Single incision laparoscopic surgery has increased recently due to successful results, achieved in several procedures. The aim of the present work is to present the first case in which single incision laparoscopy is used for the drainage of an amoebic liver abscess.
Clinical caseA 44-year-old man presented with intense right upper quadrant pain, generalised jaundice, tachycardia, fever, hepatomegaly and a positive Murphy's sign. Laboratory results revealed an increased plasma bilirubin, elevated alkaline phosphatase and transaminases, leucocytosis, negative viral panel for hepatitis, and positive antibodies against Entamoeba histolytica. On an abdominal computed tomography a 15cm×12.1cm hypodense lesion was observed in the patient's liver, identified as an amoebic liver abscess. Analgesics and antibiotics were started and subsequently the patient was submitted to laparoscopic drainage of the abscess using a single port approach. Drainage and irrigation of the abscess was performed. Four days later the patient was discharged without complications.
ConclusionManagement of amoebic liver abscess is focused on the elimination of the infectious agent and obliteration of the abscess cavity in order to prevent its complications, especially rupture. Laparoscopic surgery has proved to be a safe and effective way to manage this entity.
El uso del puerto único ha adquirido impulso, debido a los resultados exitosos logrados recientemente en diversas disciplinas. El objetivo del presente trabajo es reportar el primer caso de la laparoscopia por puerto único, para el drenaje de un absceso hepático amebiano.
Caso clínicoHombre de 44 años con dolor abdominal intenso en hipocondrio derecho, ictericia generalizada, taquicardia y fiebre; se palpa borde hepático a 5cm por debajo del reborde costal, signo de Murphy positivo. Los estudios de laboratorio revelaron: hiperbilirrubinemia directa, elevación de fosfatasa alcalina y transaminasas, leucocitosis a expensas de neutrófilos, panel viral negativo para hepatitis, y anticuerpos positivos para Entamoeba histolytica. La tomografía computada abdominal mostró una lesión hipodensa de 15 por 12.1cm en lóbulo hepático derecho. Se inició tratamiento con analgésicos, y doble esquema antibiótico. El paciente fue sometido a drenaje del absceso hepático por la vía laparoscópica a través de puerto único, aspirando 1200 cc de contenido de aspecto achocolatado, se realizó lavado de cavidad. Al cuarto día de internamiento el paciente fue dado de alta sin complicaciones.
ConclusiónEl tratamiento del absceso hepático amebiano va dirigido hacia la erradicación del agente infeccioso y de la cavidad abscedada, ya que se trata de una entidad clínica que puede tener complicaciones severas, especialmente la ruptura. La laparoscopia por puerto único ha demostrado ser una alternativa segura y efectiva, en el tratamiento de los pacientes que requieren drenaje de abscesos amebianos.
Liver amoebiasis is the commonest extraintestinal manifestation of the infection by Entamoeba histolytic (E. histolytic), complicating the course of the disease in 3–10% of the subjects infected by this micro-organism.1 It normally presents between the fifth and sixth decade of life,2,3 with an equivalent distribution in men and women; 75% of the cases locates in the right hepatic lobe, they are characterised as unique and being surrounded by a thin cover of granulation tissue.4
This entity is found mainly in developing countries with tropical and subtropical weather. In Mexico, intestinal amoebiasis and its complications present an incidence of 384.15/100,000 inhabitants, being considered an area where the disease is endemic.5,6
Amoebicidal drugs are the first line of treatment in the management ofamoebic hepatic abscesses, metronidazole being the first line medication at national and international level due to its effectiveness and accessibility. Up to 90% of the cases are solved solely with pharmacological treatment. It is necessary to resort to invasive therapeutic measures in the remaining 10% which do not respond to treatment. This includes interventional radiology procedures and conventional or minimally invasive surgical procedures.7,8
Percutaneous drainage is considered the first invasive choice; however, there are conditions in which this procedure fails, in particular due to the density of the abscess content or technical or logistical difficulties in its performance; surgical drainage is indicated in these patients. Generally, the surgical treatment of these patients is performed through open procedures, and it has recently been demonstrated that the laparoscopic treatment of liver abscesses is safe and effective, with long-term favourable results.7,9
Advances in laparoscopic surgery have led to the development of new approaches that seek to be even less invasive, with similar postoperative results and higher aesthetic results compared to those of conventional laparoscopy. Single port laparoscopy or single incision laparoscopic surgery are among these techniques and have been growing in favour due to the results obtained in procedures such as cholecystectomy, adrenalectomy and colon resection.10–12
The aim of the present work is to present the first case in which single incision laparoscopy is used for the drainage of an amoebic liver abscess.
Clinical caseA 44-year-old man presented in the emergency department with a 9-day evolution history of abdominal pain located in the right hypochondrium, which increased in intensity until becoming intolerable, of oppressive and continuous nature, irradiated in girdling pain towards the back and subsided intermittently with the use of non-steroidal analgesics. The pain was accompanied by the appearance of one-week evolution generalised jaundice and unquantified fever the day before his admission.
He does not report relevant family history; the patient's medical history only reveals occasional consumption of alcoholic beverages, especially beer and pulque during youth.
During physical examination, he had tachycardia and a 39°C fever, generalised jaundice in skin and scleras, soft and depressible abdomen with intense pain on palpation over the right hypochondrium, palpable liver edge at 5cm under the costal margin and positive Murphy's sign.
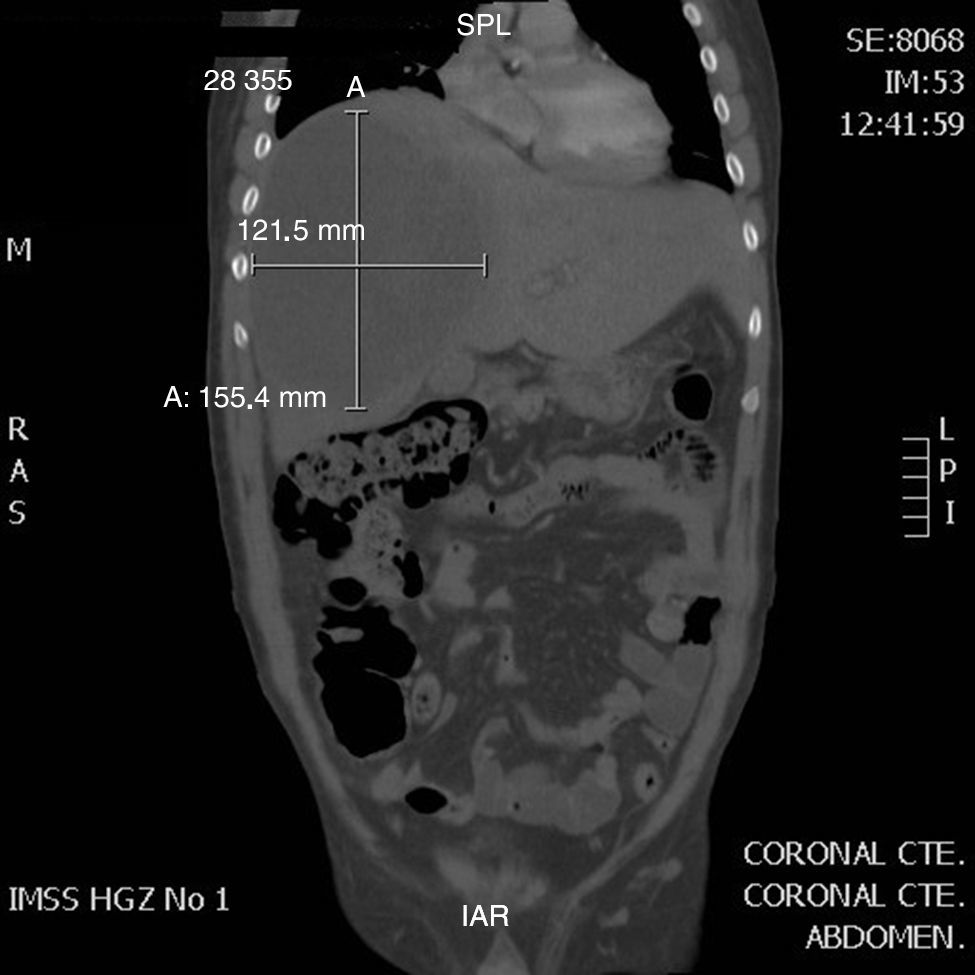
The initial laboratory studies showed hyperbilirubinaemia at the expense of direct bilirubin, with increase of alkaline phosphatase and transaminases, leukocytosis with neutrophilia, negative viral panel for hepatitis B and C and positive IgG antibodies for E. histolytic. A hepatic ultrasound was performed that revealed a well-defined hypoechoic lesion in segments V and VIII. The abdominal computed tomography showed a well-defined homogeneous hypodense lesion in the right hepatic lobe of 15.5cm×12.1cm (Fig. 1).
The patient was hospitalised and treated with analgesics and double antibiotic regime with metronidazole and ceftriaxone.
Because of the lack of an interventional radiology programme in our institution and the characteristics of the abscess regarding its volume, being unilocular and locating in the anterior region, it was considered that the patient was an ideal candidate for the laparoscopic procedure using a single port approach. This procedure was decided with the patient, who accepted and signed the informed consent form.
Surgical techniqueA 3-cm vertical transumbilical incision was performed with plane dissection until entering the peritoneal cavity, when the multiple access port (Single Incision Laparoscopic Surgery, SILS Port, Covidien) was inserted under direct vision and a pneumoperitoneum was created at 15mmHg (Fig. 2). A 5mm laparoscope and a zero-degree lens, aspirator/irrigator and a SILS clinch were introduced. When assessing the cavity, a mass over the lower hepatic face was found which, when dissected, let brown chocolate-aspect material coming from the liver flow, revealing the presence of a restrained broken liver abscess. A total of 1.200cc of the abscess content was aspirated and samples were taken for culture. Later, irrigation with 4.000cc warm sterile saline solution was carried out until obtaining a clear aspiration. It was found that this was a single abscess with walls covered by fibrinopurulent material when assessing the abscess walls. A Saratoga drain was placed in the abscess bed, which was externalised at subcostal level and anterior axillary line.
The patient started a diet and walking the next day; he was given an abdominal computed tomography for control the third postoperative day, in which obliteration of the abscess space was found. The patient was asymptomatic and afebrile the fourth day of hospitalisation; therefore, he was discharged. The drainage was removed 2 weeks later and the patient was continuing asymptomatic at 6 months of follow-up.
DiscussionAmoebic liver abscesses are a potentially serious clinical condition due to the high morbidity and mortality of its complications. Patients tend to present with a history of fever, generalised discomfort, abdominal distension, hepatomegaly and abdominal pain in the right hypochondrium. They are usually located in the right hepatic lobe and are generally single.6 The diagnosis of this disease is predominantly clinical. It can be based on image procedures, particularly hepatic ultrasound and computed tomography.13
Once the amoebic liver abscess has been identified, it is necessary to eliminate the infectious agent and obliterate the abscess cavity. In this group of patients, treatment must start immediately because this disease may have serious complications, especially rupture towards the peritoneum, pleurae, pericardium or through the skin.
Metronidazol is within the group of medications for the amibiasis treatment, which is the first choice drug to remove the Entamoeba; due to 10–20% of the amoebic abscesses showing bacterial infection, especially gram-negative bacilli, it is recommended that an antibiotic be administered.4
Despite the proven usefulness of pharmacological management, there are cases in which this will not be enough and will require invasive manoeuvres for the removal of the abscess. Today percutaneous drainage preceded by radiology is the basis of invasive management, with success rates near 85%.9
The surgical management of patients with liver abscesses is usually reserved for patients whom medical and percutaneous treatment failed, when there are large, multilocular or dense content abscesses, imminence of rupture or development of serious complications such as peritonitis.7 The contraindication for the percutaneous management or the lack of infrastructure to perform it can also be considered indications for surgical management.14
Traditionally, drainage of liver abscesses was performed through open surgeries; however, laparoscopic surgery has been demonstrated to be a safe and effective choice for the management of this group of patients.9 Among the many advantages it offers are surgical trauma minimisation, reduction of hospital stay and postoperative pain, as well as obtaining more aesthetic scars.15
Among the technologies for minimally invasive surgery, single port laparoscopy is the most promising in the last decade. Its current indications are limited to the commonest surgeries, such as cholecystectomies16,17 and appendectomies.18,19 However, recent medical literature has gradually demonstrated its usefulness in interventions on other organs such as adrenal glands, colon and kidney.12,20,21
Various studies have demonstrated that single-port laparoscopy is technically as feasible and safe as conventional laparoscopy. Its main advantage is the aesthetic aspect by using the umbilical scar for the instrumental insertion and avoiding more scars. Some authors also report a decrease in postoperative pain and less time needed off work.22–24 However, further studies are required in this field.
Although it has been argued that technically single-incision laparoscopic surgery is more demanding than conventional laparoscopy, Mutter et al. have demonstrated that programmes focused on this surgical approach can safely be started in teaching hospitals that have experienced surgeons in laparoscopy, since the learning curve starts near the plateau.25
ConclusionThe present case shows that the drainage of the liver abscesses through single-port laparoscopy is technically feasible and safe. In the future, it may turn into an option within the set of surgical approaches available for this disease despite the technical and economic limits that still exist today on its large-scale implementation.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Telich-Tarriba JE, Parrao-Alcántara IJ, Montes-Hernández JM, Vega-Pérez J. Drenaje de absceso hepático amebiano por laparoscopia de puerto único. Reporte de un caso. Cir Cir. 2015;83:329–333.