Even in expert hands, there can be serious complications when performing an endoscopic retrograde cholangiopancreatography. The most frequent complications are pancreatitis, cholangitis, bleeding, perforation, and acute cholecystitis. The hepatic subcapsular haematoma is a rare complication, with few cases described worldwide.
ObjectiveA case is presented of an extremely rare complication of endoscopic retrograde cholangiopancreatography, which required surgical treatment for its resolution without success. This is second case of mortality reported in the literature.
Clinical caseFemale patient of 30 years old, with indication for endoscopic retrograde cholangiopancreatography due to benign strictures. A hydro-pneumatic dilation and stent placement of 2 gauge 10Fr was performed. She presented abdominal pain after the procedure and significant decline in haemoglobin with no evidence of haemodynamic instability so an abdominal tomography scan was performed, showing no evidence of liver injury. The patient was haemodynamic unstable within 72h. A laparotomy was required for damage control, with fatal outcome in the intensive care unit due to multiple organ failure.
ConclusionSubcapsular hepatic haematoma after endoscopic retrograde cholangiopancreatography is a rare complication, with few cases reported in the literature. Treatment described in the literature is conservative, resulting in a satisfactory resolution.
Durante una colangiopancreatografía retrógrada endoscópica, incluso cuando es realizada por manos expertas, se pueden presentar complicaciones muy serias, las más frecuentes son: la pancreatitis aguda, colangitis, hemorragia, perforación y colecistitis aguda. El hematoma hepático subcapsular es una complicación rara, con pocos casos reportados en la bibliografía médica.
ObjetivoPresentar un caso de complicación extremadamente rara de colangiopancreatografía retrógrada endoscópica, en el cual se requiere de tratamiento quirúrgico para la resolución de esta complicación, siendo este el segundo caso reportado en la literatura con mortalidad.
Caso clínicoPaciente femenina de 30 años de edad, con indicación para colangiopancreatografía retrógrada endoscópica por estenosis benigna, con realización de dilatación hidroneumática y colocación de 2 stents calibre 10 fr. Presentó dolor abdominal posterior al procedimiento con descenso importante de hemoglobina, sin datos de inestabilidad hemodinámica, por lo que se le realiza tomografía axial abdominal que no evidencia lesión hepatica; a las 72 h presenta inestabilidad hemodinámica, por lo que requirió laparotomía exploradora, realizándose control de daños, con desenlace fatal en la unidad de cuidados intensivos por falla orgánica múltiple.
ConclusiónEl hematoma subcapsular hepático posterior a la realización de colangiopancreatografía retrógrada endoscópica es una complicación rara, con pocos casos reportados en la bibliografía mundial. Su tratamiento en la bibliografía mundial es conservador, con resolución satisfactoria posterior al mismo.
Endoscopic retrograde cholangiopancreatography was first performed in 1968 to visualise the biliary tree and further developed into endoscopic retrograde sphincterotomy and its variants from 1974.1 Even in expert hands there can be serious complications when performing an endoscopic retrograde cholangiopancreatography. These occur in 2.5–8% of cases, with a mortality rate of between 0.5% and 1%.2 The most frequent complications include: acute pancreatitis (1–7%), cholangitis (1.4%), bleeding (1%), perforation (1%) and acute cholecystitis (0.2%).3
Hepatic subcapsular haematoma is a rare complication of endoscopic retrograde cholangiopancreatography, with few cases described worldwide.4–6
Our case study is of a patient who presented with a single symptom of abdominal pain, with no evidence of hepatic subcapsular haematoma from the abdominal scan after endoscopic retrograde cholangiopancreatography. Despite surgery, the outcome of the acute abdomen was fatal.
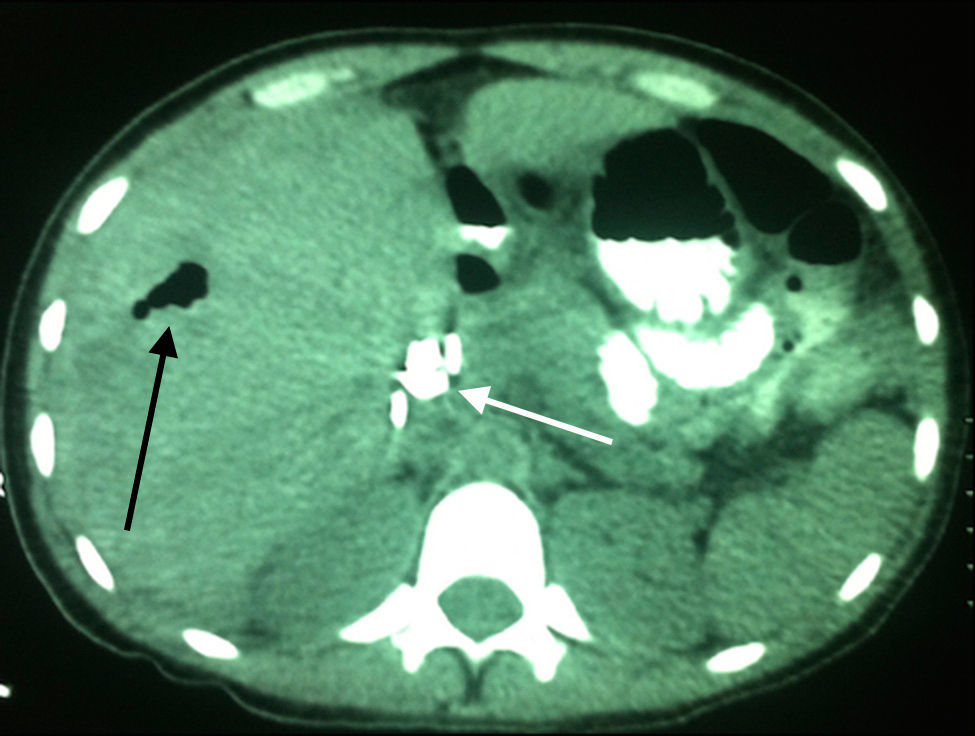
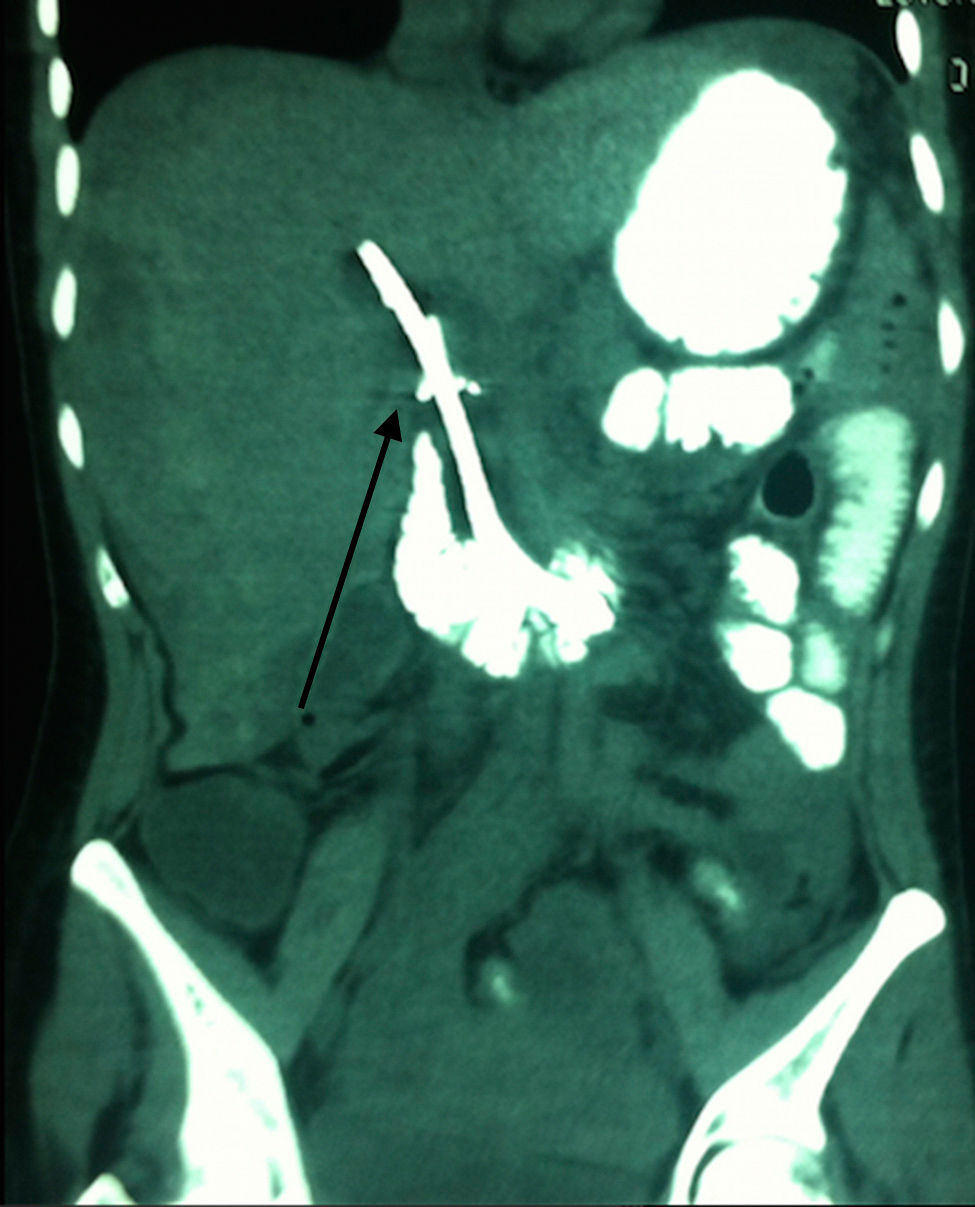
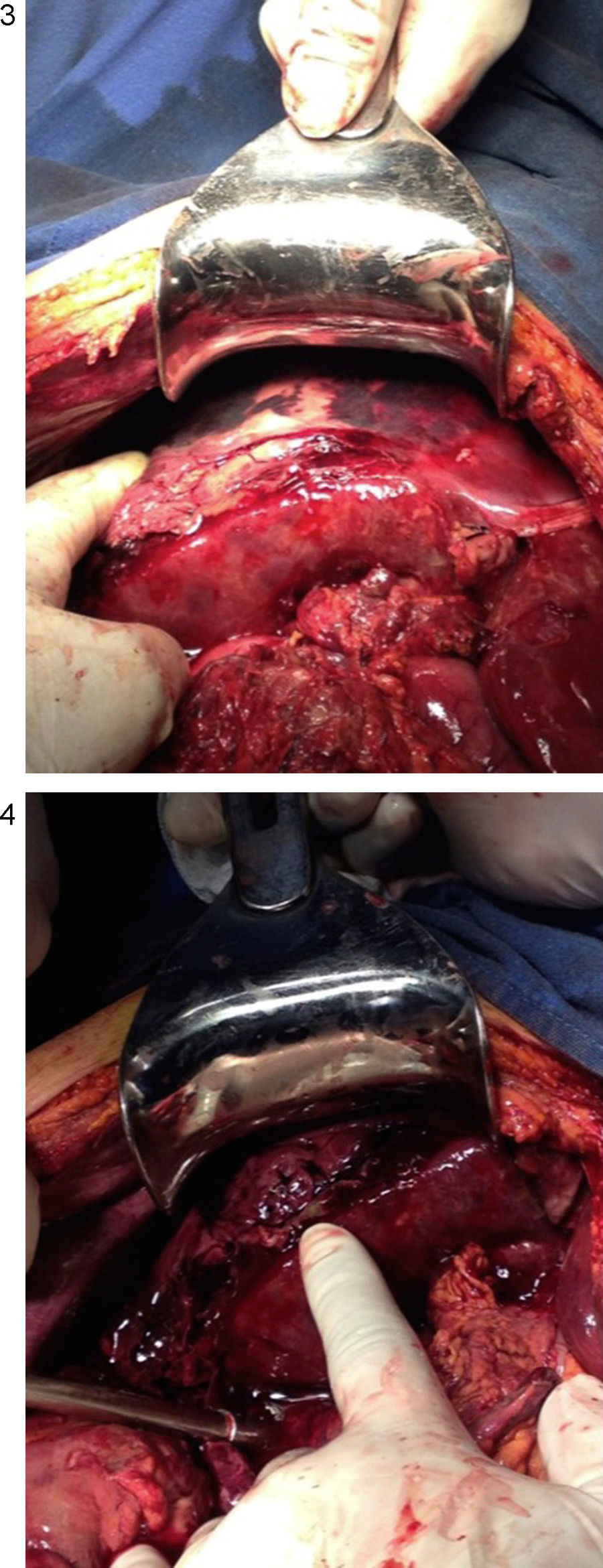
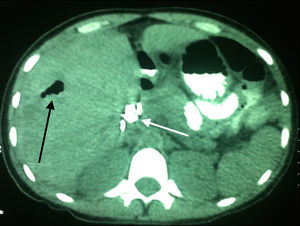
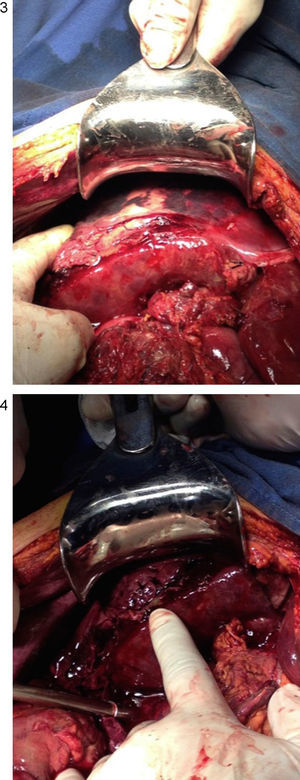
Clinical caseA 30 year old female with a history of laparoscopic cholecystecomy who was jaundiced 2 weeks after surgery, was diagnosed with benign stenosis of the common bile duct. She was assessed by the Endoscopy Unit, where mechanical dilation of the common bile duct was indicated, together with biliary sphincterotomy and insertion of a 10Fr calibre biliary prostheses. She was referred for a second session, where a hydro-pneumatic dilation was performed and 2 10Fr stents were implanted. The patient presented with abdominal pain after the procedure and was admitted to the general surgery unit for examination. A history of abdominal trauma was investigated but did not exist. Prior endoscopic retrograde cholangiopancreatography studies showed no signs of concomitant disease, nor any background of chronic or degenerative disease. Conservative treatment was initiated with the placement of a nasogastric probe, fasting and rehydration. Haematic biometry was indicated with a recorded haemoglobin concentration of 7.1g/dl; there were no clinical signs of peritoneal irritation or haemodynamic imbalance. Amylase values were at normal levels, and acute pancreatic procedure was rejected. An abdominal CT scan was indicated, which showed no signs of retroperitoneal air or liver damage (Figs. 1 and 2). During her stay at hospital the patient presented with mild abdominal pain, and was haemodynamic stable; a control abdominal CT scan was performed after 72h. The patient was haemodynamic unstable at 72h after the endoscopic retrograde cholangiopancreatography, and there was indication of an acute abdomen. We decided to perform an emergency exploratory laparotomy, with transoperative findings which included: 20,000ml foetid haemoperitoneium, with no evidence of intestinal material, indiscriminate ischaemia, ascending and sigmoid colons, with no signs of duodenal perforation, liver with broken subcapsular haematoma which involved the right lobe parenchyma (Figs. 3 and 4), and blood flow in the right liver lobe. Damage control surgery and immobilisation of the patient was performed. In the intensive care unit the patient presented with hypovolemic shock, the outcome of which was fatal, despite advanced resuscitation manoeuvres immediately following surgery.
Contrast enhanced axial CT scan of the abdomen, with no presence of liver damage. Air in the intrahepatic biliary duct is observed (a common occurrence after endoscopic retrograde cholangiopancreatography) and the presence of stents in the extrahepatic biliary duct (black and white arrows respectively).
Hepatic subcapsular haematoma after endoscopic retrograde cholangiopancreatography is a rare complication, with few cases reported worldwide. It may be explained by an accidental puncture of the intrahepatic biliary tree by a metallic probe and rupture of an intrahepatic vessel.2 The use of conservative treatment has been reported, with strict surveillance of haemodynamic status and satisfactory outcome following the same.2,5,7–18 Surgical treatment is reserved for those cases where there is haemodynamic instability despite the conservative treatment.3 We present a case where abdominal pain was present after endoscopic retrograde cholangiopancreatography and was the only symptom; a study/examination protocol was initiated after ruling out secondary aetiology to the said procedure, with a ruling out of abdominal trauma, acute pancreatitis or concomitant diseases, with the observation of a sharp fall in haemoglobin, with haemodynamic stability. Despite being a complication with few reported cases worldwide, when there is a sharp decline in haemoglobin and haematocrit this possible complication should be suspected, and is sufficient reason to perform an abdominal CT scan.1–3 When haemoglobin levels fell, an abdominal CT scan was requested 24h after the endoscopic retrograde cholangiopancreatography but there was no imaging evidence of subcapsular haematoma and the patient was haemodynamically stable, with no sign of peritoneal irritation. As there were no signs of alarm and no signs of late subcapsular haematoma, conservative treatment was resumed, and a later subcapsular hepatic haematoma presented, with spontaneous rupture, the appearance of peritoneal irritation and haemodynamic instability. As has been reported in worldwide literature, surgical treatment in these cases is reserved for patients who present with deterioration regardless of the conservative treatment,1–3,5,7–18 although there may be no signs of this in the CT imaging; conservative treatment is insufficient, when haemodynamic instability presents. Emergency treatment was therefore performed, with the observation of a ruptured hepatic subcapsular haematoma, control of damage and subsequent fatal outcome, despite emergency surgery.
ConclusionsThe importance of this report lies in the presentation of a probably under diagnosed entity which, although infrequent, should be taken in to account regarding possible posterior complications to endoscopic retrograde cholangiopancreatography, and in the description of its development and surgical treatment. This is second case of mortality reported in medical references3.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: González-López R, García-Cano E, Espinosa-González O, Cruz-Salgado Á, Montiel-Jarquin Á-J, Hernández-Zamora V. Tratamiento quirúrgico para hematoma subcapsular hepático posterior a colangiografía retrógrada endoscópica; caso inusual. Cir Cir. 2015;83:506–509.