Liver transplantation in patients with liver cirrhosis, portal vein thrombosis, and cavernous transformation of the portal vein, is a complex procedure with high possibility of liver graft dysfunction. It is performed in 2–19% of all liver transplants, and has a significantly high mortality rate in the post-operative period. Other procedures to maintain portal perfusion have been described, however there are no reports of liver graft perfusion using right gastroepiploic vein.
Clinical caseA 20-year-old female diagnosed with cryptogenic cirrhosis, with a Child-Pugh score of 7 points (class “B”), and MELD score of 14 points, with thrombosis and cavernous transformation of the portal vein, severe portal hypertension, splenomegaly, a history of upper gastrointestinal bleeding due to oesophageal varices, and left renal agenesis. The preoperative evaluation for liver transplantation was completed, and the right gastroepiploic vein of 1-cm diameter was observed draining to the infrahepatic inferior vena cava and right suprarenal vein. An orthotopic liver transplantation was performed from a non-living donor (deceased on January 30, 2005) using the Piggy-Back technique. Portal vein perfusion was maintained using the right gastroepiploic vein, and the outcome was satisfactory. The patient was discharged 13 days after surgery.
ConclusionsLiver transplantation was performed satisfactorily, obtaining an acceptable outcome. In this case, the portal perfusion had adequate blood flow through the right gastroepiploic vein.
El trasplante hepático realizado en pacientes con cirrosis hepática, trombosis venosa portal y transformación cavernomatosa de la vena porta, es un procedimiento de alta complejidad y elevada posibilidad de disfunción del injerto hepático; se realiza en el 2–19% de los trasplantes hepáticos y tiene una mortalidad significantemente alta en el postoperatorio. Se ha descrito la perfusión portal alterna, no obstante no hay reportes de perfusión alterna con la vena gastroepiploica derecha.
Caso clínicoMujer de 20 años de edad con diagnóstico de cirrosis hepática criptogénica Chil-Pugh: «B» 7 puntos, MELD: 14 con trombosis y degeneración cavernomatosa de la vena porta, hipertensión portal severa, esplenomegalia con antecedentes de sangrado del tubo digestivo alto, por varices esofágicas y agenesia de riñón izquierdo. Fue realizado protocolo de trasplante hepático y se observó la vena gastroepiploica derecha con un diámetro de 1cm drenando a la vena cava infrahepática y vena suprarrenal derecha. Se realizó el trasplante hepático ortotópico de donante fallecido el día 30 de enero del 2005 con técnica de Piggy-Back, la perfusión venosa portal se realizó a través de la vena gastroepiploica derecha y la evolución fue satisfactoria, la paciente fue egresada sin complicaciones, 13 días posterior al trasplante.
ConclusionesEl trasplante hepático fue realizado de forma satisfactoria y con buen resultado en el presente caso, ya que la perfusión portal fue llevada a cabo con adecuado flujo a través de la vena gastroepiploica derecha.
Liver transplantation in patients with liver cirrhosis, portal vein thrombosis, and cavernous transformation of the portal vein, is a highly complex procedure with high possibility of liver graft dysfunction. It is performed in 2–19% of liver transplants1 and has been associated with a significantly high rate of post-transplant mortality.2 Absence of the portal flow due to portal vein thrombosis is a multifactorial condition that arises from a combination of heriditary and acquired factors.3 Cirrhosis is the most common aetiological factor, and it is present in 24–32% of cases.4 It presents less often due to other causes, such as cancer, infection, inflammation and thrombophyllic disorders. The incidence of portal vein thrombosis is associated with the severity of the cirrhosis,5 and it is therefore a common problem during liver transplant, developing inside the liver and spreading to the extra hepatic portion of the portal vein. In some cases the thrombosis extends to the mesenteric branches, giving rise to splanchic venous thrombosis.6 Although portal vein thrombosis increases the difficulty of liver transplant7,8 it is not an absolute contraindication.9
If thromboendovenectomy is impossible patients with complete portal vein thrombosis, alternatives for portal reconstruction must be considered.5,10–15 Cavoportal hemitransposition16 and multivisceral transplant17 are options for patients with complete portal vein thrombosis when no collateral veins are present.
Although liver transplant is beneficial for the majority of patients5,10–15 the risks must be carefully considered for those with clinically stable cirrhosis and portal vein thrombosis. The indication must be established for clinically unstable patients, even when there is a risk of postoperative complications and a higher rate of intrahospital postoperative mortality.18,19
In this case of liver transplant we performed portal perfusion using the flow of the right gastroepiploic vein in the absence of portal flow. There are currently no reports of this having been carried out before, so that we present the first case of liver transplant with portal perfusion using right gastroepioploic vein flow.
Clinical caseThe patient is a 20-year-old woman, who received a liver transplant from a donor who died on 30 January 2005, diagnosed with cryptogenic cirrhosis of the liver, grade IV portal hypertension and cavernous degeneration of the portal vein, with a Child-Pugh score of 7 points (stage “B”) and a MELD score of 14. Relevant background: closure of the arterial duct at the age of 11 months due to persistence of the duct, with upper digestive tract bleeding from 5 years of age secondary to bleeding oesophageal varices and the use of sclerotherapies on several occasions, sub-aortic stenosis at 9 years old that was treated conservatively; subsequently diagnosed with portal vein thrombosis, cirrhosis of the liver and left renal agenesis.
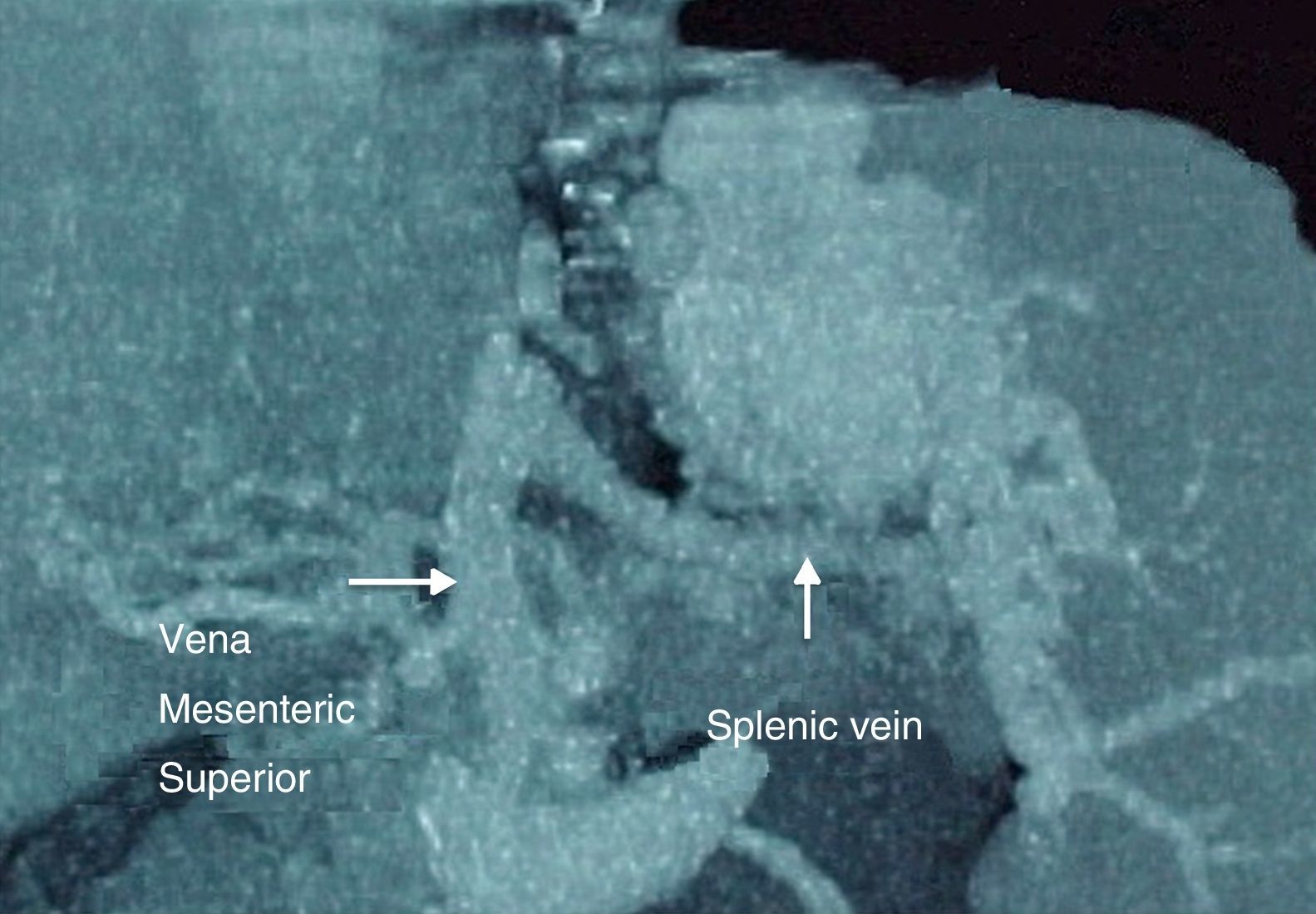
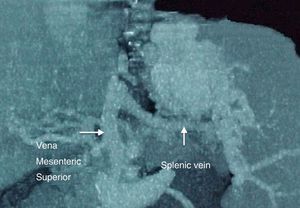
Liver transplant protocol was implemented without contraindications and the relevant data were as follows: Doppler ultrasound scan showed diffuse liver damage, cavernous degeneration of the portal vein with data suggesting portal hypertension, an increase in the diameter and flow of the splenic vein together with splenomegaly. Spleno-portal computerised axial angiotomography showed an accumulation of varices from the lower portion of the oesophagus to the gastric base, with collateral varicose circulation (Fig. 1). Endoscopy of the upper digestive tract showed post-sclerotherapy changes, with integral grade II oesophageal varices and moderate congestive gastropathy without the presence of active bleeding. Reactive antibody panel C1: 24%, CII: 16%.
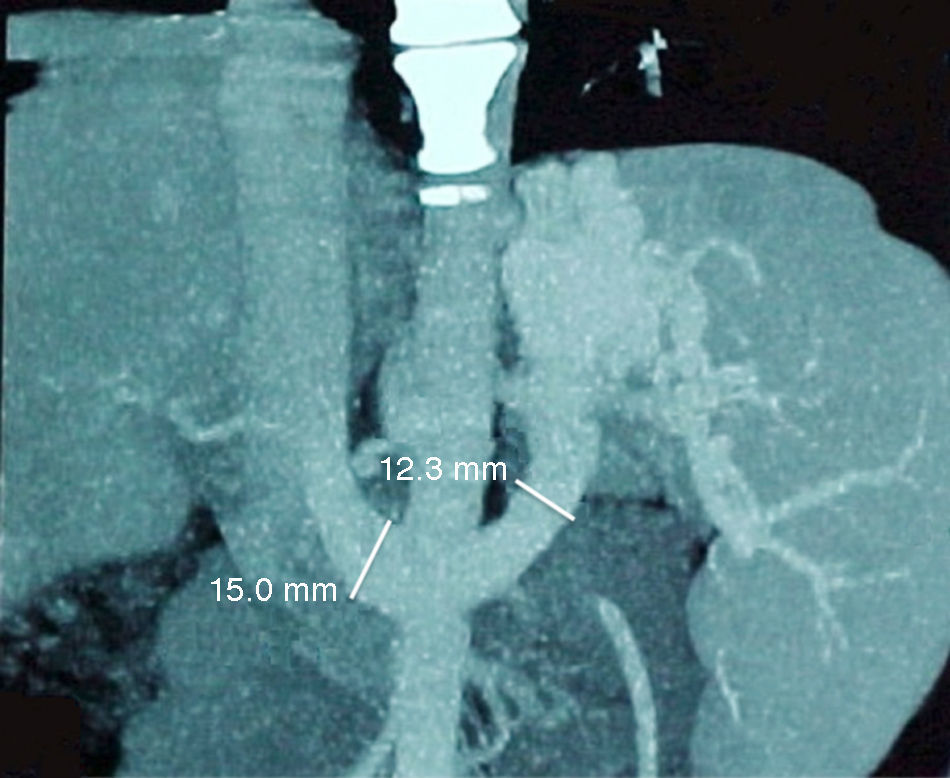
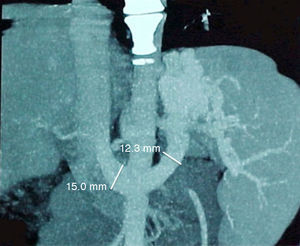
The donor was a 43 year-old woman in the same blood group. In procurement of the liver the preperfusion biopsy showed 8% steatosis with slight subcapsular congestion. Surgical findings in the recipient: spontaneous drainage of the right gastroepiploic vein (2cm in diameter) into the infrarenal vein (Fig. 2). The Piggy-Back orthotopic transplant technique was performed without complications. Venous anastomosis of the recipient suprahepatic veins was performed with the donor cava vein. Arterial anastomosis of the celiac trunk of the donor was carried out with the hepatic artery of the recipient. Portal anastomosis took the following form: donor portal vein – recipient right gastroepiploic vein, and anastomosis of the bile duct was choledoch –choledoch. Ischaemia times were: 1090min cold and 50min warm, while the anahepatic phase lasted for 61min. Transurgical bleeding was 2010ml, recovered (cell saver); 1500ml, with total actual bleeding of 510ml.
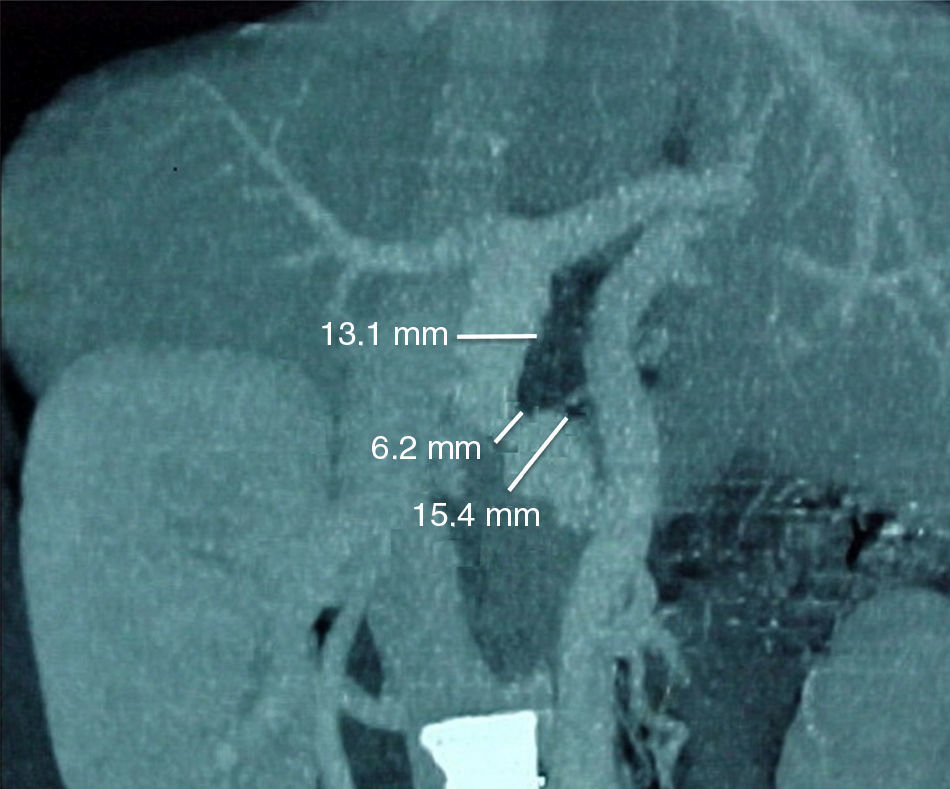
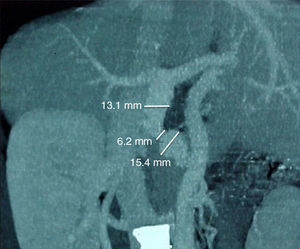
The post-operative liver graft had normal characteristics, with good venous, portal and hepatic artery perfusion (Fig. 3). The patient was extubated in the recovery room and was haemodynamically stable.
Doppler ultrasound scan in the first 24h after liver transplant showed: left portal vein 11mm in diameter with turbulent hepatopetal flow of 17.5cm/s, extrahepatic portal vein 11mm with flow, hepatopetal velocity of 22.3cm/s, the right hepatic artery with systolic flow of 23cm/s and diastolic flow of 9.4cm/s, with a pulsatility index of 8 and a resistance index of 6; the left hepatic artery was permeable and systolic flow was 32cm/s, while diastolic flow was 4.4cm/s and the pulsatility index was 8 and the resistance index was 5; the suprahepatic veins conserved their calibre and trajectory (normal multi-phase flows), the lower cava vein without abnormalities. The maximum values in post-transplant hepatic functioning tests were: aspartate aminotransferase (AST) 3095U/l, alanine aminotransferase (ALT) 6243U/l, total bilirrubin 7.7mg/dl, indirect bilirrubin 1.7mg/dl, direct bilirrubin 6mg/dl. Immunosuppressor treatment used basiliximab, tacrolimus, methylprednisolone, prednisone and mycophenolate mofetil.
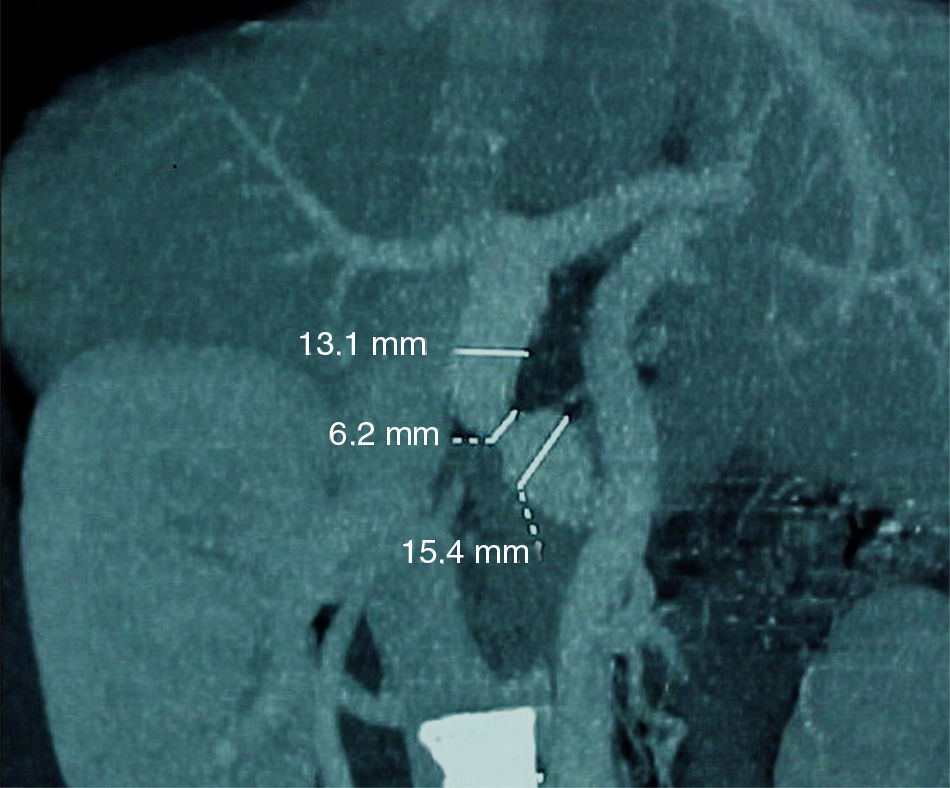
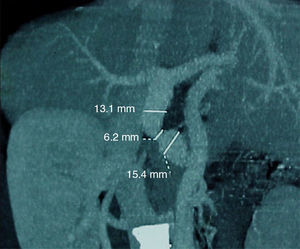
After transplant the patient progressed satisfactorily and she was discharged 13 days after the operation. On 23 July 2005 she relapsed with bleeding from varices in the fundus, so that several endoscopies were performed. The results of the endoscopy carried out on 21 December 2005 were: Westaby grade II oesophageal varices, GOV1 and GOV2 II gastric varices, one with a site of breakage, mild congestive gastropathy and from moderate to severe erosive antral gastritis, whole varices in the fundus and normal duodenum. Spleno-portal angio-CAT on 27 January 2006 showed an accumulation of varices from the gastric fundus, varicose collateral circulation, dystrophic calcifications, varices towards the lower third of the oesophagus, permeability of the right gastroepiploic anastomosis with the portal vein, an area of stenosis in 50% of this anastomosis, portal vein with flow to the right and left branches with delay towards the circulation of the suprahepatic veins, the upper mesenteric vein draining towards the varicose portion of the gastric fundus (Fig. 4). This was treated by application of liquid cyanoacrylate and lipiodol, sclerotherapies in the varices of the fundus and medication to reduce portal hypertension. The laboratory report on 10 February 2006 showed: haematic biometry, with 3200/ul leukocytes, haemoglobin: 9.7g/dl, 77000 platelets, prothrombin time of 14.3/13.3s, INR: 1.08, thromboplastin time (TPT) 28.2/32.3s, 76mg/dl glucose, creatinine 1mg/dl, BT 1mg/dl, BD 0.10mg/dl, BI at 0.90mg/dl, 47U/l ALT, 29U/l AST, 60U/l alkaline phosphatase, 4.4mmol/l potassium, 137mmol/l sodium and 477U/l lactic dehydrogenase.
DiscussionPortal vein cavernous degeneration is a relatively rare condition that is found in 3.2% of portal hypertension cases.20 Portal vein thrombosis is a complication in chronic liver disease that occurs in approximately from 5% to 15% of patients21. Several factors are associated with portal vein thrombosis, among which the following stand out: male sex, spontaneous portosystemic shunts, previous treatment for portal hypertension including endoscopic therapies, transjugular intrahepatic portosystemic shunts, surgical shunts, splenectomy, Chil-Pugh C liver involvement, alcoholic liver disease, recurrent episodes of encephalopathy, severe ascitis, Budd-Chiari syndrome, hypercoagulation states and cancer.5,22–26
Portal vein thrombosis is considered to be a relative contraindication in some hospitals27 in which similar results have been shown to arise over the long term between liver transplant patients with or without portal vein thrombosis.11–14 Until the end of 1980 portal vein thrombosis and splachnic vein thrombosis were considered contraindications for liver transplant due to concern about compromising portal perfusion. The first successful liver transplant in patients with portal vein thrombosis was reported by the Pittsburgh group in 1985, using a free iliac vein graft.28 Two year later they presented the first series of cases,29 after which several techniques have been suggested to resolve this situation.
Several classification systems have been proposed, of which Yerdel's classification is the most widely accepted and clinically used.5 Grades I and II of portal vein thrombosis are almost always managed by resection of the portal vein with or without thrombectomy; grades III and IV require more complex techniques. In the management of grades I and II the initial strategy is to remove the thrombus, eliminating the most internal layer of the vessel (thrombo-endovenectomy).5 If the thrombosis includes a short segment of the portal vein, this may be resected and the residual part of the thrombus may be affixed to the vessel wall.5
Rethrombosis of the portal vein has been reported in 28.5% of patients,23,29 and the percentage of mortality is 100%.5
In this case the patient presented complete thrombosis and cavernous transformation of the portal vein. As the right 2cm diameter gastroepiploic vein was found to drain into the infrarenal cava vein we took the decision to use it, with the probability of satisfactorily perfusing the liver graft, as in fact occurred. Although liver function remained normal, hepatofugal circulation persisted due to the occlusion of varicose vessels. We revised the medical literature and found no reports of portal perfusion with right gastroepiploic vein flow in liver transplant, so we present a relatively simple alternative when it is possible to perfuse the hepatic graft.
ConclusionsLiver transplant may be performed in cases of complete portal thrombosis and with cavernous degeneration of the portal vein. Several surgical procedures exist for portal perfusion, such as the technique used in this case, which was performed satisfactorily using the flow of the right gastroepiploic vein.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank doctors Ricardo Navarro López, Guadalupe Joseline Valadez González, Diego Enrique Acevedo Luna and Aida Rebeca Márquez Valdez for their help in the final revision of this paper and in editing the images.
Please cite this article as: Mendoza-Sánchez F, Javier-Haro F, Mendoza-Medina DF, González-Ojeda A, Cortés-Lares JA, Fuentes-Orozco C. Perfusión portal con flujo de la vena gastroepiploica derecha en trasplante hepático. Cir Cir. 2017;85:60–65.