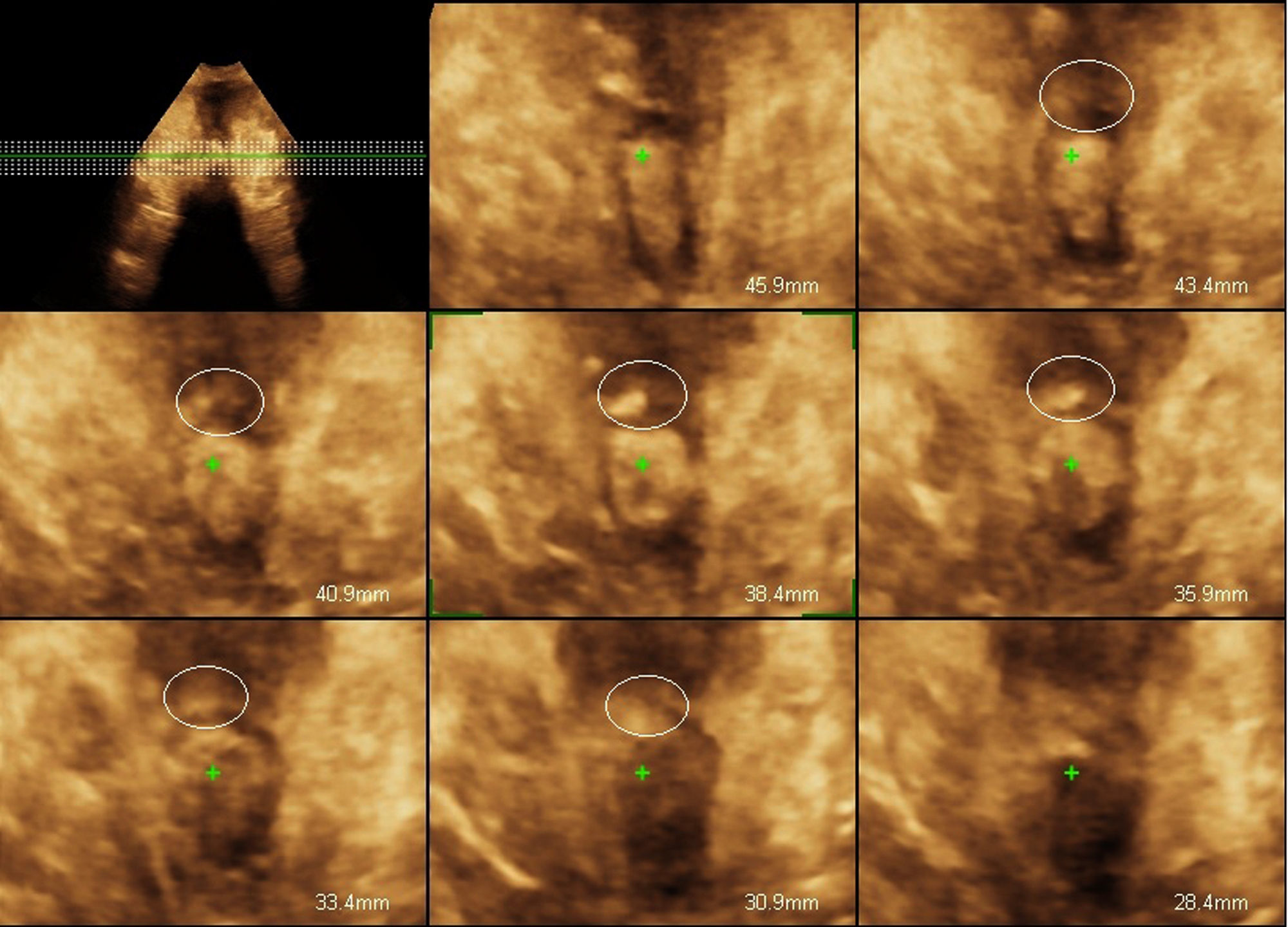
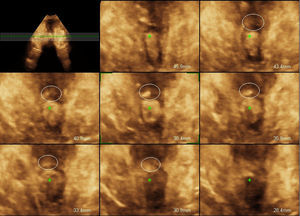
The ultrasound scan diagnosis of the primary suture of the anal sphincter was based on detecting a thickening of the external anal sphincter with a more hyperechoic appearance than the rest of the sphincter ring, as may be seen in Fig. 1. This ultrasound examination was performed by an external gynaecologist who had no connection with the birth and was unaware of the existence of a tear in each patient.
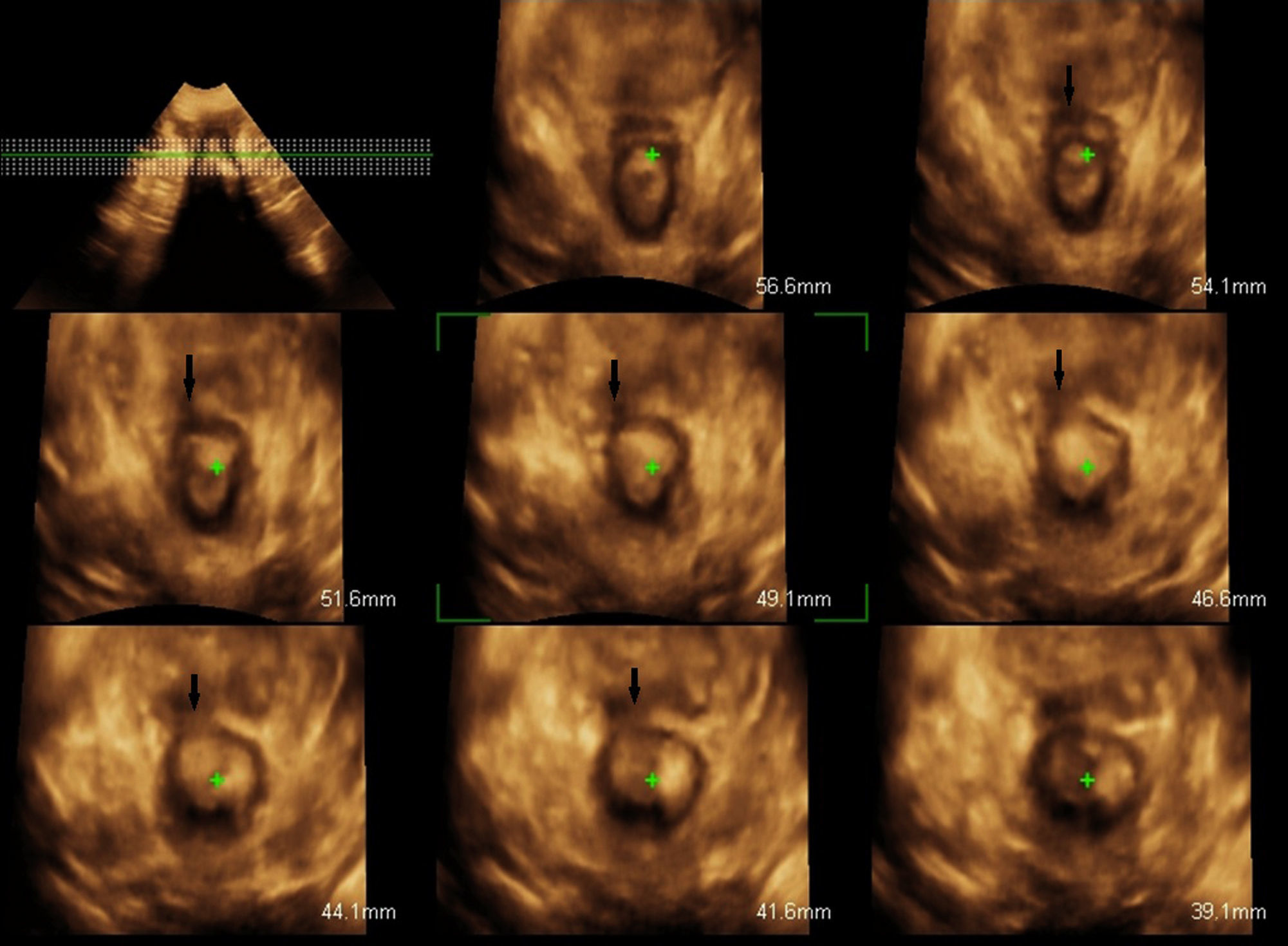
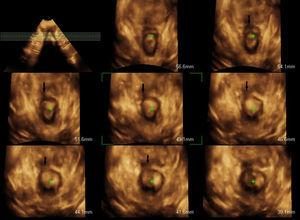
The obstetric data of the patients in whom high-grade tears had not been detected during birth and who presented lesions during the ultrasound scan are shown in Table 3. Although after birth all an examination of the anal sphincter of the women had been exhaustively performed in 2 examinations prior to the perianal suture, in 3 patients the lesions were diagnosed by ultrasound scan. These 3 cases were instrument-assisted births in which an episiotomy had been performed. The lesions were detected after 12h and showed as a loss of external anal sphincter continuity, with retraction of the remaining muscle ends, while the internal anal sphincter remained intact, as may be seen in Fig. 2. The lesions in these 3 patients were confirmed by transperineal 3/4D ultrasound scan 6 months after the birth. In this check-up all 3 women were asymptomatic.
Patients with high grade tears that were not detected during birth that presented lesions during ultrasound scan.
| Case | Age at maternity | BMI | Gestational age at birth | Epidural duration (min) | Duration of second phase of birth (min) | Instrumentation (vacuum) | Episiotomy | Type of tear | Neonatal weight (g) | External anal sphincter (ultrasound scan) | Internal anal sphincter (ultrasound scan) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 31 | 24.98 | 41 | 550 | 70 | + | + | 3.350 | + | − | |
| 2 | 27 | 28.91 | 41 | 540 | 35 | + | + | 3.710 | + | − | |
| 3 | 31 | 31.59 | 40 | 710 | 110 | + | + | 2 | 3.795 | + | − |
BMI: body mass index.
During the ultrasound scan none of the patients mentioned discomfort or pain, in spite of the fact that the evaluation took place within 48h after giving birth, while many of them had perineal sutures. Following the examination all of the patients stated that before the ultrasound scan they had thought that the scan would cause pain in the perineal region, but that this had not occurred.
None of the women studied presented clinical data showing anal incontinence during the postpartum period.
DiscussionObstetric sphincter tears are the most frequent cause of anal incontinence in healthy women.6,15,16 A direct relationship has been found to exist between the degree of the sphincter defect after repair and the degree of anal incontinence.17 It is therefore important that the coloproctological surgeon diagnose these defects as soon as possible, to commence the appropriate treatment as early as is feasible.
Different approaches have been described for the evaluation of the anal sphincter by ultrasound scan, including endoanal, transvaginal and transperineal approaches.18 Classically endoanal ultrasound scan is now the main test for the diagnosis of these lesions, due to its good sensitivity and specificity.19 However, it is not a useful technique for evaluating the primary sutures of the sphincter during the immediate postpartum period because of the discomfort it may cause to patients. We also have to take into account the difficulty of accessing specialised personnel who are able to perform an examination of this type during the immediate postpartum period.6 Some authors therefore advise that postpartum endoanal ultrasound scan should be reserved solely for research purposes.6
With the aim of finding an imaging technique that is easier to perform, accessible and non-invasive, the role of transperineal ultrasound scan was studied in the diagnosis of internal and external lesions of the anal sphincter.18 Previous studies have described that the location and extension of the anal sphincter lesions diagnosed using 3/4D transperineal ultrasound scan were compatible with those obtained using magnetic resonance imaging.20
Evaluation of sphincters by transperineal ultrasound scan has been described with the use of different ultrasound probes. Different authors have established the usefulness of endovaginal probes for this type of examination.18,21–23 Peschers et al.,24 as is the case in our work, used convex transducers, and they described all of the layers in the anal sphincter complex, in the same way as had been established using endoanal ultrasound scan.
Transperineal ultrasound scan has not only been able to describe the anatomical structures of the anal sphincter, as it has also made it possible to identify traumatic obstetric lesions in the sphincter complex,21 as we observed in our study.
In the case of patients with anal sphincter lesions it is important that they be given an ultrasound scan following the repair of the sphincter after the birth. They should also receive periodical check-ups to evaluate the healing process and to detect possible symptoms of incontinence.25 Nevertheless, ultrasound is not only useful in the evaluation of the scarring process, as it is also useful in the diagnosis and follow-up of hidden lesions of the anal sphincter that were not diagnosed during the birth.6 These hidden lesions have been described in 7.9% of vaginal births.21 These types of hidden trauma were also detected in our study, with a frequency of 2.1%, which is lower than the figure established in previous studies.21
However, the incipient diagnosis at such an early stage which we performed in this work may be restricted by oedema, haemorrhaging and lacerations in the genital area.26 To attempt to reduce these erroneous diagnoses it was decided to undertake a single axial plane tomographic ultrasound study. This established the diagnosis of sphincter lesion if the said trauma was present in the 5 central slices of the multislice mode.
Sphincter lesions that go unnoticed during birth and are identified during the subsequent ultrasound scan are the cause of some cases of postpartum anal incontinence.27 Asymptomatic sphincter defects have been detected in patients with reduced sphincter thickness at the 12 o’clock position and with an intact perineal body.28 This is due to the fact that the body of the perineum stabilised the remaining muscle fibres of the external sphincter.28
The chief objective following a complete ultrasound examination must be to advise women after they have suffered anal sphincter obstetric trauma.25
To conclude, we can say that 3D transperineal ultrasound scan is useful for determining the primary repair of the anal sphincter during the immediate postpartum period. It causes the patients no discomfort and also offers early indication of those sphincter lesions that went unnoticed during vaginal birth.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors declare that they received no financing of any type and that they have no conflict of interests to declare.
Please cite this article as: García-Mejido JA, Palomino LG, Palacín AF, Sainz-Bueno JA. Aplicabilidad de la ecografía transperineal en 3/4D para el diagnóstico de lesiones del esfínter anal durante el posparto inmediato. Cir Cir. 2017;85:80–86.