Trauma Evaluation and Management course was designed to develop trauma cognitive skills in senior medical students. Its effectiveness has been demonstrated in many regions, except in Latin America, where it has been poorly studied. The objective was to determine the Trauma Evaluation and Management course effectiveness, and whether greater effectiveness is achieved in basic- or clinic-cycle students, as well as student perception.
Material and methodsDescriptive, observational, longitudinal and prospective study. Two tests were performed, pre- and post-course; the manual was read by the students prior to both tests. Students were divided into 2 groups: group A (consisting of 71 basic-cycle medical students) and group B (consisting of 44 clinical-cycle medical students).
ResultsGroup A achieved a 2.45 increase (p<0.01) in the post-course evaluation compared with pre-course test. Group B increased the mean score by 2.25 (p>0.05) from pre- to post-course tests. There was a significant difference between groups in both evaluations (pre-course test p<0.01 and post-course test p>0.05), with no difference in improvement (p>0.05). Using a questionnaire, 92.17% of the students totally agreed that the course improved their trauma knowledge, 76.52% that it increased their trauma clinical skills, with 94.78% being totally satisfied with the course, and 86.09% totally agreed that Trauma Evaluation and Management course should be in Medicine curriculum.
ConclusionsTrauma Evaluation and Management course improves trauma cognitive skills, and undergraduate medical students in Mexico broadly accept it.
El curso Evaluación y Manejo del Trauma fue diseñado para desarrollar las habilidades cognitivas en trauma por los estudiantes de Medicina. Su efectividad ha sido demostrada en muchas regiones excepto a nivel de Latinoamérica, donde ha sido poco estudiado.
El objetivo fue conocer la efectividad del curso Evaluación y Manejo del Trauma, cuándo alcanza mayor efectividad en ciclos básicos o clínicos, y la percepción de los alumnos sobre el curso.
Material y métodosEstudio descriptivo, observacional, longitudinal y prospectivo. Dos evaluaciones fueron realizadas: pre- y poscurso. Los estudiantes se dividieron en 2 grupos: el grupo A (71 estudiantes de Medicina de ciclos básicos) y el grupo B (44 estudiantes de Medicina de ciclos clínicos).
ResultadosEl grupo A logró un aumento de 2.45 puntos (p<0.01) en la evaluación poscurso comparada con la evaluación precurso. El grupo B aumentó en promedio 2.25 puntos de la evaluación poscurso (p>0.05). Hubo una diferencia significativa entre los grupos en ambas evaluaciones (precurso p≤0.01 y poscurso p<0.05); sin diferencia en el aprovechamiento (p>0.05). Mediante encuesta, el 92.17% de los estudiantes se mostró totalmente de acuerdo en que el curso mejoró su conocimiento en trauma, el 76.52% que incrementó sus habilidades clínicas en trauma, el 94.78% quedó totalmente satisfecho con el curso y el 86.09% estuvo totalmente de acuerdo en que el curso Evaluación y Manejo del Trauma debe ser incorporado al currículo de la carrera de Medicina.
ConclusionesEl curso Evaluación y Manejo del Trauma mejora las habilidades cognitivas en trauma y es bien aceptado por los estudiantes de pregrado en México.
Assault was the seventh cause of death in Mexico in 2010, with 25,757 deaths, while accidents were the fourth, 16,552 of deaths being the result of traffic accidents involving motor vehicles.1 Training in trauma care is an essential part of medical education, due to its impact on mortality. In Mexico, undergraduate medical students’ knowledge of trauma before their internships has been researched, and their shortcomings in this regard demonstrated.2 This highlights the need to research the methods for gaining trauma knowledge.
The areas of Orthopaedics and Traumatology are covered in the Physician and Surgeon degree course in the Faculty of Medicine of Mexico's Universidad Nacional Autónoma, in the ninth semester of the course.3 However, no internationally accredited course is offered, such as the Advance Trauma Life Support course or the Trauma Evaluation and Management [TEAM] course; the latter was designed by the American College of Surgeons for medical students in order to make students aware of the basic principles of polytrauma patient care4; it consists of a 4–6-hour course, which is essentially theoretical, as a first approach to trauma care for medical students.
The Trauma Evaluation and Management course has been included in the curricula of many medical colleges around the world, its effectiveness and student perception of it, with an improvement in their cognitive and clinical skills have been confirmed.5–8 The best time to implement the course has also been studied9; however, it has only been compared in clinical cycles. There is also a version of the Trauma Evaluation and Management course, known as the expanded Trauma Evaluation and Management course, which has the same objectives and content but it includes added practice in different scenarios, the course content is thus practical as well as theoretical.10
The objectives of this study were to discover the differences in medical students’ cognitive trauma skills before and after they had taken the Trauma Evaluation and Management course, to find out whether or not there are differences in how basic-cycle and clinical-cycle medical students benefit from the course, and to find out the students’ perception and satisfaction with the course.
Material and methodsAn analytical, longitudinal and prospective study was undertaken to achieve the above mentioned objectives. Undergraduate students of the Faculty of Medicine of Mexico's Universidad Nacional Autónoma were included, who had been randomly selected, and those who did not complete the 2 assessments (pre- and post-course) were excluded. In the end, the students formed 2 groups: group A included 71 basic-cycle students (34 first-year and 37 second-year students from a 5.5 year course), and group B, comprising 44 clinical-cycle students (18 third-year and 24 fourth-year students). The sample size enabled a 90% confidence interval. The selection criteria were that they should be Physician and Surgeon degree students of the Faculty of Medicine of Mexico's Universidad Nacional Autónoma who had not undertaken the course previously.
Fifteen days before the course the students were given the Trauma Evaluation and Management manual to study. The manual was as approved by the Mexican chapter of the American College of Surgeons. Before they started the course they were given a questionnaire of 20 multiple-choice questions in order to evaluate the subjects covered in the Trauma Evaluation and Management course, according to their objectives. This evaluation consisted of responses to questionnaires from previous versions of the Trauma Evaluation and Management course. The students then undertook the course and when they had completed it they were given the final questionnaire to evaluate the course itself (20 multiple-choice questions); this was different to the initial evaluation questionnaire, and a survey of 5 questions on student satisfaction was also taken. The questionnaires were given a numerical scale from 0 to 10 as the minimum and maximum score respectively.
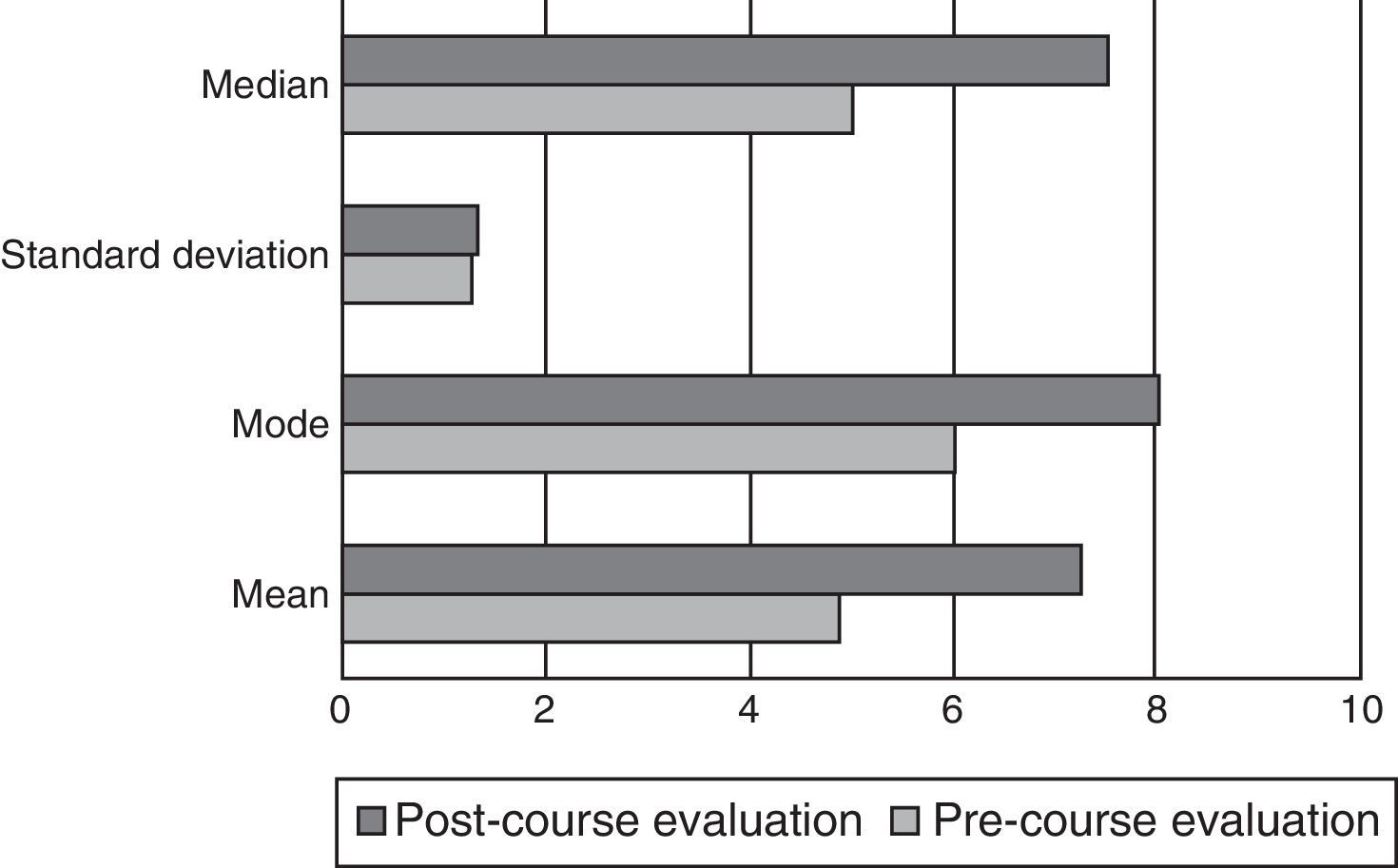
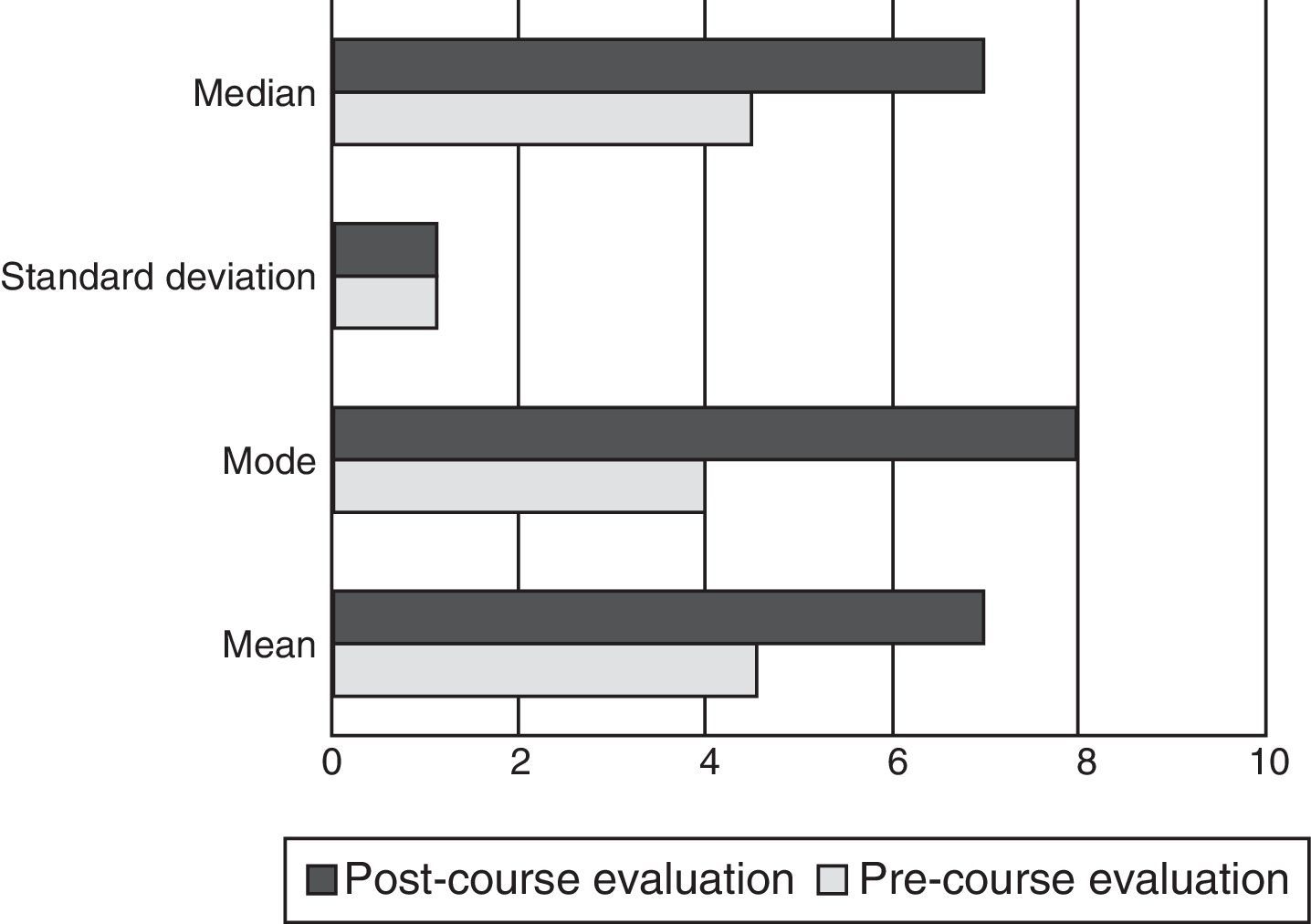
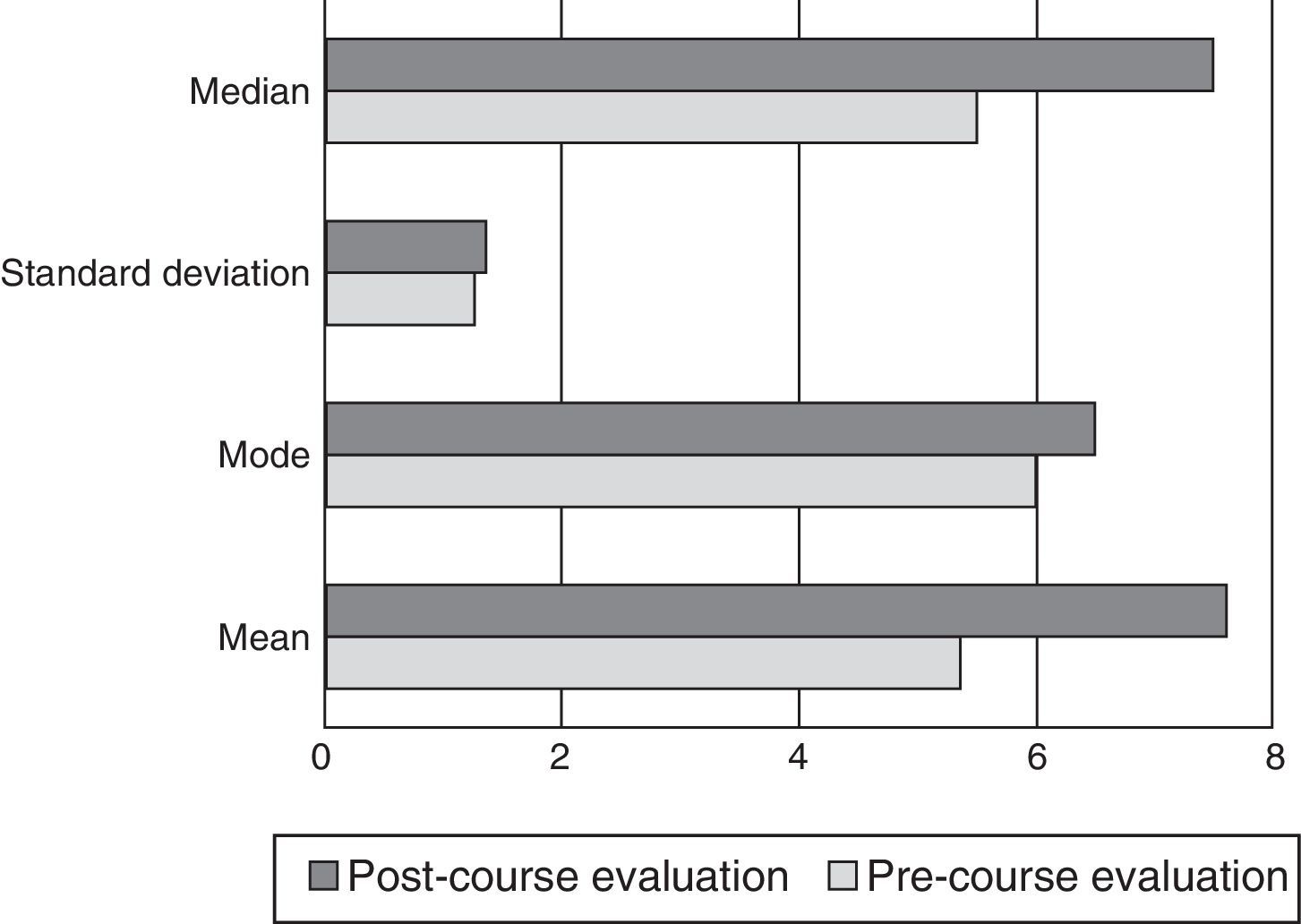
The mean, the standard deviation, mode and median of the pre-course and post-course evaluations were obtained from the total sample (groups A and B) and for each group. The software package IBM SPSS Statistics 20 was used for the statistical analysis, using Pearson's correlation coefficient for the analysis in each group.
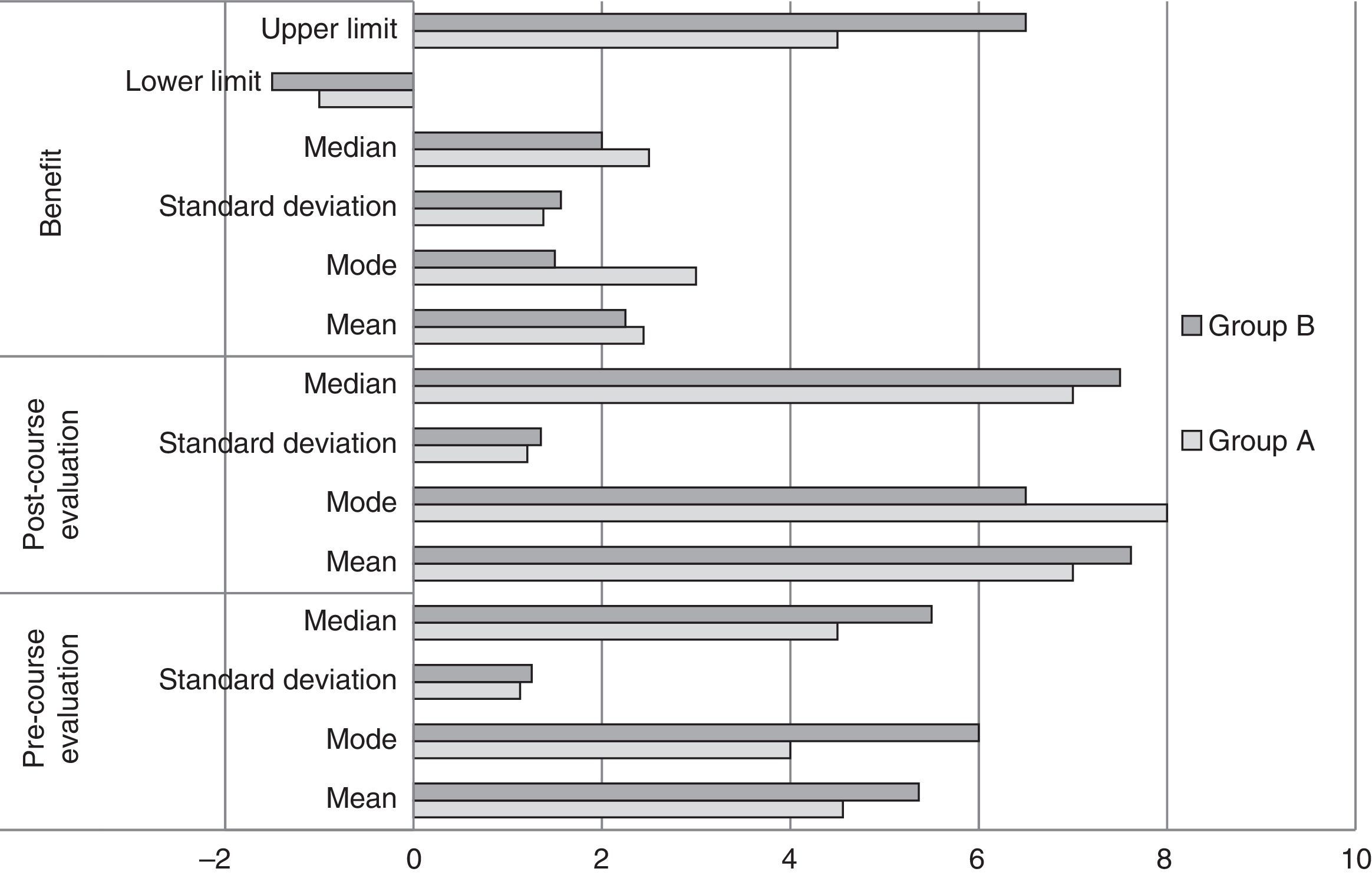
The benefit of the course was assessed as the difference between the score in the post-course evaluation questionnaire minus that obtained in the pre-course questionnaire for each student; the mean, the SD, the mode and the median of this difference was obtained for each group. The highest and the lowest scores were recorded in each group as well.
In order to compare each group, the Student's t-test was used to prove or disprove the statistical difference in the means of both groups in the pre-course evaluation, in the post-course evaluation and in the benefit from the course.
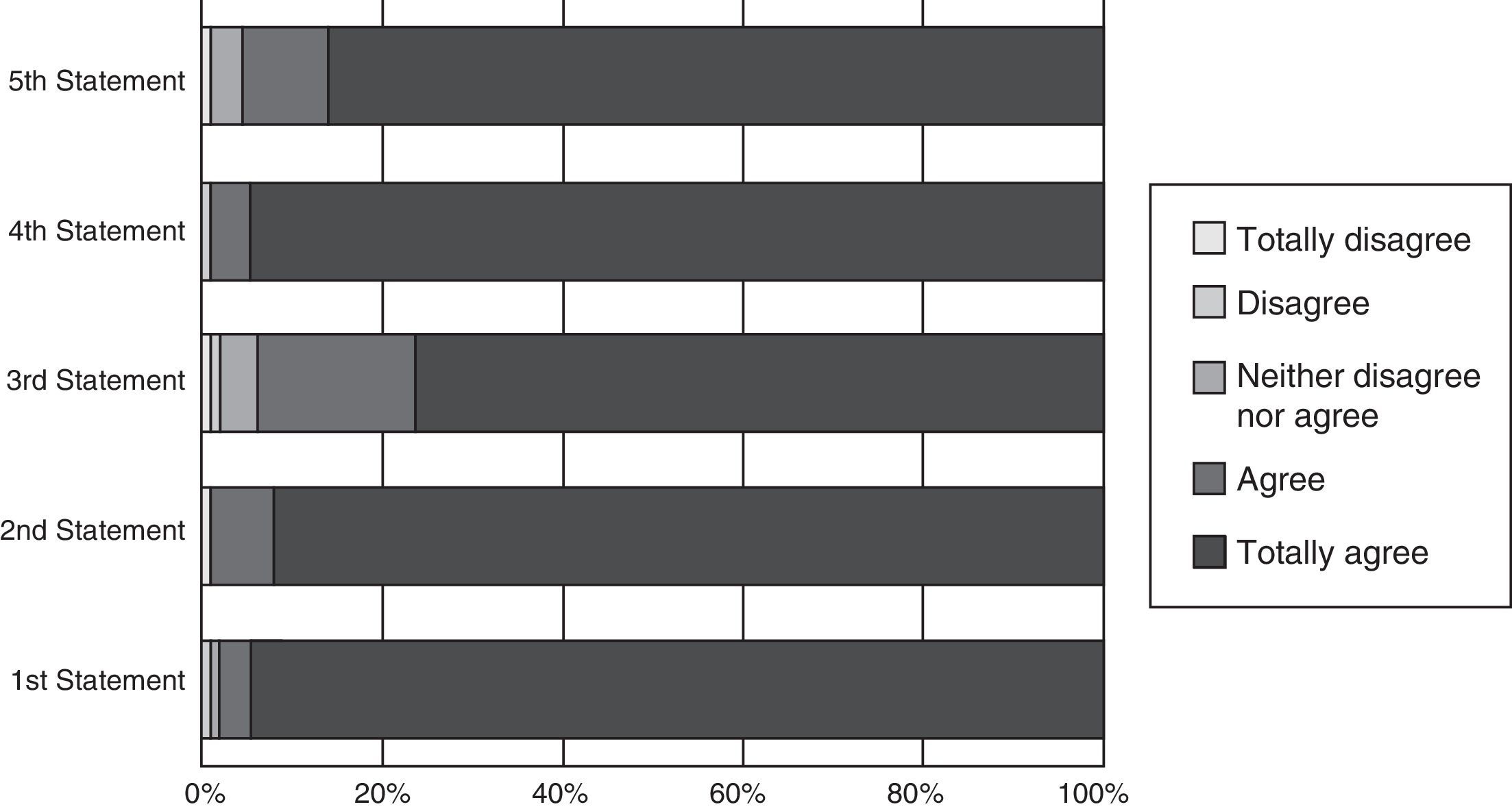
The students expressed their level of satisfaction with and perception of the course in a survey which included the following statements: (1) the objectives of the course were achieved; (2) the Trauma Evaluation and Management course improved my trauma knowledge; (3) the course improved my clinical trauma skills; (4) in general I was satisfied with the Trauma Evaluation and Management course, and (5) the Trauma Evaluation and Management course should be a compulsory element in the Medicine degree curriculum. The students gave their opinion marking each statement on a scale from 1 to 5, 1 being total disagreement and 5 total agreement.
ResultsThe results from all of the students (n=115) are shown in Fig. 1. A statistical difference was demonstrated in the total sample between the initial evaluation and the final evaluation (p<0.01).
Group A (Fig. 2)In this group a statistical difference was observed between the pre and post course evaluations (p<0.01). The mean benefit was 2.44 (SD=1.37), the mode, 3, and the median 0.5; the least benefit was −1, and the greatest was 4.5.
Group B (Fig. 3)No statistically significant difference was demonstrated between either test in this group (p>0.05). The mean benefit was 2.25 (SD=1.56), the mode, 1.5, and the median, 2; the least benefit was −1.5, and the greatest was 6.5.
Comparison between groups (Fig. 4)A statistically significant difference was obtained in the pre-course evaluation between both groups (p<0.01), as with the post-course evaluation (p<0.05); by contrast, there were no statistical differences in benefit between either group (p>0.05).
With regard to student satisfaction (Fig. 5), none of the students stated that they totally disagreed (0%); one disagreed (0.87%) and one said that they neither agreed nor disagreed (0.87%), 4 agreed (3.48%), and 109 (94.78%), totally agreed with the first statement. One student completely disagreed (0.87%), none of the students stated that they disagreed (0%), nor did any say they neither agreed nor disagreed (0%), 8 (6.96%) students agreed and 106 (92.17%) said that they totally agreed with the second statement. One student totally disagreed (0.87%) another disagreed (0.87%), 5 students said they neither agreed nor disagreed (4.35%), 20 (17.39%) agreed and 88 (76.52%) totally agreed with the third statement. None of the students totally disagreed (0%), one (0.87%) student disagreed, none of the students neither agreed nor disagreed (0%), 5 agreed (4.35%) and 109 (94.78%) totally agreed with the fourth statement. Finally, one student totally disagreed (0.87%), none of the students disagreed (0%), 4 (3.48%) neither agreed nor disagreed, 11 agreed (9.56%) and 99 totally agreed (86.09%) with the fifth statement.
Survey statements. First: the objectives of the course were met. Second: the Trauma Evaluation and Management course improved my trauma knowledge. Third: the course improved my clinical skills in trauma. Fourth: in general, I was satisfied with the Trauma Evaluation and Management course. Fifth: the Trauma Evaluation and Management course should be compulsory on the Medical degree curriculum.
The Trauma Evaluation and Management course improved cognitive trauma skills as demonstrated in other countries such as Canada,6 Australia7 and Jamaica8; however, the statistical difference in benefit was only demonstrated in the basic cycle students and not in the clinical cycle students. Comparing both groups, the clinical cycle students had a higher score in the pre-course and the post course evaluation questionnaire compared to the basic cycle students, with a statistically significant difference; this means that the third and fourth grade students achieved better scores than the first and second year students in both evaluations. This coincides with Cherry et al.,9 however, he demonstrated that the fourth-year students had higher scores than the third-year students in a college in the United States.
The benefit was similar for the clinical cycle and the basic cycle students, their score improved consistently.
The lack of statistical improvement in benefit for clinical cycle students might be explained by the higher scores in the pre-course evaluation, which represents a lower growth margin; they would have had to improve their score upwards in order to obtain statistical significance. Despite this, when the benefit for both types of students (clinical and basic cycle) there is no difference, as both groups improved their score.
It is an interesting fact that the greatest benefit was found in the clinical cycle group, and the least benefit, which in fact was a step backwards, was also found in this group. This information is difficult to explain and might be an indication for a different line of research.
In terms of student perception, most agreed that the Trauma Evaluation and Management course should be included in the Medical degree curriculum; they also said that they were satisfied with the course.
In order to achieve greater benefit in clinical cycles an expanded Trauma Evaluation and Management could be implemented in which the students receive a practical course which has been demonstrated as a good way to increase their interest,10 and this might be why the clinical cycle students did not increase their score further.
ConclusionThe Trauma Evaluation and Management course should be part of the Medical curriculum as it improves the trauma cognitive skills of pre-grade students. Although the benefit for clinical cycle students is not statistically significant, the level of knowledge reached in this group is greater, and therefore we suggest that the Trauma Evaluation and Management course should be implemented for clinical-cycle students. Furthermore, the Trauma Evaluation and Management course is well accepted by medical students, and therefore its inclusion in their degree course would not be disputed.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Delgado-Reyes L, Gasca-González OO, Delgado-Guerrero F, Reyes-Arellano W. Efectividad del curso Evaluación y Manejo del Trauma en estudiantes de Medicina mexicanos: ¿cuándo implementar? Cirugía y Cirujanos. 2016;84:220–224.