Necrotising enterocolitis is the most frequent and severe acquired gastrointestinal disease in newborns and still has high mortality. There are few published papers about prognostic factors of death in our country.
ObjectiveTo know the factors associated with death in patients with necrotising enterocolitis.
Material and methodsRetrospective, descriptive, comparative study with a case–control design was conducted on patients with necrotising enterocolitis during a 5-year period.
ResultsDeceased patients had significantly lower platelet counts compared to survivors (p=0.022) and the prognostic factors associated with mortality were anaemia (p=0.006, OR=15.62), stage III of necrotising enterocolitis (p<0.001, OR=47.5), to require surgical treatment (p<0.001, OR=47.5), to have intestinal necrosis (p=0.001, OR=48.5) or perforation (p=0.016, OR=24.25), to have medical complications, specifically intravascular disseminated coagulation (p<0.001, RR=98), and multi-organ failure (p<0.001, RR=2). It was also found that patients with gastrointestinal symptoms and diagnosis of necrotising enterocolitis when they were hospitalized were more likely to have surgical treatment.
ConclusionsWe must be aware of the factors associated with mortality, as well as those associated with surgical treatment to reduce overall mortality for this condition.
La enterocolitis necrosante es la patología digestiva adquirida más frecuente y grave en el período neonatal con alta mortalidad. Existen pocos estudios en nuestro medio sobre factores pronóstico de muerte.
ObjetivoConocer los factores asociados a mortalidad en pacientes con enterocolitis necrosante.
Material y métodosEstudio retrospectivo, comparativo, tipo casos y controles de neonatos con enterocolitis necrosante durante un periodo de 5 años.
ResultadosLos pacientes fallecidos tuvieron significativamente menor cifra de plaquetas respecto a los sobrevivientes (p = 0.022), los factores asociados con significancia estadística a mortalidad fueron anaemia (p = 0.006, OR = 15.62), estadio III de la enfermedad (p = <0.001, OR = 47.5), requerir tratamiento quirúrgico (p = <0.001, OR = 47.5), tener necrosis (p = 0.001, OR = 48.5) o perforación intestinal (p = 0.016, OR = 24.25), padecer complicaciones médicas especialmente coagulación intravascular diseminada (p = <0.001, OR = 98) y falla orgánica múltiple (p = <0.001, RR = 2). Además se encontró que los pacientes con síntomas gastrointestinales y diagnóstico de enterocolitis necrosante al ingreso tuvieron asociación con tratamiento quirúrgico.
ConclusionesSe debe estar atento a los factores asociados a mortalidad; así como, los que se asocian a tratamiento quirúrgico, para en conjunto disminuir la tasa de mortalidad en esta entidad.
Necrotising enterocolitis is the most frequent and severe digestive disease acquired during the neonatal period. The mortality rate of necrotising enterocolitis varies depending on the population under study, although it is commonly associated with prematurity and low weight at birth. Medical care has enabled the survival of increasingly smaller patients, which has increased the incidence of necrotising enterocolitis; however, mortality has not changed.1
There are various studies in scientific bibliography dedicated to defining the risk factors associated with mortality in patients with necrotising enterocolitis: Kessler et al.2 found low gestational age, low weight at birth, and higher values of serum lactate associated with death. Fitzgibbons and his team3 reported a multi-centre study of over 500 hospitals and more than 70,000 patients with weights between 500 and 1500g, grouping them by weight into several categories, and found that higher weight at birth decreases mortality. However, Alexander and Smith4 reported the mortality of neonates with weight under 1500g, and they published that in this group of patients, regardless of gestational age, the factors associated with death were a long segment of intestinal necrosis and intestinal pan-necrosis.
Bonnard et al.5 reported that in a small series of patients high intra-abdominal pressure, evidenced by intravesical pressure, may be associated with mortality. This pressure increase, caused by the inflammatory response cascade, may lower the pressure of intestinal flow, triggering ischaemia, necrosis and intestinal perforations, which occur in 20–30% of patients in advanced stages, and comprise the most severe acute complications of this disease, increasing mortality between 20% and 40%. Gastrointestinal perforation is a clear indicator of surgery, but unfortunately there is no reliable or absolute marker for the imminence of a perforation. Usually, progressive abdominal distension, a palpable mass, clinical deterioration in spite of medical treatment, or the presence of a persistent fixed loop in successive X-rays may indicate intestinal necrosis and/or the imminence of perforation, and thus be an indication of surgical intervention.6
The surgical treatment of necrotising enterocolitis is restricted to neonates with ischaemia or intestinal necrosis and/or perforation, which ideally should be conducted when there is confirmed vascular deterioration of the intestine, but before there is perforation; however, this period often presents few symptoms.7
In our country, there are few bibliography reports regarding necrotising enterocolitis. In a series of 322 cases, Mancilla-Ramírez et al.8 reported an incidence of necrotising enterocolitis of 7.2% of those admitted to the neonatal intensive care unit (NICU), with a global mortality of 29.5%. Flores-Nava et al.9 reported a mortality of 29.4%. Piña-Ceballos et al.10 reported a mortality of 5% in a series of 20 patients, although neither of the three reports mentions any death-indicating factors. The only report addressing this issue is that of Rivera-Moreno et al.11, where factors associated with mortality were analysed in patients with necrotising enterocolitis stage III, with a mortality of 52%, reporting a state of shock and acute kidney failure as prognostic factors. Based on the above, there is a need to expand our knowledge of prognostic factors associated with mortality among neonates with necrotising enterocolitis in our environment, which has led us to conduct this study.
PurposeThe purpose is to know the prognostic factors of mortality among neonates with necrotising enterocolitis in our population, so as to help in prevention, timely diagnosis and adequate treatment of this disease.
Material and methodsA retrospective, descriptive, comparative study was designed, of a case–control type, between deceased patients (cases) and survivors (controls). Patients with necrotising enterocolitis diagnosis were included for a period of 5 years (1 June, 2008 until 31 May, 2013). Both the epidemiological variables and those pertaining to the disease and which might be related to death were analysed, such as: perinatal conditions, symptomatology, physical exploration, concomitant conditions, lab and clinical tests, stage of necrotising enterocolitis by means of Bell's modified classification, treatment, complications and evolution. Patients managed in other hospitals were not included, and those whose enterocolitis condition was not confirmed on reviewing the file or who had incomplete files were removed.
The following criteria were applied for lab tests: anaemia with a haemoglobin value below 12g/dl; leukopenia in patients of one day of age and with any value under 9400/μl, or, in patients with more than one day, with any value under 5000/μl; bandemia at any band value equal to or greater than 10%, and thrombocytopenia with any platelet level below 150,000/μl.
Statistical analysisCentral tendency measures, with average, were used for the epidemiological variables, as well as the median if the sample distribution was abnormal. Student's t test was used for the comparison of continuous variables, and Chi-square was used for nominal variables. The odds ratio (OR) of the variables associated with mortality were obtained, calculating the confidence interval (CI) at 95%.
ResultsDuring the studied period, 105 files of patients with necrotising enterocolitis were analysed, of whom 6 died and were defined as cases, and 99 survived and were defined as controls. The prevalence of enterocolitis was 9.2% of the total of admissions at the NICU during the study period.
Perinatal variablesOf the total, 59 were male and 46 were female, with a ratio of 1.2:1. The average gestational age was 35 weeks (24–42), with a median of 36. The average weight at birth was 2162.5g (580–3950). Upon admission, the range of ages was 1–63 days, with an average of 9.71 and a median of 5 days. According to Bell's modified classification, there were 31 stage I patients (29.5%), 66 stage II (62.9%) and 8 stage III (7.6%) patients.
It was found that 77 cases (73.3%) had received some kind of feeding prior to admission, predominantly breastfeeding, in 26 cases (33.7%), followed by specialised formulas in 19 (24.6%) and maternal milk in 16 (20.7%), among others.
The reason for admission was the enterocolitis in 25 patients (23.8%). In the other cases, this developed during the hospitalisation, after admission for other reasons such as respiratory and (31) infectious (14) issues, prematurity (7), neurological symptoms (6), cardiomyopathy (5) and surgical conditions (4), among others. Some concomitant conditions were found, possibly related to the necrotising enterocolitis, such as respiratory distress syndrome in 16 patients, perinatal asphyxiation in 8, low Apgar in 3, and apnoea in 2.
Clinical conditionsAt the time of diagnosis of necrotising enterocolitis, all patients presented one or more gastrointestinal symptoms, with predominance of abdominal distension in 84.8%, vomiting in 36.2%, abdominal pain in 31.4%, fixed loops in 23.8%, absence of peristalsis in 16.2%, stools with macroscopic blood in 11.4%, rejection to oral administration in 8.6%, absence of stools in 5.7%, and diarrhoea in 2.9%.
Laboratory and clinical testsAnaemia was found in 29 patients (27.6%), leukopenia in 7 (6.7%), bandemia in 13 (12.3%) and thrombocytopenia in 32 (30.5%).
All the patients had some abnormal radiological data, and many presented 2 or more. The most frequent were loop distension in 81 (77.1%), oedema of loop walls in 58 (55.2%), pneumatosis intestinalis in 30 (28.6%), intestinal occlusion in 9 (8.6%), portal pneumatosis in 8 (7.6%), ascites in 4 (3.8%) and pneumoperitoneum in 3 (2.9%).
TreatmentA total of 94 patients (89.5%) required medical treatment only (one of whom required diagnostic paracentesis) and 11 patients (10.4%) required surgical treatment; of them, 2 (1.9%) had penrose-type drains placed on their cribs (one survived and one died), and 9 (8.57%) required exploratory laparotomy, the findings of which are the following: 5 patients had necrosis, in 3 it was localised and in 2 it was generalised, or pan-necrosis, encompassing the whole small intestine and part of the colon; 4 of 5 had intestinal perforation; the 4 remaining patients initially had stage II with intestinal pneumatosis. They were managed with fasting for 10 days, but since the intestinal occlusion persisted they had surgery; in 2 patients symptoms were compatible with Hirschsprüng disease, so intestinal mapping and a colostomy were conducted; one had occlusive fibrous bands following the necrotising enterocolitis, requiring bridolisis, and the other, with gastroschisis history, had an associated intestinal atresia, requiring intestinal bypass.
Medical and surgical complicationsIt was determined that 22 patients (20.9%) presented medically relevant complications, some more than one. The most frequent were the following: 10 septic shock (9.5%), 8 respiratory complications (7.6%), 4 disseminated intravascular coagulation (3.8%), 3 neurological (2.8%), 3 multiple organ failure (2.8%), and 3 cases had infections in other places (one urosepsis, one sepsis related to the catheter, and one cellulitis of the abdominal wall).
Of the patients with surgery, there was disruption of the wound in 2 patients, enterocutaneous fistula in one with massive necrosis, and one presented an exit of intestinal loop through the penrose insertion point.
MortalityOf 105 analysed patients, 6 died (5.7%), with septic shock and/or multiple organ failure as cause of death.
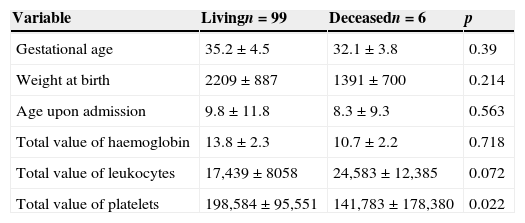
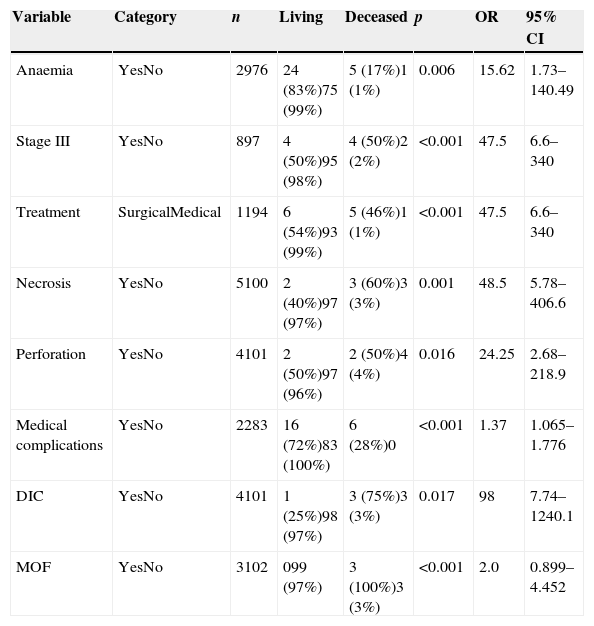
Analysis of mortality prognostic factorsIn the univariate analysis we found that, although the gestational age and the weight at birth were lower among deceased patients, and they had a lower value of haemoglobin and a higher value of leukocytes than the survivors, these differences did not have any statistical significance, only the platelet value was significantly lower among the deceased with regard to the survivors (Table 1). Upon associating qualitative variables to mortality, it was found that anaemia, stage III of the disease, the need for surgical treatment, the presence of necrosis or intestinal perforation, the fact of presenting medical complications, particularly disseminated intravascular coagulation and multiple organ failure, are the factors that significantly increase the risk of death (Table 2). The other analysed variables had no statistically significant association.
Comparison of quantitative variables between cases and controls.
| Variable | Livingn=99 | Deceasedn=6 | p |
|---|---|---|---|
| Gestational age | 35.2±4.5 | 32.1±3.8 | 0.39 |
| Weight at birth | 2209±887 | 1391±700 | 0.214 |
| Age upon admission | 9.8±11.8 | 8.3±9.3 | 0.563 |
| Total value of haemoglobin | 13.8±2.3 | 10.7±2.2 | 0.718 |
| Total value of leukocytes | 17,439±8058 | 24,583±12,385 | 0.072 |
| Total value of platelets | 198,584±95,551 | 141,783±178,380 | 0.022 |
Comparison of nominal variables with statistical significance between cases and controls.
| Variable | Category | n | Living | Deceased | p | OR | 95% CI |
|---|---|---|---|---|---|---|---|
| Anaemia | YesNo | 2976 | 24 (83%)75 (99%) | 5 (17%)1 (1%) | 0.006 | 15.62 | 1.73–140.49 |
| Stage III | YesNo | 897 | 4 (50%)95 (98%) | 4 (50%)2 (2%) | <0.001 | 47.5 | 6.6–340 |
| Treatment | SurgicalMedical | 1194 | 6 (54%)93 (99%) | 5 (46%)1 (1%) | <0.001 | 47.5 | 6.6–340 |
| Necrosis | YesNo | 5100 | 2 (40%)97 (97%) | 3 (60%)3 (3%) | 0.001 | 48.5 | 5.78–406.6 |
| Perforation | YesNo | 4101 | 2 (50%)97 (96%) | 2 (50%)4 (4%) | 0.016 | 24.25 | 2.68–218.9 |
| Medical complications | YesNo | 2283 | 16 (72%)83 (100%) | 6 (28%)0 | <0.001 | 1.37 | 1.065–1.776 |
| DIC | YesNo | 4101 | 1 (25%)98 (97%) | 3 (75%)3 (3%) | 0.017 | 98 | 7.74–1240.1 |
| MOF | YesNo | 3102 | 099 (97%) | 3 (100%)3 (3%) | <0.001 | 2.0 | 0.899–4.452 |
DIC: disseminated intravascular coagulation; MOF: multiple organ failure; 95% CI: 95% confidence interval; OR: odds ratio.
Lastly, given that several of the factors associated with mortality are related to surgical treatment, we conducted an analysis of all the variables as predictive factors for the need of surgery, and found that of all the continuous variables, only the total number of leukocytes was significantly higher among those who needed surgical treatment (24,172 vs 17,107; p≤0.001); the gestational age, the weight at birth, the haemoglobin and platelet values were lower among those who needed surgical treatment, but these differences did not reach statistical significance. As for the nominal variables associated with the need for surgery, we found a few that were also associated with mortality, such as stage III of the disease (p≤0.001), having medical complications (p≤0.001), or having disseminated intravascular coagulation (p=0.017); however, there were others that were not associated with mortality, such as having gastrointestinal symptoms (p=0.005) or the diagnosis of necrotising enterocolitis (p=0.021) as the reason for admission, and presenting pneumoperitoneum symptoms (p=0.001) or septic shock (p=0.017) during progress.
DiscussionDespite the progress of current medicine, necrotising enterocolitis still has a high prevalence in NICU; the rate we obtained of 9.2% is slightly higher than the 7.2% reported by Mancilla-Ramírez et al.,8 and it is still the most frequent and severe digestive disease acquired during the neonatal stage. Although bibliography states that approximately 90% of patients with necrotising enterocolitis are pre-term newborns, with gestational age between 30 and 32 weeks,12,13 in our study, the average gestational age of patients who had necrotising enterocolitis ranged around 35 weeks of gestation, thus confirming that prematurity is still an extremely important risk factor with regard to the occurrence of this disease.
In relation to feeding, it is known that exclusive breastfeeding lowers the incidence of necrotising enterocolitis, whereas the administration of formula increases it.14,15 In our study, most of the patients had received some kind of feeding, with the most frequent being the use of formula, thus confirming the association between the use of formula milk and the presence of necrotising enterocolitis. In centres of reference such as ours, the use of formula milk is very frequent due to the absence of maternal milk, since patients usually are neonates, but frequently also mothers who remain severely ill, so that there is no availability of maternal milk.
The concomitant disease that most frequently occurred in our population was respiratory distress syndrome and perinatal asphyxiation, which cause intestinal hypoxia and, consequently, a greater risk of necrotising enterocolitis.
At the time of prognosis, the most frequent signs and symptoms were abdominal distension, vomiting and abdominal pain, which matches the findings of Balanescu et al.,15 who reported that 50% of cases presented abdominal distension as the main symptom of necrotising enterocolitis, followed by gastric residue in 40% and vomiting in 28%; however, abdominal pain, which was the third most frequent sign in our series, is rarely reported, probably since they are neonates, but we are convinced that it is a sign which may be obtained with enough patience to examine the neonate. As for the lab findings, the most common reports are leukopenia and thrombocytopenia as referred by Méndez et al.16 in their 15-year retrospective study, where 38.3% had leukopenia and 13.9% had thrombocytopenia; in our study, we found a higher frequency of thrombocytopenia and a lower one of leukopenia; however, both symptoms are frequently associated with necrotising enterocolitis.
In relation to the prognostic factors of mortality, worldwide scientific bibliography commonly reports low weight at birth, prematurity, severity of symptoms, and intestinal perforation.2–4,17–19 Intestinal necrosis and intestinal perforation are surgical findings with major association with mortality.20,21 In our study, having stage III increased the risk of death by 47 times, having necrosis, 48 times, and, in the case of perforation, 24 times, which confirms these prognostic factors, and although the gestational age and weight at birth were lower in both cases, statistical significance was not reached, probably because a greater number of patients was required. Other factors described as associated with mortality reflect the severity of the condition, such as: sepsis, respiratory failure, disseminated intravascular coagulation, metabolic acidosis, shock state, hypotension, thrombocytopenia and ascites.19,22,23 We confirmed that having any medical complication, particularly disseminated intravascular coagulation and multiple organ failure, significantly increased mortality. Although according to our data, thrombocytopenia was not a risk factor, there was a statistically lower platelet value in deceased patients when compared to surviving patients.
In relation to other lab findings, the anaemia in our study was a factor related to mortality, since neonates with anaemia have a 15 times greater risk of death than those who do not have it, a previously unreported fact.
Finally, our patients needed surgery in 10.4% of all cases, which is a marked difference with reports of up to 40%.20,24 It is likely that our low rate of surgical treatment is due to awareness about the suspected disease in our unit, in the face of the first clinical signs.
Since the need for surgery is a factor that is related with others which are in turn associated with mortality, we analysed factors associated with the need for surgical treatment; thus the presence of pneumoperitoneum, which is widely accepted as an absolute indicator of surgical treatment and has been described in 50–75% of patients with necrotising enterocolitis, and which was confirmed in data of this study, others such as portal pneumatosis or ascites were not associated, which explains why the absence of radiological data does not rule out the need for surgery.21
The stage III showed significant association with the need for surgical treatment and with mortality, which is explained by the characteristics of this stage; however, in the sample other previously unreported factors were found in relation to the need for surgery, such as the fact of having been hospitalised due to gastrointestinal symptoms, or having been admitted with a necrotising enterocolitis diagnosis in relation to patients who were admitted with other diagnoses and later developed necrotising enterocolitis, all of which must alert the paediatric surgeon in the face of neonates admitted to the NICU with these symptoms. On the other hand, we must also heed the reports by García et al.,24 who state that once the neonatal period is over, patients with necrotising enterocolitis who require surgery are susceptible to late mortality, such as intestinal occlusion and cholestasis, which decrease life expectancy during the first year.
ConclusionsThe doctor proving care to newborns must pay greater attention to patients diagnosed with necrotising enterocolitis, particularly those with low weight, prematurity, anaemia, thrombocytopenia, and those who present medical complications, particularly disseminated intravascular coagulation and multiple organ failure, since these factors were associated with mortality in our environment. Furthermore, the paediatric surgeon managing these patients must pay attention, in addition to these factors, to others, such as septic shock, high value of leukocytes, gastrointestinal symptoms as the reason for admission or those patients who are admitted from the start with a necrotising enterocolitis diagnosis, since they may frequently have a need for surgical treatment during their progress. Necrosis or intestinal perforation, when among the surgical findings, are associated with greater mortality.
A greater sample size is required to confirm some associations which had no statistical significance; however, our results are useful in as much as they draw attention to the prognostic parameters of the disease, many of which may be corrected in time or compensated for to avoid a greater severity of the process, and thus have an impact on mortality.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Bracho-Blanchet E, Torrecilla-Navarrete ME, Zalles-Vidal C, Ibarra-Ríos D, Fernández-Portilla E, Dávila-Pérez R. Factores pronóstico para mortalidad en neonatos con enterocolitis necrosante. Cirugía y Cirujanos. 2015;83:286–291.