Marjolin's ulcer is defined as the appearance of a neoplasm within a chronic wound. The most common histological type is squamous. A total of 2 cases treated in our hospital are presented.
Clinical casesCase 1. A 71 year old man who presented with redness and suppuration from the wounds he had in his right foot after an electric shock 40 years earlier. The radiology showed involvement of the 4° and 5° metatarsal. Supracondylar amputation was performed, showing a well-differentiated invasive squamous cell carcinoma. Case 2. A 56 year old male, paraplegic for 20 years. He was treated due to an infected right heel ulcer, with partial improvement, but the ulcers persisted. Biopsy was performed, reporting as epidermoid carcinoma. Infracondylar amputation was performed. The diagnosis was a well-differentiated squamous cell carcinoma infiltrating the dermis.
ConclusionThe prevalence of Marjolin's ulcer is 1.3–2.2% of all ulcers. Diagnosis is difficult, so biopsy is recommended on any suspicious lesion or ulcer that has received conservative treatment for one month without improvement, although this time limit is not clear. The treatment is the surgery. Local excision with a margin of an inch is enough. If the ulcer is extensive, amputation is required. Survival is estimated between 66 and 80% at 2 years, with recurrence rates of 23%. Unfavourable factors are poor tumour differentiation and metástasis, appearing in 20% of cases.
La úlcera de Marjolin se define como la aparición de una neoplasia en el seno de una herida crónica. La histología más frecuente es epidermoide. Presentamos 2 casos tratados en nuestro hospital.
Caso clínicosCaso 1. Varón de 71 años que consultó por supuración y enrojecimiento de las heridas que presentaba en el pie derecho, tras una descarga eléctrica 40 años antes. En la radiología se apreciaba afectación del 4° y 5° metatarsianos y del tarso. Se realizó amputación supracondílea, con resultado de carcinoma epidermoide bien diferenciado infiltrante. Caso 2. Varón de 56 años, parapléjico desde hacía 20 años. Es tratado por úlcera en talón derecho sobreinfectada, con mejoría parcial pero con persistencia de la lesión ulcerosa. Se realizó biopsia, de la que se informó como carcinoma epidermoide. Se realizó amputación infracondílea. El diagnóstico fue de carcinoma escamoso bien diferenciado que infiltraba la dermis.
ConclusionesLa prevalencia de la úlcera de Marjolin es de 1.3-2.2% de todas las úlceras. El diagnóstico es difícil, por lo que se recomienda biopsia de toda lesión sospechosa o de cualquier úlcera, que después de 1 mes de tratamiento conservador (aunque este límite es impreciso) no presenta mejoría. El tratamiento es quirúrgico; la escisión local con margen de un centímetro es suficiente; si la lesión es extensa es necesaria la amputación.
La supervivencia se estima entre el 66-80% a los 2 años, con tasas de recurrencia del 23%. Los factores desfavorables son la pobre diferenciación y las metástasis, que aparecen en el 20% de los casos.
Marjolin's ulcer is defined as the appearance of an invasive neoplasm in a chronic wound of any origin. According to Onesti et al.,1 the first description of malignant transformation of a scar on the skin is attributed to Celsius in the first century. However, it was Jean Nicolas Marjolin, in 1828, who described the ulcer which bears his name as a post-burn scar which turns malignant. Currently all cancers in chronic wounds are included under the definition of Marjolin's ulcer, and cases of all types have been described: those caused by burns, chronic venous ulcers, pressure ulcers, traumatic wounds, traumatic wounds, areas around a stoma, lupus, chronic lymphoedema ulcers, amputation stumps, chronic pilonidal sinus, hidradenitis suppurativa, necrobiosis lipoidica, chronic osteomyelitis fistula, freeze wounds, partial or total skin graft donor areas, neuropathic ulcers or snake bite ulcers.1,2 The inflammatory environment of chronic ulcers affects the pathophysiology of the lesion, as does the abundance of cytotoxic products deriving from the activity of macrophages in the wound. Although cases have been described where basal cell tumours and melanomas have appeared,1 the most common in terms of histology is the epidermoid strain.
We present 2 cases, diagnosed and treated in our Diabetic Foot Unit over the last 10 years.
Clinical casesClinical case 1A 71-year-old male with no medical history of interest. At the age of 40 he suffered a high energy shock (during an electrical storm, the bolt struck him in the occipital region (Fig. 1), exiting through his right foot). He consulted the Emergency Department of our hospital with suppuration and reddening of the ulcers that he incurred as sequelae from the accident (Fig. 2) in his lower right limb. Plain X-ray of the foot revealed large bone involvement of the forefoot (Fig. 3), with no changes in the vascularisation of the lower limbs visible on magnetic resonance angiography. Given the extension of the lesion, a below-knee amputation was decided, which took place without incident, and the patient was discharged from hospital.
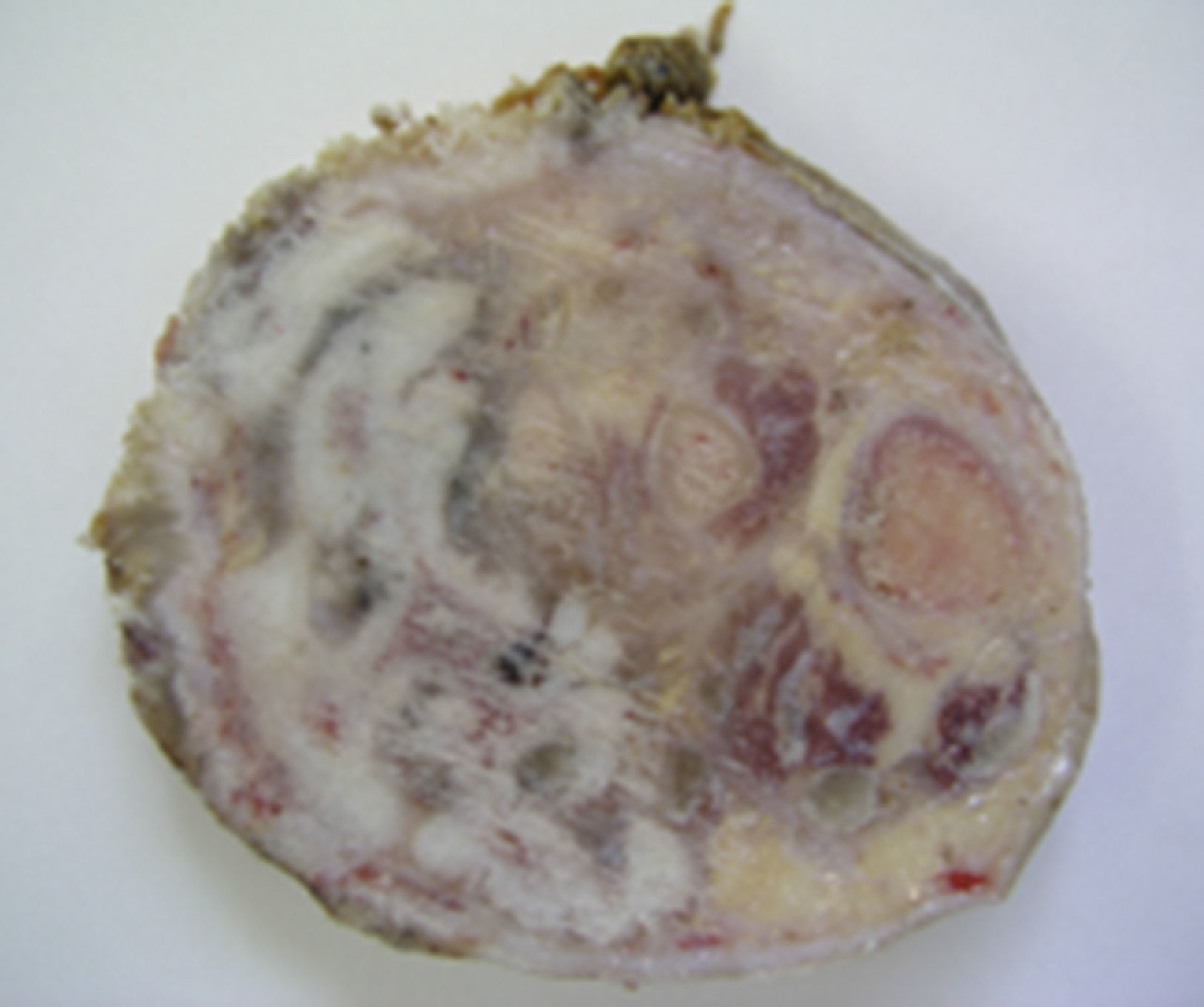
The pathological anatomy study report (Fig. 4) was of a well-differentiated epidermoid carcinoma which was infiltrating the dermis, subcutaneous soft tissues, striated muscle fibres and spongy bone. The postoperative outcome was satisfactory, and the patient was discharged on the 8th day. At 5-year follow-up the patient was free from disease.
Clinical case 2A 56-year-old male, paraplegic after a road accident 20 years previously and being monitored in the National Paraplegic Centre in Toledo. He came to our Emergency Department with an ulcer on the right heel which had developed over a few months (Fig. 5). On examination he presented an ulcer 4cm×7cm, with raised edges, with fibrin and granulation tissue at its base, no slough, and associated cellulitis of the leg up to the popliteal fossa; there was no crepitation. Both the pedal and posterior tibial arterial pulses were present. There were no signs of bone involvement on plain X-ray. Conservative management with local cures and intravenous antibiotherpy was decided. Gradual improvement of the cellulitis was achieved until it resolved with discreet decrease in the size of the ulcer. However, in the following weeks the patient suffered another episode of cellulitis, with no apparent changes in the size or characteristics of the ulcer which responded again to antibiotherapy. After 8 weeks’ follow-up the lesion had not resolved, a biopsy was performed of the edge of the ulcer and the anatomical pathology report showed dysplastic changes with invasive epidermoid carcinoma.
Given the extent of the lesion, a below-knee amputation was performed, without incident in the post-operative period. The anatomical pathology report showed a well-differentiated squamous cell carcinoma infiltrating the entire thickness of the skin. At 2-year follow-up there were no signs of local or distant relapse.
DiscussionSquamous cell carcinoma of the skin is the second most common skin cancer after basal cell carcinoma. It can appear de novo or in skin damaged by precancerous lesions such as actinic keratosis or Bowen's disease. In the case of chronic wounds, although any histological type of neoplasm can appear, the most common is squamous cell carcinoma.
The incidence of Marjolin's ulcer is estimated at 1.3–2.2%1,3 of all chronic ulcers, and increases with the years over which the ulcerous lesion develops. Cases have been described of the cancer appearing up to 40 years after the initial lesion,4 although the mean from the start of the ulcer to diagnosis of squamous cell carcinoma is 9 years.1
It is considered that its origin is multifactorial, and that toxins produced by cell lysis, the presence of cells with a high mitotic capacity, an ischaemic environment and poor lymphatic drainage4 create ideal conditions for carcinogenesis. The cells go through processes of hyperplasia of the basal layer, pseudoepithelial hyperplasia and finally atypical changes.5
Diagnosis based on a set of clinical signs and symptoms can be difficult, because the diagnosis is only established by histopathological study and despite the recommendation that all ulcers which do not heal after a reasonable period of time should be biopsied, unfortunately an appropriate time to consider biopsy has not been established. Some authors recommend 3 weeks with conservative treatment.3 By contrast, other authors prefer leaving more time for the ulcers to develop because the ulcers on which these lesions form take several weeks to close completely (diabetic arteriopathy, osteomyelitis fistula, etc.) and they suggest performing a biopsy after 3 or 4 months.1 Although definitive diagnosis is anatomopathological, there can be signs which would recommend taking samples earlier: changes in the characteristics of the ulcer, bleeding or pain if there had been none before. In any case, if a Marjolin's ulcer is suspected, a biopsy should be taken to confirm a diagnosis as soon as possible.
Management is surgical, as long as local excision with a margin of at least a centimetre is feasible. In these cases it is appropriate to apply a partial thickness skin graft to cover the defect. In the extremities, for patients where local surgery is not possible due to spread of the tumour, the size of the tumour or due to the involvement of neighbouring structures or haemorrhage, the affected area needs to be amputated.1 There is controversy as to whether a lymphadenectomy should be performed systematically. Most authors1,4 only recommend lymph node exeresis if the lymph nodes are palpable or proven to be tumorous, and do not recommend performing this prophylactically.
Many alternatives to surgery have been tried.3,5 Treating Marjolin's ulcer with CO25 appears to be effective in very early lesions, with no invasion of the deep tissues and when they are small in size. Other alternatives such as Mohs micrographic surgery (MMS) have been demonstrated as effective in lesions which are difficult to approach surgically (anatomical difficulties) or in early stages, but it is an expensive option which requires a trained team and a great number of patients. For the majority of cases and in most of the centres in which we work, the surgical approach is the norm. In any case the earliest possible diagnosis and treatment is vital, because this influences the prognosis.
In general the survival of these patients is between 66% and 80% at 2 years4; compared with other skin tumours, it has a poorer prognosis. Recurrence after surgery is 23%, with a latency time between exeresis and recurrence of the tumour of 4.6 months.6 The degree of tumour differentiation is one of the most important prognostic factors, so that recurrence increases significantly the poorer the histological grade.3,6 Distant metastases in Marjolin's ulcer occur in 20% of cases and the most common sites are the lymph nodes, the lung and the liver. Tumours which present in the head and neck have a better prognosis, essentially because they present a lower incidence of metastasis than those that occur in the lower limbs.
In our case, the initial lesion in the 2 patients was totally different, as was the time of development until the appearance of the tumour and its invasive capacity. Therefore, in general a high level of suspicion is required in order to achieve the earliest possible diagnosis and treatment.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Garcia-Marín JA, de Alcala Martinez-Gomez D, Campillo-Soto A, Aguayo-Albasini JL. Úlcera de Marjolin: experiencia de 10 años en una unidad de pie diabético. Cirugía y Cirujanos. 2016;84:340–343.