Silent sinus or imploding antrum syndrome is a very rare condition, consisting of a usually asymptomatic spontaneous collapse of the sinus walls and floor of the orbit. It is associated with negative pressures, and when this occurs, it presents with manifestations such as enophthalmos, hypoglobus, and tilt flow orbital floor. As its incidence is very low, it is frequently missed as a diagnosis, and in fact there are currently fewer than 150 cases reported in the literature.
Clinical casesThree patients have been identified in our practice over a period of two years, with different symptoms that influenced the decision of the treatment modality, which were: watch and wait, endoscopic sinus surgery, or endoscopic sinus surgery plus orbitoplasty.
ConclusionsDespite being a rare entity, it stills catches the attention of the ENT, OMF surgery and Ophthalmologist. The diagnosis is mainly radiological, due to the late clinical manifestations and symptomatology.
The treatment should be individualised and based on the symptoms and the individual decision of each patient, firstly by Functional Endoscopic sinus surgery, and once sinus permeability is restored, it may require augmentation surgery of the orbital floor, either with autologous bone implant, titanium or other material. It is important to be aware of this pathology, to know and to suspect it, avoiding misdiagnosis.
El síndrome de seno silente o implosión maxilar es una entidad muy rara que consiste en un colapso espontáneo y usualmente asintomático del seno maxilar y el piso de la órbita asociado a presiones negativas. Se presenta generalmente con manifestaciones como enoftalmia, hipoglobus e inclinación caudal del piso de la órbita. Debido a su baja incidencia se encuentra infradiagnosticado por la falta de sospecha clínica; menos de 150 casos han sido reportados en la literatura médica.
Casos clínicosPresentamos el caso de tres pacientes captados en nuestro servicio en un lapso de 2 años con esta patología y diferente sintomatología, que influyó en la decisión de la modalidad de tratamiento a utilizar: desde expectante, hasta cirugía endoscopica funcional más orbitoplastia con sus diferentes bemoles.
ConclusionesEl síndrome de seno silente, a pesar de ser una entidad nosológica rara, llama la atención del especialista en oftalmología, cirugía maxilofacial u otorrinolaringología. Su diagnóstico, a pesar de su manifestación clínica, es fundamentalmente imagenológico por la aparición tardía de signos clínicos evidentes.
El tratamiento debe ser individualizado y siempre basado en la sintomatología y la decisión personal del paciente basándose en la cirugía endoscópica funcional. Una vez restablecida la permeabilidad, puede requerir cirugía de aumento de piso orbitario con implante de hueso autólogo, de titanio u otro material. Es importante tener en cuenta esta patología, conocerla y sospecharla para poder realizar certeramente el diagnóstico.
Silent sinus syndrome is a very rare condition, which comprises collapse of the maxillary sinus walls and floor of the orbit; it is usually unilateral.1,2 It is associated with negative antral pressure in the absence of symptoms, hence its name, since it becomes clinically evident after it has been established for years.2
It presents clinically as enophthalmos, which is the displacement of the eyeball within the orbit, and hypoglobus, which could be defined as inferior displacement of the eyeball. For this reason, an ophthalmologist is generally consulted rather than a paranasal sinus specialist.1–3
It was first described by Montgomery in 1964 in the pre CT scan era, as enophthalmos caused by sinus disease. Its name was introduced by Soparker et al. in 1994.1,2
It is still considered idiopathic in origin, although there are many theories. Congenital underdevelopment and acquired mechanical theories have been posited. It is most common between the third and fourth decades of life, and affects both sexes equally. The disease develops generally and progressively over years.4,5
In addition to the physiognomic situation, there can be double vision and other signs, such as retraction, ptosis, lid lag, dry eye or lagophthalmos.2,4,6
Diagnosis is essentially clinical, endoscopic and imaging based, provided there has been no trauma, previous surgery or known sinus disease.
Endoscopically, the middle meatus is observed to have broadened; in general the uncinate process is atelectatic or is not visible due to lateral displacement of the middle concha. Aetiologically, it has not been established whether this is the cause or the consequence of the disorder.7,8
In terms of imaging tests, the reference standard is a single tomography scan, to assess the bone situation with a bone window (2000–4000HU) on two axial and coronal slices, and the axial slices show internal retraction of the medial and superior wall of the maxillary sinus and a reduction in its volume. The lateralised uncinate process can be seen on the coronal slices, the widened middle meatus, inferior displacement of the floor of the orbit and increased volume of the orbital cavity. The floor of the orbit that corresponds to the roof of the affected maxillary sinus is retracted and thinned. Opacification can be partial or complete, and the infundibulum is almost always occluded.6,7
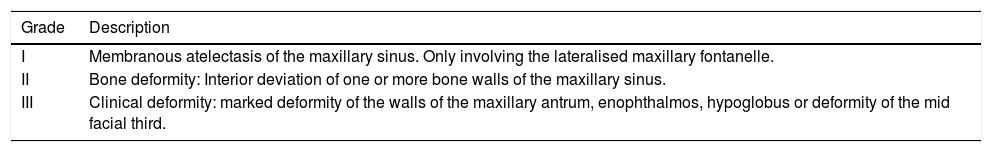
Kass et al. suggested a classification for atelectasis of the maxillary sinus as membranous when there is lateralisation of the maxillary fontanelle only (Grade I), when there is bone involvement (Grade II), and evidently clinical disease with enophthalmos, hypoglobus or deformity of the middle third of the face (Grade III)3 (Table 1).
Kass classification.
| Grade | Description |
|---|---|
| I | Membranous atelectasis of the maxillary sinus. Only involving the lateralised maxillary fontanelle. |
| II | Bone deformity: Interior deviation of one or more bone walls of the maxillary sinus. |
| III | Clinical deformity: marked deformity of the walls of the maxillary antrum, enophthalmos, hypoglobus or deformity of the mid facial third. |
CMA classification according to Kass et al.3
Because the disease is so rare, either spontaneous or associated with a potential trigger,9 and there is no suspicion, it is an under diagnosed entity, with the consequent delay or limitation in its definitive treatment.10
Clinical casesReview phaseIn the last two years, three cases of silent sinus syndrome were referred to our ENT and head and neck surgery department; two were male and one female, ranging from 35 to 50 years of age.
Only one of the patients complained of facial asymmetry, the remainder were asymptomatic.
A complete history was taken from all the patients, and they all underwent physical examination and endoscopic examination of the nasal cavity. It is important to mention that in their targeted interview none of the 3 cases reported a history of facial trauma, nearby explosions or detonations, or any dento-alveolar, nasoethmoidal or maxillomandibular fractures. They then underwent confirmatory imaging tests.
Clinical case 1A 37-year-old man with chronic renal failure, referred to our unit's nephrology department to undergo the elimination of septic foci protocol, awaiting kidney transplantation.
The patient was asymptomatic; however during the targeted interview he mentioned a slight sensation of double vision with upward deviation of the eyes, and no history of facial traumatism. Mild ocular asymmetry was observed clinically, with right enophthalmos compared to the contralateral eye.
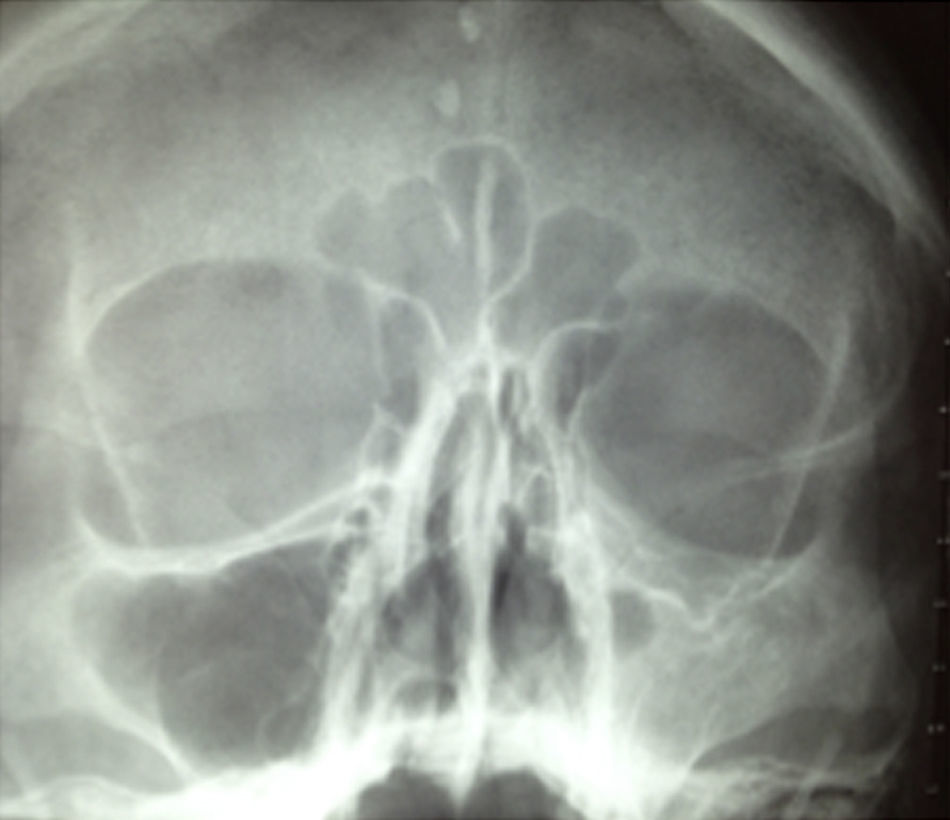
Plain X-rays revealed opacity in the right maxillary sinus, therefore a tomography study was performed which showed a mild increase in orbital volume, with an opaque atelectatic maxillary sinus with soft-tissue isodensity in its interior (Fig. 1).
The nasal endoscopy showed normal mucosa, functional aligned septum, lateralisation of the right nasal wall, the ostium of the maxillary sinus was not visualised, and the uncinate process was lateralised and anterior, with the middle concha implanted in the floor of the orbit.
A diagnosis was made of silent sinus syndrome, and therefore the ophthalmology department was asked to assess the patient. He was deemed not to be a candidate for surgery to the floor of the orbit, and therefore underwent endoscopic surgery of the nose and PNS, with right middle meatotomy, uncinectomy and restoration of permeability, with widening of the maxillary sinus ostium. He was discharged adequately asymptomatic, and made very good progress in postoperative follow-ups.
Clinical case 2Our second case is a 47-year-old woman who also attended our department to undergo the elimination of septic foci protocol due to a diagnosis of rheumatic heart disease with a double mitral lesion, scheduled for valve replacement surgery.
At the consultation she reported a concern about facial asymmetry but no nasosinusal symptoms or history of facial trauma (Fig. 2).
Plain X-rays showed opacity and medialisation of the left jaw and apparent lowering of the orbital floor, and therefore computed tomography of the nose and PNS in the bone window was requested as a complementary imaging study (Fig. 3).
Tomography showed a reduction in the size of the maxillary sinus, entirely occupied by soft-tissue isodensity, with thickening of its lateral wall, slight elevation of the canine fossa and an evident lowering of the orbital floor, with lateral displacement of the infraorbital canal. Similarly, there was evident opacification due to soft-tissue isodensity in the anterior ethmoid sinus, which suggested pathological involvement of other paranasal sinuses, in addition to the affected sinus. The orbital soft-tissue showed normal characteristics.
Because there were so few symptoms and in accordance with the patient's wishes, surgery was not performed and we opted for monitoring and surveillance.
Clinical case 3A 48-year-old, employed male with no comorbidities or history of facial trauma or other relevant events, referred to our department by the ophthalmology department due to double vision, plus “sunken eye”, and bilateral nasal congestion with right predominance, constant, insidious frontofacial headache, accompanied with constant yellowish-white rhinorrhoea with right predominance. Visual acuity was 20/25 in each eye, and there was relative enophthalmos of 4mm, with deep upper sulcus and palpebral retraction in downwards gaze. There was no clinical presentation of limited ocular movements.
On ENT examination the right jaw was observed to be lower than the contralateral jaw. Nasal endoscopy revealed a straight nasal dorsum and mesorrhine nose, aligned functional septum, with a tumour of polypoid appearance in the right nostril apparently coming from the middle meatus, class II Lildholdt. Yellowish bridges of mucus were observed towards the middle meatus.
Tomographic imaging showed, as in the previous cases, an image of a collapsed and occupied right maxillary sinus, with soft-tissue isodensity in the middle meatus extending towards the upper portion of the inferior concha.
Given the clinical and imaging findings, and the abovementioned findings, functional surgery to the nose and paranasal sinuses was scheduled, using an endoscopic approach plus orbitoplasty with repair of the orbital floor.
The procedure was performed under general anaesthetic. We performed a middle meatotomy, resection of the polypoid tumour and drainage of the maxillary sinus using an endoscopic approach.
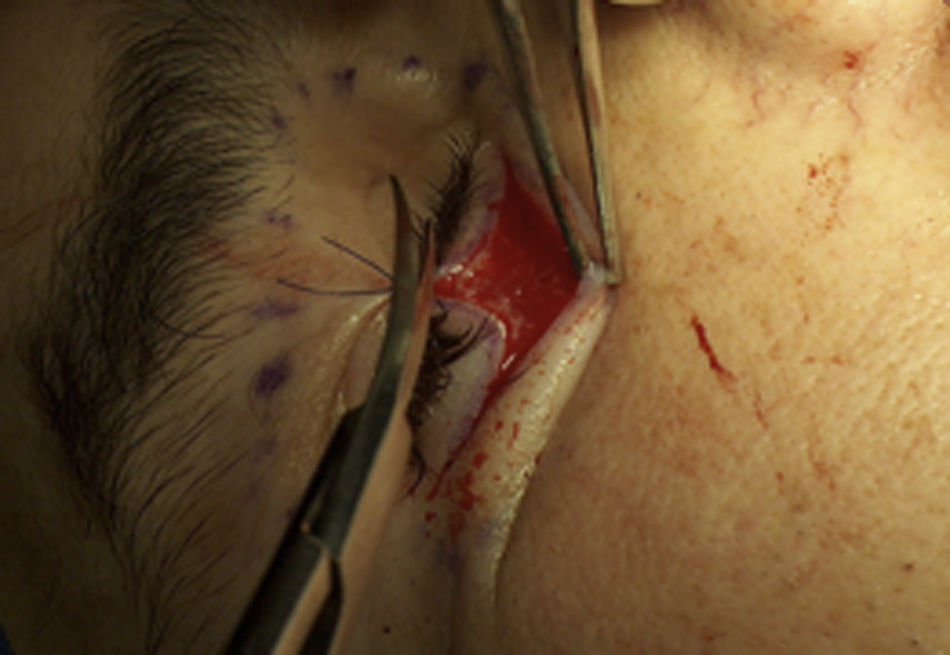
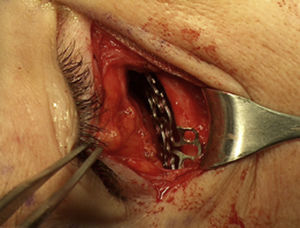
A “Converse Tambin”, also termed subciliary, approach was used for the orbitoplasty. The orbital socket was prepared and appropriately indicated (Fig. 4).
First a temporary tarsorrhaphy was performed with silk to protect the eyeball. The approach was made with a horizontal incision parallel to the ciliary line two millimetres below the base of the eyelashes, extended laterally 10-12mm to expose the entire lower rim.
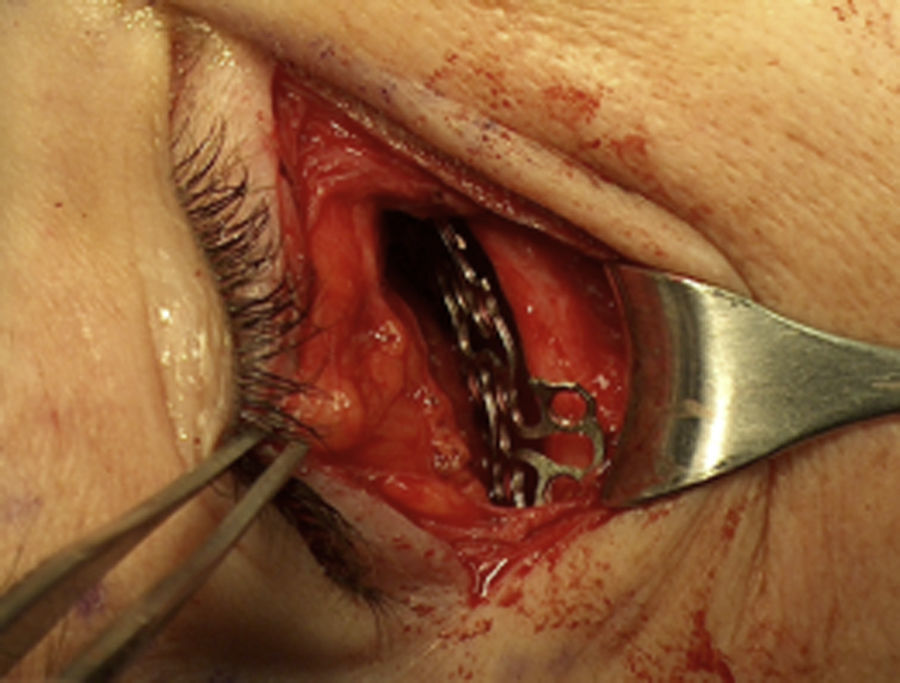
Then we dissected between the skin and the orbicularis muscle until we reached the orbital rim, where we resected the muscle and the periostium to the orbital bone, with the scalpel blade, avoiding the insertion of the orbital septum and the infraorbital nerve (5–7mm below the rim); we separated the edges to inspect the orbital floor.
A titanium mesh was selected and placed over the orbital floor and rim, fixed with monocortical screws 4mm in length. The deep tissues were repaired with vicryl 4-0, and the skin with subdermal nylon 4-0 (Fig. 5).
Once palpebral and orbital symmetry had been achieved postoperatively, the patient was discharged home the day after surgery, with remission of the orbital and nasosinusal symptoms, and an excellent postoperative outcome (Fig. 6).
DiscussionGiven these patients’ clinical and radiological features, it is important to consider and rule out other causes of spontaneous enophthalmos. Silent sinus syndrome or imploding antrum syndrome is a rare entity, and the events that lead to the disorder remain unknown.10–12
Numerous studies suggest dysfunction of the Eustachian tube results in pulmonary atelectasis. Some articles on the equalising function of sinus air due to the action of the maxillary sinus ostium report a similar mechanism. There is a theory of congenital under development; however the acquired theory has taken on importance, because it has been demonstrated that negative intrasinus pressure exists early, before any clinical sign.13,14
The risk of obstruction of the ostium is always present; although it is not clear whether this is the cause or the result of the sinus collapse.15,16
A differential diagnosis should be made with other causes of enophthalmos and hypoglobus, such as trauma, at any level of the facial anatomy, especially if it occurs to the middle third; scirrhous carcinoma; orbital varices resulting in intermittent proptosis; osteomyelitis; Parry-Romberg syndrome, which is a neurocutaneous syndrome which involves facial hemiatrophy; lineal scleroderma, and lipodystrophy.5,14,16
The uncinate process was lateralised in our patients, which coincides with Bossolesi et al. This might have contributed to the negative intrasinusal pressure and the subsequent collapse of the walls. The facial asymmetry was more obvious in two of the three patients, and was almost imperceptible in the patient who did not undergo surgery.11,12
Imaging studies revealed that all the cases had arching of the affected maxillary sinus walls, and tilt flow orbital floor, especially the first and the third case, as reported by Rose Ge et al.14,16
We present three different types of treatment options in this paper, according to the particular situation of each patient. In the first case functional endoscopic surgery to the nose and paranasal sinuses was performed and the maxillary antrum made permeable, with a successful outcome, examination revealed healthy mucosa and no inflammation, and drainage of the affected sinus was re-established physiologically. The second patient, who chose to be managed by monitoring and surveillance, is undergoing serial endoscopic and imaging checkups and remained asymptomatic 25 months following diagnosis. The third patient, who underwent functional endoscopic surgery to the nose and paranasal sinuses plus orbitoplasty, was free from ocular manifestations, including enophthalmos and was satisfied with their outcome and appearance, at the follow-up at 24 months.17–19
Surgical management should be individualised depending on the symptoms, and the patient's individual decision, after they have been informed about the condition, its prognosis and natural curve.19,20
ConclusionsSilent sinus syndrome, although a rare nosological entity, catches the attention of ophthalmology and ENT specialists. Its diagnosis, despite its clinical manifestation, is essentially imaging based, due to the late onset of obvious clinical signs
Treatment, if symptomatic, is based on functional endoscopic surgery, and once permeability has been restored, can require augmentation of the orbital floor, with an implant of autologous bone titanium or other material.
It is important to take this disorder into consideration, be aware of it and suspect it to reach an accurate diagnosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe authors have no relevant source of funding to disclose.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Chavez-Montoya R, Araujo-Ramírez O, Castillo-López IY, Govea-Camacho LH. Síndrome de implosión maxilar: Tres casos y sus diferentes abordajes de tratamiento. Cir Cir. 2017;85:529–534.