Fractures of the chest wall include sternum and rib fractures. Traditionally they are managed conservatively due to the anatomy of the rib cage that allows most of them to remain stable and to form a callus that unites the fractured segments. In spite of this management, some patients present with chronic pain or instability of the wall which makes them require some type of fixation. The present article performs a literature review based on 4 cases.
Clinical casesThe first case was a 61 year-old man with blunt chest trauma, with a great deformity of the chest wall associated with subcutaneous emphysema, and pneumothorax. The second case was a 51 year-old man with blunt chest trauma, initially managed at another institution, who despite treatment, had persistent pain and dyspnoea. The third case was a 30 year-old man that suffered a motor vehicle accident, with resulting pain and crepitation of the rib cage and with diagnostic images showing multiple rib fractures. The last case is a 62 year-old man that fell down the stairs, with blunt chest trauma with high intensity pain, dyspnoea and basal ipsilateral hypoventilation.
ConclusionRib fracture fixation offers a good alternative in selected patients to decrease associated morbidity, leading to a patient's fast return to his or her working life.
Las fracturas de la pared torácica, comprenden fracturas costales y del esternón. Tradicionalmente se manejan de manera expectante, debido a la anatomía de la reja costal, que permite que la mayoría permanezcan estables y formen callos óseos que unan los segmentos fracturados. A pesar de este manejo, algunos pacientes cursan con dolor crónico o inestabilidad de la pared, por lo que requieren algún tipo de fijación. El presente artículo hace una revisión del tema respecto a una serie de 4 casos.
Casos clínicosEl primer caso es un hombre de 61 años con trauma cerrado de tórax, con gran deformidad de la pared torácica, asociada a enfisema subcutáneo y neumotórax. El segundo caso es un hombre de 51 años con trauma cerrado de tórax, con manejo inicial en otra institución; pero en quien a pesar de esto persiste el dolor, y la sensación de disnea. El tercer caso es un hombre de 30 años quien sufre accidente de tránsito, con dolor, y crepitación de la reja costal, y con imágenes diagnósticas que muestran fracturas costales múltiples. El último caso es un hombre de 62 años que presenta caída por escaleras, con trauma cerrado de tórax con dolor de alta intensidad, y disnea; en quien se evidencia movimiento paradójico del tórax izquierdo e hipoventilación basal ipsilateral.
ConclusionesLa fijación de fracturas costales, ofrece en pacientes seleccionados una buena alternativa para disminuir la morbilidad asociada, y permitir al paciente su pronto retorno a su vida laboral.
The first open fracture reduction report belongs to the 1st century 1 AD and was performed by Soranus, according to Hurt.1 Later on, Paré described a method of handling rib fractures in which there was an attempt at closed reduction and then an open reduction if the first attempt failed2; that procedure became obsolete because it was not very effective. During the Second World War, doctors chose to remove rib fragments inside the lung,3 and today, open reductions and external fixation of ribs and sternal fractures are increasingly practised4 in selected cases, even implementing minimally invasive approaches.5
External traction has been initially described for handling sternal fractures,6,7 then wire and Russian internal thread fastenings were implemented in 1956.8 Later on, positive pressure with mechanical ventilation was implemented. This technique is still used, since it provides better handling and avoids respiratory failure, which is frequent in complex fractures.9
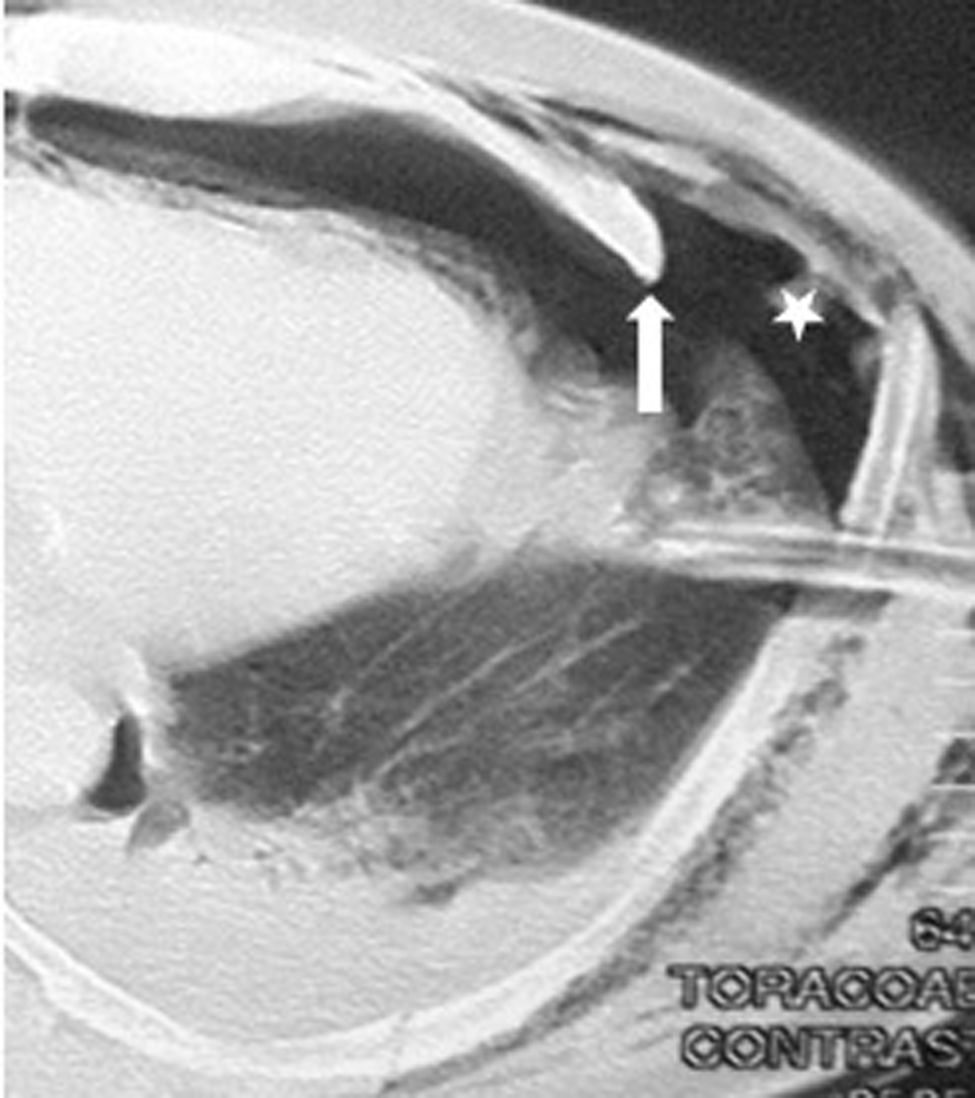
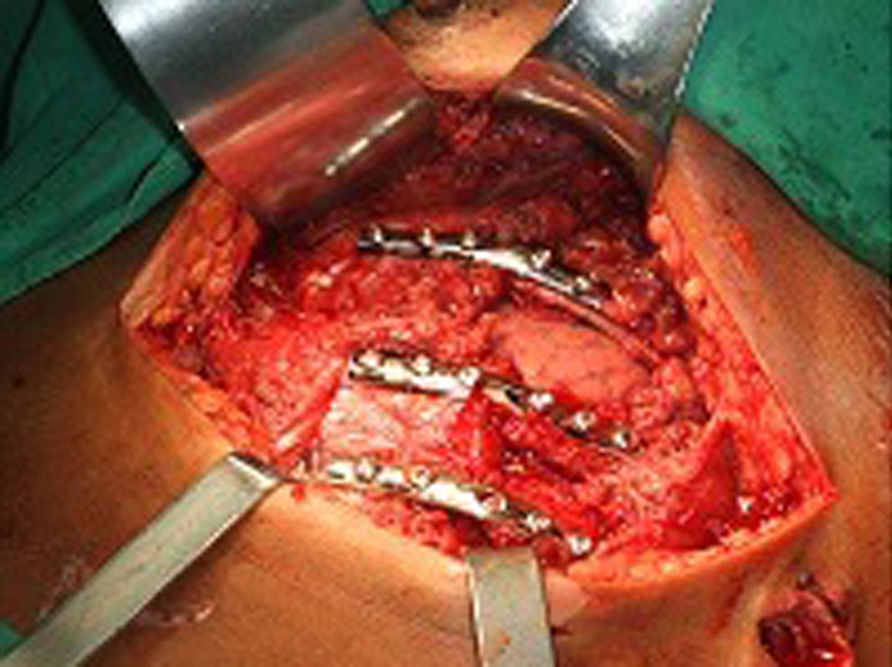
Clinical casesCase 161-Year-old male patient with a history of chest blunt trauma caused by being run over by a bull. He was transferred to an emergency department where he went into respiratory failure; he was intubated and needed mechanical ventilation. During the initial assessment, a large deformity was identified in his left anterior thoracic wall with unstable thorax associated with subcutaneous emphysema. The chest X-ray registered a left-sided pneumothorax, so a left-sided closed thoracotomy was performed and the patient was transferred to the intensive care unit. At this point, a chest computerised axial tomography scan was ordered, which evidenced multiple displaced left rib fractures and pneumothorax (Fig. 1). With these findings, a cross-consultation with thoracic surgeons was made, who considered that the patient was a candidate for rib osteosynthesis with an 8-hole, one-third tubular osteosynthesis plate with bicortical screws. This procedure was carried out without complications, and watertight closure was used after surgery (Fig. 2).
The patient was extubated six days after surgery and discharged 14 days after surgery, without complications. He returned to work 30 days after the trauma. There was no pulmonary function follow-up since the patient was lost.
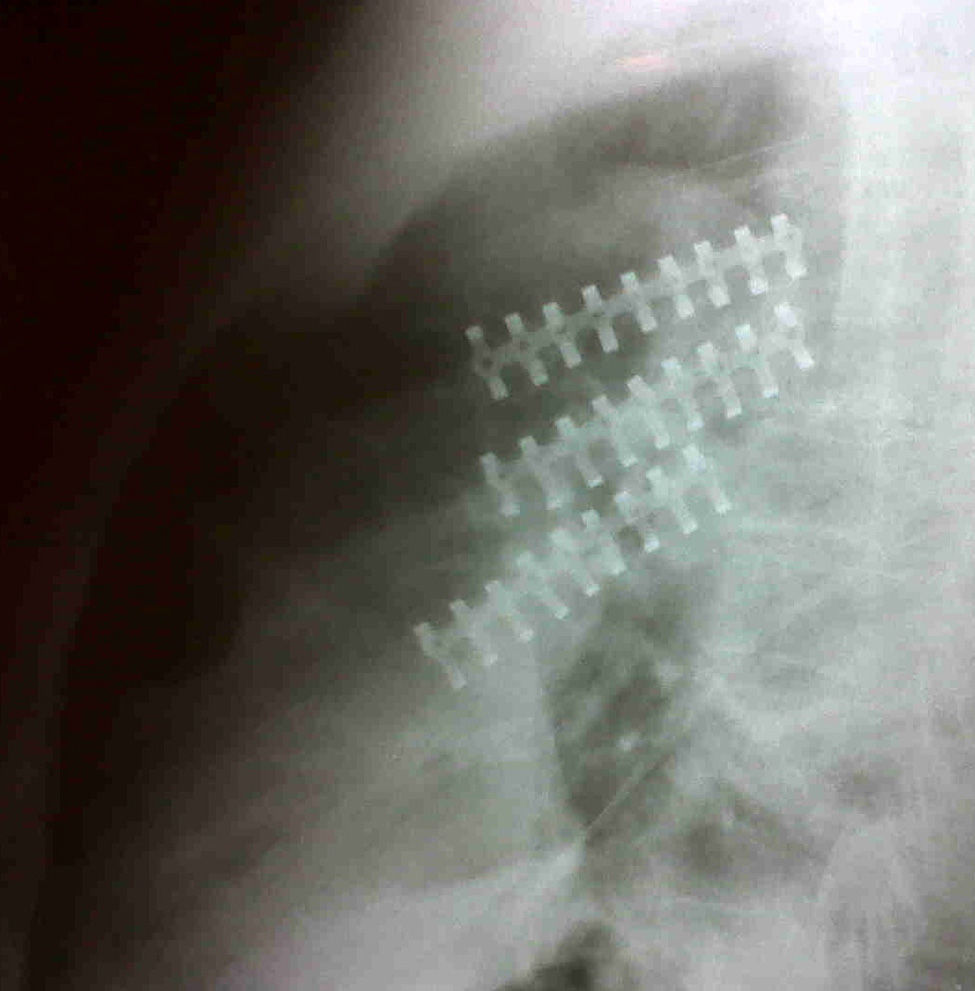
Case 251-Year-old patient who underwent a closed trauma in his left hemithorax after being hit by a bull. He received initial treatment at a rural hospital, but since the pain in his left hemithorax and a sensation of dyspnoea persisted, he was referred to our institution. During physical examination there was no evidence of paradoxical respiration or subcutaneous emphysema, or hypoventilation or abnormal lung sounds. A computerised chest tomography scan was conducted, which showed displaced fracture of three left ribs with haemothorax. Based on the clinical and tomographic findings, he underwent rib osteosynthesis using the STRACOS system® and watertight closure after surgery without complications. He returned to work 20 days after the trauma. There was no pulmonary function follow-up since the patient was lost (Figs. 3 and 4).
30-Year-old male patient who suffered a traffic accident riding a motorcycle; he was the driver. He had an abdominal closed trauma, severe head injury with loss of consciousness and facial fractures. During physical examination, he evidenced a reduction of respiratory sounds in lung bases, with no abnormal lung sounds, pain and crepitation on palpation of the anterior upper left rib cage. Abdomen showed no muscular guarding. A computerised chest tomography scan was performed, where a pulmonary contusion in the lower left lobe was evidenced, with rib fractures from the second to the seventh rib on his left side; the third and fourth ribs were fractured in three fragments. He received orotracheal intubation to handle his airways due to his facial fractures and due to the evidence of unstable thorax, with paradoxical respiration in the fractured segment of the rib. For this reason, we performed osteosynthesis of his rib cage using the MATRIX RIB® system with 10-hole precast plates and bicortical blocking screws, with watertight closure after surgery, without complications. The patient was extubated 15 days after surgery but due to his head injury he could not return to work. There was no pulmonary function follow-up since the patient was lost (Fig. 5 for case 3 and Fig. 6 for cases 4, 5 and 6).
62-Year-old male patient, who after consuming alcohol fell down a winding staircase, from the second to the first storey of his house. He suffered closed trauma in his left hemithorax, with subsequent acute pain, dyspnoea and diaphoresis, which was the reason he consulted at our institution. During physical examination, paradoxical motion of the left thorax was confirmed between the fourth and seventh intercostal space, with subcutaneous emphysema in posterior region and baseline ipsilateral hypoventilation; he was taken to an operating theatre with an unstable thorax diagnosis to receive osteosynthesis in the affected ribs, using the MATRIX RIB® system with 10-hole precast plates and bicortical blocking screws, with watertight closure after surgery and no postsurgical complications. This patient was discharged five days after the day of admission and returned to his everyday life 20 days after the trauma. There was no pulmonary function follow-up since the patient was lost.
DiscussionIndications for osteosynthesisUnstable thoraxUnstable thorax is defined as the existence of four or more unilateral and adjoining fractured ribs in two or more places, causing a paradoxical motion when breathing.
An unstable sternum occurs when the sternum is dissociated during the respiratory motion due to multiple bilateral anterior fractures of the ribs.10
Patients with unstable thorax treated with internal fixation (surgical) recover faster and therefore can return to their everyday life activities quicker, since they need fewer days on mechanical ventilation. Their stay at the intensive care unit is shorter, with a lower pneumonia incidence and improvement of their pulmonary function within the first month after the surgical fixation, compared to patients who did not receive a fixation.11,12
Expectant management of an unstable thorax has been the standard treatment for a long time. However, it does not provide the best results. In a retrospective study in which 62 patients with unstable thorax were analysed and who carried out a 5-year follow-up,13 only 43% returned to the job they had prior to the unstable thorax diagnosis, even though the pulmonary function only decreased in a very low percentage.
Deformity of the thoracic wallThis refers to the deformity caused by a high-impact or high-energy trauma, which generates bone and soft tissue involvement, which requires debridement and/or extraction of fragments, and if it is treated correctly would result in a lung hernia.14 This situation can be treated by removing the bone fragments from a chip fracture and then covering the defect with a rotational muscular flap or placing a synthetic mesh, as well as performing osteosynthesis with titanium plates that reduce the need to cover large hernia defects.15
Severe pain and reduction impossibilityMost of the patients with rib fractures accomplish the sealing of the defect without the need of reductions. However, prospective non-randomised studies report that the symptomatology could persist for up to 30 days after the rib trauma in some patients. Therefore, they need more time to recover and more days off work, which impacts their quality of life,16 which diverges from the results observed in patients who undergo surgical reduction of their costal arches.
Non-fusionA small group of patients do not undergo consolidation of the fractures in spite of the formation of a bone callus and so do not attain thorax stabilisation and are left with a defective sequela, which causes chronic pain and discomfort when breathing and can last months or even years after the fracture. The logic of the recuperation of the non-fused defect is based on the presumption that, without surgical intervention, that segment will never heal and therefore, the symptoms will prevail.12
Thoracotomy for other indicationsThoracotomy also has different indications from rib traumas with multiple rib fractures or with an unstable thorax. For example, in cases of pulmonary laceration, retained haemothorax or diaphragm laceration, and in cases of tumour removal since they are also candidates for the surgical repair of rib fractures.17,18
Technical aspects of rib fracture repairThe anatomy of ribs is very variable, both among separate ribs and in the proportions that form them. Therefore, fractures tend to be chip fractures and do not follow a linear pattern. Also, a fracture near the anterior rib pole will be different from a posterior rib fracture.
Ribs have different geometries in each spatial axis, so they have an overall curvature, a rolled curvature and a longitudinal twisting. The rib surface is twisted and conical when they curve, which makes the fixation plates used to fix long bones differ as their overall curvature increases.19 For this reason, plates especially designed for each rib have to be used to fix them, and they have to be made of a material that is flexible to avoid breakage or shifting of the Plate.20 In addition, the fact that the neurovascular bundle is placed on the inferior margin makes the patient prone to post-thoracotomy syndrome if the intercostal nerve becomes sore or is injured when fixing a fracture.21
Various devices and techniques have been described to fix ribs: wire sutures, intramedullary wires, staples, and plates made of several metals or absorbable materials, and there are even descriptions of minimally invasive techniques to handle rib fractures.10
Anterior plates and cerclage wiringThese are steel plates that are flat, malleable and are fixed towards the anterior pole of the rib fracture on the anterior cortical of the injured arch. They are fixed surrounding the rib using cerclage wiring, which is why they can cause injuries due to the compression of the neurovascular bundle that could be associated with the shifting of the Plate.22
Anterior plates with screw fixationThese create a fixing of the fracture with dynamic compression generated by the screws, which allows stability both during rest and during motion and inhibits plate rotation and shifting. They are specially designed for the geometry of each group of rib arches and require perforation of the cortical to apply the screws. With this system, the risk of compressing the intercostal nerve can be avoided.23
Intramedullary fixingThis involves inserting a wire or a steel or titanium plate into the rib's marrow, fixing its distal cortical. It is usually indicated in posterior rib fractures due to complex access. The main complication of this method is the dislodging of the osteosynthesis device, which can even pierce the total density of the rib and cause injuries in nearby structures, such as the pulmonary parenchyma or the skin.24 Another associated complication is the rotation of the rib on its longitudinal axis.25
Flexible staplesThese are devices in the shape of staples that are placed on the anterior surface of the rib. In addition, they have flexible sheets that surround the rib on each side of the fracture, imparting stability to the structure. The advantage is that they do not require screws or perforation of the bone, which makes removal easy, but it is highly likely they could compress the intercostal nerve.26
U-shape platesThis is a device that combines the different systems for rib fixing. It involves flexible sheets that hold the rib in the superior margin such that compression of the intercostal nerve is avoided. They are fixed on the anterior surface using screws with fixing Plates.27
Absorbable platesThese are devices made of absorbable materials, such as polylactide and polydioxanone, which are frequently used in maxillofacial or long bone fractures. They are less rigid than titanium plates and do not need to be removed.28 The risk of non-healing due to stress has been described; it is associated with excessively rigid devices. As of today, there are no trials to show that healing is quicker with absorbable-material fixing.29
Preoperative preparation and approachesOnce the rib fractures or unstable thorax has been identified, a tomography scan of the rib cage with 3D reconstruction should be conducted, which allows determination of the exact location of the defects to be treated in a precise manner and enables a better approach. In general, the conventional thoracotomy incision provides an adequate exposure of the rib cage, and it is also possible to perform a videothoracoscopy to remove the bone fragments and/or to accurately locate the segment with the fracture, and then perform a smaller incision that involves less injury to muscles.30
ComplicationsThe main complications linked to the repair of rib fractures are: (1) those associated with surgical wounds, whether they are infections (1.2%), seromas (0.6%), pleural empyemas (0.3%), haematomas of the surgical wound, or persistent pleural effusions; (2) those associated with rib fixing, which could be the shifting of the plate (1.2%), rib perforation by the intramedullary fixing device with or without injury to nearby structures, persistent pain that prompts the removal of the prosthetic material (1.4%), and rib osteomyelitis.11
ConclusionsThe fixing of rib fractures, in spite of being a rarely used technique, constitutes a good alternative in selected patients to reduce associated morbidity, allowing the patient to be discharged earlier, allowing lung ventilation in acute cases until the patient can return to work thanks to effective healing of the ribs, which would not be possible by implementing traditional management in most cases. For this reason, getting used to the techniques and devices used for open reduction and rib fixing broadens the therapeutic repertoire of a surgeon and can provide better alternatives for the patients who need them.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Jiménez-Quijano A, Varón-Cotés JC, García-Herreros-Hellal LG, Espinosa-Moya B, Rivero-Rapalino O, Salazar-Marulanda M. Osteosintesis de reja costal. Revisión de la bibliografía y reporte de casos. Cir Cir. 2015;83:339–344.