Face burns are a singular pathology with great functional and psychological impact in the patients suffering them. The ears play a fundamental role in personal interactions and damage to this organ results in physical and emotional distress. The reconstructive treatment of the burned ear is a challenge. Multiple procedures have been described to achieve success in the reconstruction of the burned ear; immediate reconstruction with autologous rib cartilage, secondary reconstruction, alloplastic material reconstruction, tissue expansion, skin grafts and also microvascular flaps are some of the most common procedures used in this patients. All these techniques focus on giving a natural appearance to the patient. Burns to the ears affect 30% of the patients with facial burns, they require an excellent treatment given by a multidisciplinary team.
Las quemaduras en la cara son una entidad con gran impacto funcional y psicológico debido a las secuelas que presentan los pacientes. Las orejas juegan un papel fundamental en la interacción de las personas y las lesiones de este componente anatómico se asocian a secuelas físicas y emocionales. El tratamiento reconstructivo de las quemaduras en orejas es un reto. Se tienen múltiples procedimientos para lograrlo, entre los que destacan: la reconstrucción inmediata con cartílago costal, la reconstrucción diferida, el uso de material sintético, el uso de expansores tisulares, el uso de injertos y el uso de colgajos libres. Todas estas técnicas van encaminadas a devolver una apariencia natural a la oreja quemada. Las quemaduras en orejas se presentan en un 30% de los pacientes con quemaduras faciales y requieren un excelente tratamiento por un equipo multidisciplinario.
Facial burns pose a medical challenge. Their physical and psychological sequelae require optimal and appropriate specialist medical care and precise reconstruction. The ears form part of the face and are of great aesthetic and functional importance.
The ears are vulnerable to burns due to their prominent location on the side of the head, the thin skin that covers them and their three-dimensional structure. For this reason, in 90% of patients with neck and facial burns the ears are involved, of whom 30% will have a lesion to the cartilage framework of the ear.1
Moreover, the thin skin that covers the cartilage framework of the ear is fragile and can be injured easily. In second or third degree burns, the cartilage of the ear is affected, either by direct damage or by secondary infections, which cause a deformity that requires correct reconstruction.2
The aim of this paper is to review the current concepts and principles of ear reconstruction in burns patients.
Classification of the burned earK’ung et al. created a simple classification to categorise patients with ear burns. The classification has 3 degrees depending on the most affected part of the ear3:
- •
Mild: loss of the helix and the upper part of the ear without extensive scarring to the skin around the ear.
- •
Moderate: the concha is normal in shape but is strongly adherent to the skin. There is involvement of the upper third of the ear, including the anterior and posterior crura, and considerable scarring around the ear.
- •
Severe: there are only remnants of the concha, and marked scarring to the soft tissue around the ear remnants. In very severe cases there can be stenosis of the external auditory meatus.
Ear burns must be attended from the moment the patient arrives at the emergency department. The aim of this paper is not to report how to care for a burns patient, but rather to highlight the most important details in the management of ear burns. On arrival at the emergency department, it must be ascertained whether or not the cartilage framework has been exposed. This is vitally important to prevent complications such as chondritis or cartilage necrosis.
Ibrahim proposes some principles for the care of ear burns, as follows4:
- •
Avoid pressure to the burned ear and bulky dressings in the first weeks.
- •
Debridement of eschar and crusts should be minimised.
- •
The hair around the ear should be shaved to reduce the risk of infection.
- •
Wash with soap twice daily.
- •
Always apply ointment with a bacteriostatic and bacteriocidal action.
There are many dressings, solutions, ointments and topical antibiotics that can be used on ear burns. Their use will depend on the degree of the burn. They can be divided into 2 major groups:
- -
Antiseptic agents: these are designed to limit (bacteriostatic) or eliminate (bacteriocidal) microorganisms in the burn. On arrival at the emergency department the area should be washed with antibacterial soap. Care should be taken when using chlorhexidine, because burns to the cornea have been reported, and povidone-iodine due to potential absorption in deep burns.5
- -
Antimicrobial agents: the therapeutic objective in first degree and superficial second degree burns is to keep the skin hydrated and to prevent infection. Lubricant ointments can be used for this purpose, and in cases where there is a risk of infection, silver sulfadiazine cream. The antimicrobial effect of silver is sufficient to prevent the development of infection. When used on the auricle, exposure to the sun should be avoided, because use of the cream on the face is associated with pigmentation of the skin.6
Mafenide acetate is a sulphonamide with excellent antibiotic properties, which also deeply penetrates eschar. These characteristics make it an ideal agent for the treatment of burns where there is exposure of the cartilage framework. It provides coverage against gram negative and Gram positive pathogens and has a mild antifungal action. It should be applied to eschar every 2h to ensure adequate penetration.7
The most frequent complications associated with the use of mafenide acetate are pain, local inflammation and allergic reactions. This drug acts as a carbonic anhydrase inhibitor, and therefore the patient should be monitored for hyperchloremic metabolic acidosis.8
Finally, hypochlorite solutions can be used routinely on facial and ear burns. Since first described by the British chemist Henry Dakin, this product has been demonstrated to have an excellent antimicrobial effect with no reports of toxicity or alteration of healing in concentrations of 0.025%. Care should be taken when used, since application of the product to healthy tissue has been associated with irritation and pruritus.9
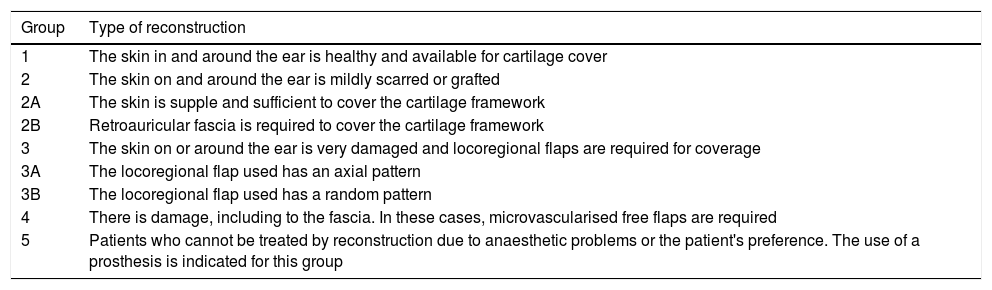
Post burn reconstruction of the auricleThe reconstruction of the burned ear poses a challenge for reconstructive surgeons. This is because the ear contains cartilage, subcutaneous cell tissue and thin skin, and the unusual shape of the ears is complicated to reconstruct. When a patient is assessed for reconstruction, any hearing problems should be evaluated. Furthermore, the degree of the burn must be assessed. In some cases the burn is only impeding some functional processes, such as wearing glasses, masks or earrings. In others, there is deformity or destruction of the ear and the surrounding tissue. Bandari created a classification for the detailed planning of auricle reconstruction in burns patients. The classification divides the patients according to the procedure used for reconstruction, from grafts to free flaps. Bandari's classification is shown in Table 1.1
Bandari's classification for reconstruction of the auricle after a burn.
| Group | Type of reconstruction |
|---|---|
| 1 | The skin in and around the ear is healthy and available for cartilage cover |
| 2 | The skin on and around the ear is mildly scarred or grafted |
| 2A | The skin is supple and sufficient to cover the cartilage framework |
| 2B | Retroauricular fascia is required to cover the cartilage framework |
| 3 | The skin on or around the ear is very damaged and locoregional flaps are required for coverage |
| 3A | The locoregional flap used has an axial pattern |
| 3B | The locoregional flap used has a random pattern |
| 4 | There is damage, including to the fascia. In these cases, microvascularised free flaps are required |
| 5 | Patients who cannot be treated by reconstruction due to anaesthetic problems or the patient's preference. The use of a prosthesis is indicated for this group |
Surrounding tissue of suitable quality is necessary reconstruction of a burned ear using local flaps. Small defects that involve less than one-third of the helix can be reconstructed with “pie slice” excisions or Antia-Buch flap. For major defects, flaps from the contralateral concha can be used. The lobe can be reconstructed from neighbouring tissue flaps, and in appropriate cases, concha and rib cartilage covered by a retroauricular advancement flap.
Major reconstructionTanzer was the first person to describe a treatment for burns patients in 1974: he resected all of the burned skin and placed partial thickness grafts for subsequent reconstruction with a sculpted costal cartilage framework. He described complicated dissection of the grafted skin, which limited appropriate reconstruction at a second stage.10 This prompted Edgerton to modify the technique. He made a flap from temporalis muscle fascia to cover the auricular prosthesis, made from porous polyethylene (medpore), with 65% exposure of the prosthesis. These first advances changed the conception of the reconstructive management of the burned ear.11 It was not until the end of the nineteen-eighties that Avelar reconstructed a burned ear, in a delayed fashion, using rib cartilage from the patient, with good results.12 It was then that the use of autologous material became popular (rib cartilage) for reconstruction in patients with burned ears. Simultaneously, there was an increase in the number of publications recommending the use of tissue expansion prior to placing the cartilage framework.13,14 In 1985 Brent published a series of patients with burned ears who underwent resection of the burned skin, placement of an autologous cartilage framework, temporo parietal fascial flap advancement and application of partial thickness grafts.15 Many authors perform modifications of this technique. The changes made by Nagata are noteworthy, which involve removing all the damaged cartilage tissue and using a mastoid fascia flap in some cases.16 These studies were the basis for immediate reconstruction in patients with ear burns.3 In a recent study, Medved measured the microcirculation in the burned ears of 6 patients. The authors concluded that oxygen saturation and blood flow in patients who underwent reconstruction using flaps supplied by the superficial temporal artery were more similar to that of a healthy ear.17 The use of free flaps is indicated in extreme cases. Radial flap and contralateral fascial flap have been described, unfortunately not with good results, due to the necessity for large venous grafts on the vascular anastomoses.18,19
Tissue expansion in burnsTissue expansion has been used in reconstructive surgery since 1957. It becomes an excellent option in burns, because it mobilises healthy tissue and provides functional and aesthetic improvement in sites with scarring. In the case of the ear, tissue expansion is used to cover the cartilage framework. It should only be considered if the scar is mature and in the mastoid or cheek area. The jaw region has high levels of exposure. The major disadvantage of expansion is that a second operation is required for removal of the expander and flap advancement. A silicone sheet has been suggested for use over the expander to reduce the risk of exposure.20
The use of synthetic implantsSilicone frameworks (Silastic) are no longer used due to their high complication rate. Used in burn patients, 70% of silicone frameworks suffer some degree of exposure.21 Therefore porous polyethylene (medpore) is the most used synthetic agent. This material is rigid, which provides good protection for the newly formed ear, but there is a risk of exposure, therefore attempts should be made to use locoregional flaps of healthy skin as coverage. The major advantage in using medpore is the reduction in morbidity when taking rib cartilage. However its main disadvantage is the exposure rate, which is greater than that of an autologous rib graft.22,23
The use of dermal substitutesThe advantages of dermal substitutes are: dressings are made easier, a reduction in costs and improved healing. These advantages are controversial. The products that have shown benefit for burns patients are:
Transcyte: a nylon mesh covered with synthetic collagen that is placed on the surface of the burn and promotes epithelialisation. It has been demonstrated to have advantages over other methods in facial burns.24
Alloderm: made from acellular cadaveric dermis and has also shown benefits in facial burns.25
Integra: a bi-layered product, containing a complex mesh of cross-linked collagen fibres. It is used in tangential excisions where there can be no immediate coverage with grafts.
Over the last ten years, there has been an increase in publications on tissue engineering. The objective of reconstructing a biocompatible cartilage framework must be to imitate a natural ear, and to reduce donor site morbidity. There are several things to take into consideration when recreating an ear. First a mould is required for appropriate cell planting (chondrocytes) which, in turn, can differentiate and therefore adapt appropriately to the receptor site. In vitro studies demonstrate that it takes at least 6 months for chondrocytes to cover a cartilage framework. The second problem is the costs associated with tissue bioengineering. Even in developed countries, differentiating and planting chondrocytes on a synthetic framework is very costly. Burns tend to present in people with medium to low incomes, and in public institutions with limited resources.26,27
Rehabilitation phaseAll patients with burned ears should be strictly monitored by a multidisciplinary team. Most patients with deep second degree or total thickness burns should use elastic pressure masks, which control the scarring process. These pressure masks should be used for at least one year, until the scarring process matures. Unfortunately the use of these adjuvants is not comfortable and most patients do not adhere to the treatment.28
Post burn careSilicone bands improve the appearance of scarring, softening the tissues. The mechanism of action is to occlude the scar and increase its hydration. Vitamins A and E have not been scientifically demonstrated to improve the healing process after a burn.29,30
ConclusionsBurns to the ears are common in facial burns and have major psychosocial and functional impact. Reconstructive treatment for these patients is a challenge and should be managed by a multidisciplinary team and a surgeon with experience in burns and ear reconstruction. There are many procedures from serial dressings to the use of free flaps, following the reconstructive ladder. Correct management, and the choice of the best reconstructive method, is required in the care of ear burn patients.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Carrillo-Córdova JR, Jiménez Murat Y, Apellaniz-Campo A, Bracho-Olvera H, Carrillo Esper R. Reconstrucción auricular en el paciente quemado. Cir Cir. 2017;85:454–458.