Positioning during neurosurgical procedures is a challenge for surgical teams even if precautions are taken, the mechanisms underlying peripheral nerve injury (elongation, compression or ischaemia) are latent and it is important to know the frequency of occurrence in our environment.
ObjectiveTo analyse the frequency of peripheral nerve injury secondary to surgical positioning.
Materials and methodsProspective study including 163 patients scheduled for neurosurgical procedures. Four groups: supine, lateral, ventral and park bench were analysed by neurological exploration in order to detect injury and relate with risk factors already described.
ResultsIn this study 112 patients were included, two patients who were under park bench position experienced paresthesias in ulnar region of less than 24 hours’ duration; statistically significant correlation with body weight greater than 85kg.
ConclusionThe incidence of peripheral nerve injury is low, understanding the mechanisms that may originate it helps towards prevention and early detection of complications.
El posicionamiento durante el procedimiento neuroquirúrgico es un desafío para el equipo quirúrgico, aun cuando se tomen precauciones los mecanismos causantes de lesión de nervio periférico por elongación, isquemia o compresión es latente y es importante conocer la frecuencia de presentación en nuestro medio.
ObjetivoAnalizar la frecuencia de lesión nerviosa periférica secundaria al posicionamiento quirúrgico.
Material y métodosSe estudió prospectivamente a 163 pacientes (18 a 65 años) llevados a procedimientos neuroquirúrgicos. Grupos de acuerdo con posición quirúrgica programada: decúbito dorsal, decúbito lateral, decúbito ventral y park bench (PB). Se hizo una exploración neurológica detallada al ingreso, al egreso y a las 24h postoperatorias con el fin de detectar clínica de lesión y relación con factores de riesgo descritos en otras series.
ResultadosSe obtuvieron datos completos en 112 pacientes, 2 pacientes posicionados en PB presentaron parestesias en la región cubital con duración menor a 24h; correlación estadísticamente significativa con peso corporal mayor de 85kg.
ConclusiónLa frecuencia de presentación de lesión de nervio periférico es baja, la comprensión de los mecanismos que pueden originarlo ayudan a la prevención y detección temprana de complicaciones.
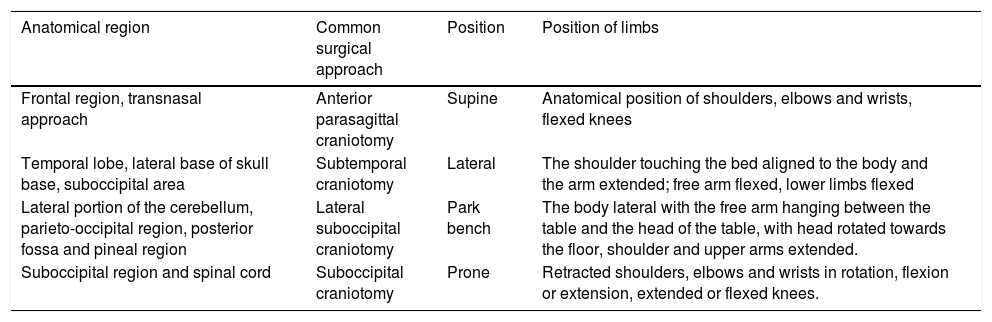
Positioning patients on the operating table is a major challenge to neuroanaesthetists in their daily practice. The location of intracranial lesions requires various approaches to enable appropriate exposure, preserving the surrounding structures to the utmost; this means that the body and limbs are required to adopt forced postures (Table 1).
Common neurosurgical approaches.
| Anatomical region | Common surgical approach | Position | Position of limbs |
|---|---|---|---|
| Frontal region, transnasal approach | Anterior parasagittal craniotomy | Supine | Anatomical position of shoulders, elbows and wrists, flexed knees |
| Temporal lobe, lateral base of skull base, suboccipital area | Subtemporal craniotomy | Lateral | The shoulder touching the bed aligned to the body and the arm extended; free arm flexed, lower limbs flexed |
| Lateral portion of the cerebellum, parieto-occipital region, posterior fossa and pineal region | Lateral suboccipital craniotomy | Park bench | The body lateral with the free arm hanging between the table and the head of the table, with head rotated towards the floor, shoulder and upper arms extended. |
| Suboccipital region and spinal cord | Suboccipital craniotomy | Prone | Retracted shoulders, elbows and wrists in rotation, flexion or extension, extended or flexed knees. |
A detailed preoperative assessment, together with the neurosurgeon, of the physiological dynamics and the impact that positioning can have on each patient is important and thus, the best individualised strategy for positioning can be achieved.1
Despite manoeuvres designed to prevent complications, injury to the peripheral nerve is latent in each case; in fact, in reports by the Closed Claim Project, of the American Society of Anaesthesiologists (AS) setting out the most common injury complaints, 22% involve damage to the peripheral nerve.2 Even taking into account a great number of complications, peripheral nerve injury remains uncertain and can range from 0.03%3 to 0.11%.4
Peripheral nerve damage can occur at any time perioperatively: during venous or arterial puncture, when handling the anesthetised patient to position them appropriately or due to continuous compression in forced positions. The mechanism that causes the injury can be direct, due to elongation, ischaemia and/or prolonged compression; elongation injury can range from irregular ischaemia due to disruption of the intraneural vessels, to rupture of connective tissue causing haemorrhage and necrosis, and there can be oedema in the perineurium.5 Ischaemia secondary to tissue compression can be the result of poor perfusion due to arterial occlusion and interruption of nerve blood supply.6
Therefore, patients with microvasculature disorders, such as those with arterial hypertension,7 diabetes mellitus8 and smokers,9 are particularly vulnerable to the abovementioned mechanisms of injury.
Little is known about the frequency and risk factors of peripheral nerve injury in our environment, especially in neurosurgical patients. The objective of this study was to correlate the incidence of peripheral nerve injury with the diverse positions of the neurosurgical patient.10
Material and methodsA prospective, observational, longitudinal, analytical study performed in the neuroanaesthetics department of the Instituto Nacional de Neurología y Neurocirugía, approved by the institution's scientific and ethics committees.
ParticipantsThis study included 163 patients, ranging in age from 18 to 65 years, from May to November 2010. All the patients had normal preoperative examinations, with no evidence of prior peripheral nerve damage, and ASA I-III physical status. Patients with a Glasgow Coma Scale score lower than 13, those who were discharged intubated or with any postoperative neurological sequelae were excluded.
ProtocolThe participants were distributed into 4 study groups, according to the position programmed for the cranial lesion resection (planned according to the location of the lesion, the patient's morphology and comorbidities): supine, lateral, ventral and park bench (PB).
The type of anaesthesia was chosen at the discretion of each anaesthetist. The surgical position was checked by an experienced attending neuroanaesthetist, and 3 basic safety and quality elements were checked at the time of surgical positioning: (1) pressure area care; (2) protection of organs vulnerable to ischaemia (nose, eyes, genital organs), and (3) distal limb perfusion.
The diagnosis, surgery planned, patient's age, body mass index, chronic/degenerative diseases, smoking and alcoholism, and transoperative incidents were taken into account.
Postoperative evaluationA detailed neurological examination was performed of the limbs, movement, muscle strength, osteotendinous reflexes and sensitivity, on leaving the operating theatre and 24h postoperatively.
Statistical analysisAll the measurements are presented as means±SD. The nominal data were analysed using the χ2 test. The differences between the values were considered significant with a p value <.05. SPSS was used for all the statistical tests and graphs.
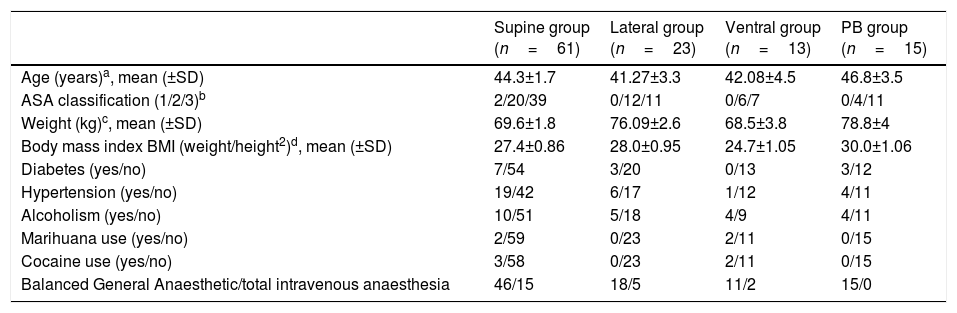
ResultsThis study included 163 patients, of whom 51 had an elimination criterion; 112 patients had the necessary data for the statistical analysis; the demographic data are shown in Table 2.
Demographic results.
| Supine group (n=61) | Lateral group (n=23) | Ventral group (n=13) | PB group (n=15) | |
|---|---|---|---|---|
| Age (years)a, mean (±SD) | 44.3±1.7 | 41.27±3.3 | 42.08±4.5 | 46.8±3.5 |
| ASA classification (1/2/3)b | 2/20/39 | 0/12/11 | 0/6/7 | 0/4/11 |
| Weight (kg)c, mean (±SD) | 69.6±1.8 | 76.09±2.6 | 68.5±3.8 | 78.8±4 |
| Body mass index BMI (weight/height2)d, mean (±SD) | 27.4±0.86 | 28.0±0.95 | 24.7±1.05 | 30.0±1.06 |
| Diabetes (yes/no) | 7/54 | 3/20 | 0/13 | 3/12 |
| Hypertension (yes/no) | 19/42 | 6/17 | 1/12 | 4/11 |
| Alcoholism (yes/no) | 10/51 | 5/18 | 4/9 | 4/11 |
| Marihuana use (yes/no) | 2/59 | 0/23 | 2/11 | 0/15 |
| Cocaine use (yes/no) | 3/58 | 0/23 | 2/11 | 0/15 |
| Balanced General Anaesthetic/total intravenous anaesthesia | 46/15 | 18/5 | 11/2 | 15/0 |
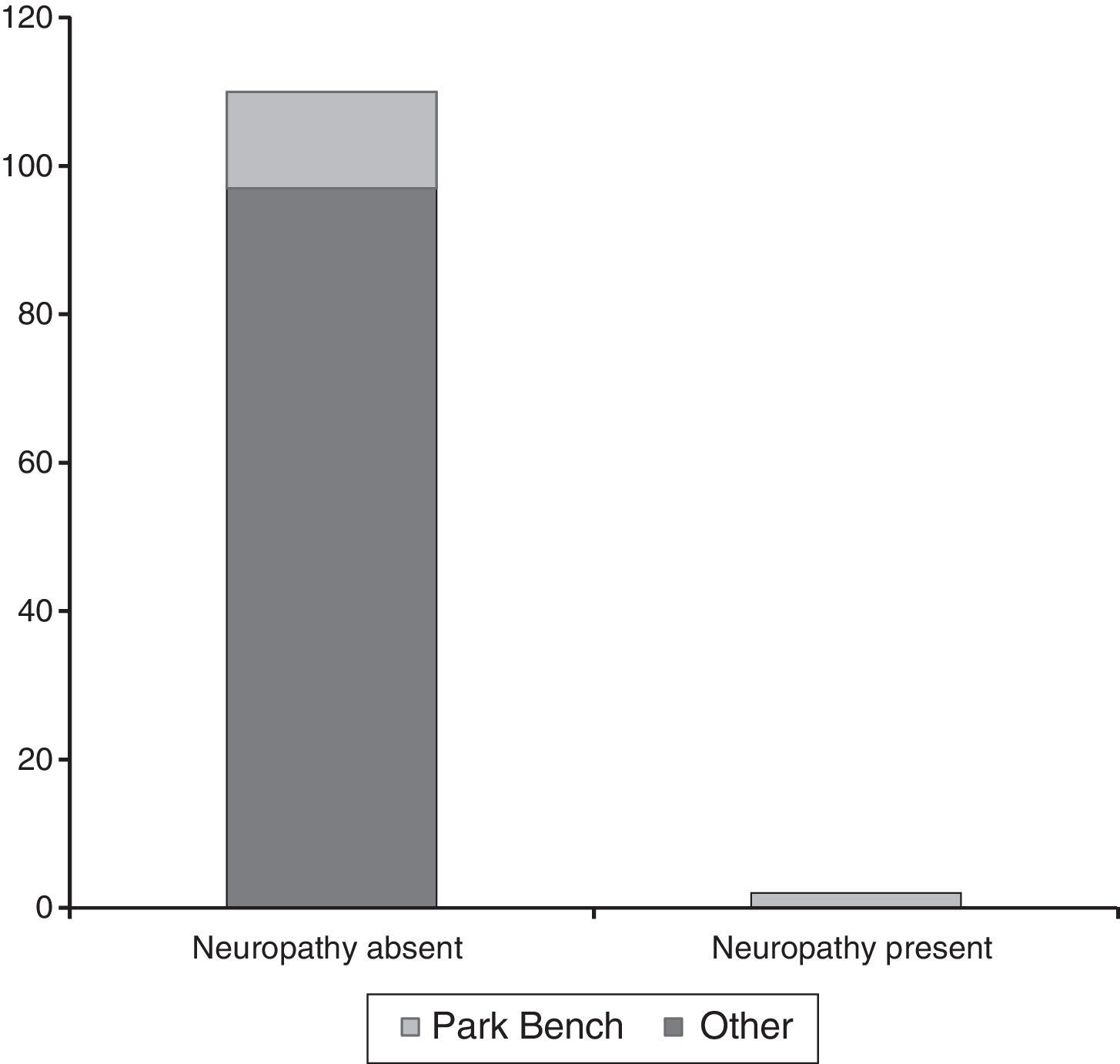
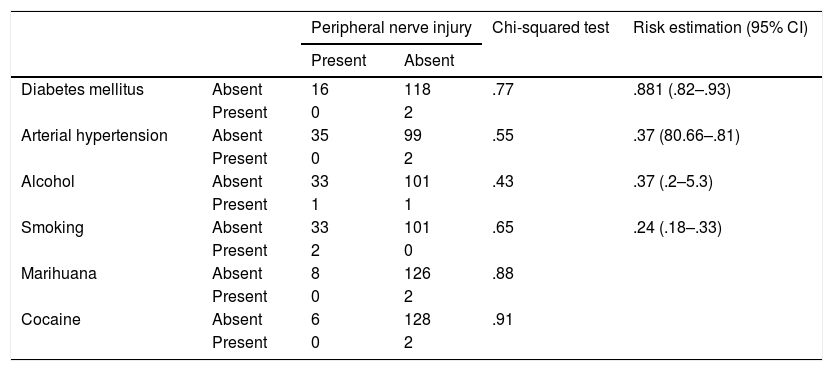
Two cases of peripheral nerve injury were found (1.78%); both patients had paraesthesia of the region innervated by the ulnar nerve with preserved movement, strength and reflexes, the symptom lasted for less than 24h, and remitted completely. The two cases of postoperative paraesthesia belonged to the PB position group, in the thoracic limb that was underneath the surgical table p<.05 (Fig. 1).
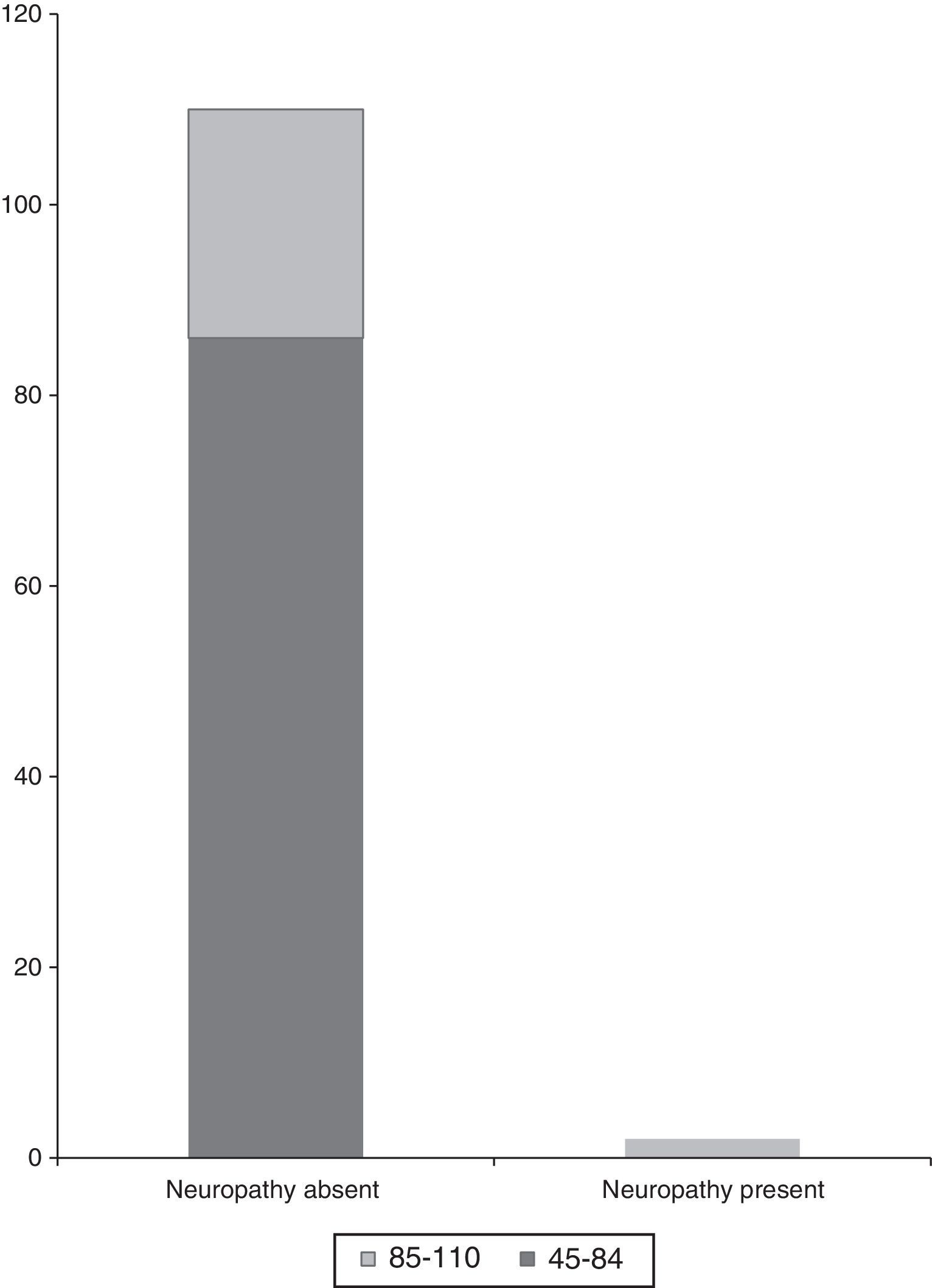
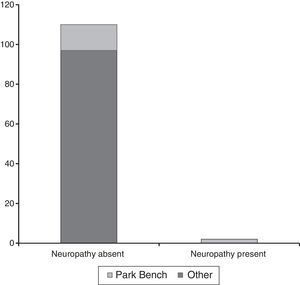
The mean weight of patients who had no peripheral nerve damage was 72.3kg, and 89kg (p<.05) of those who did. Body mass index was not significant in the analysis (Fig. 2).
Thirty-three percent of the patients were smokers, 2 patients with peripheral nerve injury were smokers, no statistical significance presented in the analysis, although a tendency was observed (p=.065).
Among the transoperative incidents, 4 cases of hypotension were reported, of which one was peripheral nerve injury positive (p=.06).
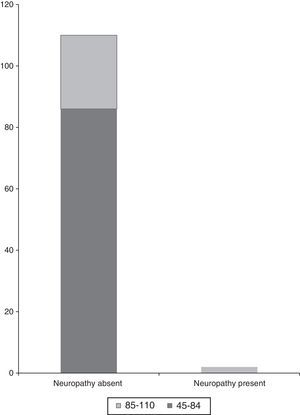
Table 3 shows the analysis of the presence of the variables and their relationship with the presence of peripheral nerve damage.
Correlation of peripheral nerve damage with risk factors.
| Peripheral nerve injury | Chi-squared test | Risk estimation (95% CI) | |||
|---|---|---|---|---|---|
| Present | Absent | ||||
| Diabetes mellitus | Absent | 16 | 118 | .77 | .881 (.82–.93) |
| Present | 0 | 2 | |||
| Arterial hypertension | Absent | 35 | 99 | .55 | .37 (80.66–.81) |
| Present | 0 | 2 | |||
| Alcohol | Absent | 33 | 101 | .43 | .37 (.2–5.3) |
| Present | 1 | 1 | |||
| Smoking | Absent | 33 | 101 | .65 | .24 (.18–.33) |
| Present | 2 | 0 | |||
| Marihuana | Absent | 8 | 126 | .88 | |
| Present | 0 | 2 | |||
| Cocaine | Absent | 6 | 128 | .91 | |
| Present | 0 | 2 | |||
In this study, undertaken exclusively with neurosurgical patients, we found that the frequency of peripheral nerve injury comprised 1.78% of cases (2 cases out of 112); within the range reported in the literature. The largest published case series on injuries secondary to anaesthetic positions is that by Welch et al.,3 who retrospectively studied 380,680 cases from a database of patients who received anaesthesia over a period of 10 years; 480 patients had characteristics for a potential perioperative peripheral nerve injury, of these 359 were removed because they did not meet the perioperative definition of peripheral nerve injury, the 112 remaining patients fulfilled the inclusion criteria, comprising .029% of cases; in the analysis by subgroup, 8.9% (n=13,346) of the neurosurgical patients had peripheral nerve injury.
Menezes et al.11 published a study in 2013 that included 172 patients from all surgical specialties; a frequency of peripheral nerve damage of 4.7% was reported.
In 1987, Alvine and Schurrer12 presented a series of 6538 postoperative cases (none neurosurgical), and found an incidence of .26% (17 patients) ulnar nerve injury. They performed a follow up at 6 months, and found that 5 patients still had discomfort and reduced nerve conduction velocity.
Another of our findings related to position and presence of injury; the 2 patients had been placed in the PB position. This type of surgical position is frequent in the posterior fossa approach; the patient is placed in a lateral position with flexed neck and head rotated towards the floor, the contralateral arm is flexed and hangs free from the head of the operating table, and the other arm is aligned to the patent's trunk.13
In this type of position, the ulnar nerve can be damaged with increased pressure to the ulnar channel at the level of the elbow secondary to excessive flexion of the elbow (>90°)14; this description coincides with the clinical findings reported in the 2 positive cases in our study.
Obesity is one of the risk factors associated with damage to the peripheral nerve and the ulnar nerve in particular, although in the past this condition was associated with thin patients due to the lack of protective subcutaneous fatty tissue.5 The 2 patients from our study who were affected weighed more than 89kg, with a body mass index >30, as reported by Baumann et al.15; overweight patients are vulnerable to compression against the surgical table and the retractor bars, showing reduced amplitude of somatosensory evoked potentials (SSEP). The series by Menezes et al. found that a body mass index greater than 30 is significantly associated with peripheral nerve injury.11
Smoking was another risk factor associated with peripheral nerve injury16; we found no association in our results. Similarly, the affected patients had no other associated substance abuse.
Diabetes mellitus has been reported as a predisposing factor for the condition17; however, we found no correlation with the cases that were positive in our study.
Ischaemia has been proposed by several authors as a pathophysiological mechanism of the injury. In this regard, transoperative incidents were recorded in our study, such as episodes of hypotension,18 which were not statistically significant.
Chronic arterial hypertension is another proposed risk factor that predisposes the blood vessels to ischaemia as it progresses. Neither of the 2 patients affected were reported as hypertensive.3
Nowadays, intraoperative monitoring technology has achieved a reduction in complications across the board; in this case specifically, SSEP have been shown to be useful for the early detection of peripheral nerve injury.15 In a published study by Ying et al.19 485 patients were analysed retrospectively who had undergone microvascular decompression (hemifacial spasm and trigeminal neuralgia) in the PB position; the ulnar and median nerves of these patients were routinely monitored bilaterally by SSEP; only 14 (2.9%) patients had intraoperative changes with a reduction in amplitude of 50%; this change is considered a potential risk for postoperative nerve injury. In these cases, the position of the patient was checked and it was found that excessive traction of the shoulder, hyperextension of the neck and compression of the elbow were the probable causes of this reduction; the patients did not undergo postoperative follow up, therefore we cannot specify the clinical outcome; even when these tools enable us to establish these changes objectively and immediately, apparently the sensitivity of monitoring is low.
Peripheral nerve injury can be difficult to detect and can even go unnoticed by the medical team, especially in a neurosurgical scenario, since patients can considerer the symptoms normal after the event and not report them as important. Likewise, physical neurological examination is limited if an efficient neurological examination is not performed before the patient goes for surgery.
One of the limitations of this study is that there was no objective evaluation such as transoperative or postoperative monitoring of evoked potentials, such as electromyography or conduction velocities. Similarly, the number of patients was low for detecting complications and made comparison between groups difficult.
ConclusionAlthough the frequency of peripheral nerve injury is low and the condition is transitory, it is important to understand the mechanisms that lead to it to prevent its postoperative onset. Although positioning is team work (anaesthetist, surgeon, nurse), it is down to the anaesthetist as a leader in the operating theatre to ensure the optimal placement of the patient on the operating table.
In our centre, at least 4 patients are operated per week in the PB position; broad experience has enabled the development of techniques and solutions to ensure minimal complications for patients. Even so, positioning remains a challenge for neurosurgeons and neuroanaesthetists.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis paper received no source of funding.
Conflict of interestThe authors have no conflicts of interests to declare.
This paper was written as a subspecialty thesis in Neuroanaesthetics for P. Esquivel-Enríquez, endorsed by the National Autonomous University of Mexico. It is also a posthumous homage to Dr. Esquivel-Enríquez’ brilliant but unfortunately short career.
Please cite this article as: Esquivel-Enríquez P, Pérez-Neri I, Manrique-Carmona L. ¿La posición neuroquirúrgica ocasiona lesión de nervio periférico? Cir Cir. 2017;85:493–498.