Continuous perineural infusion of local anaesthetic provides better postoperative analgesia than intravenous administration of opioids or NSAIDs in upper limb surgery. The infraclavicular approach is a good option, due to the muscular stability to catheter; the abduction of the arm apparently makes the brachial plexus more superficial and which elevates the clavicle in the cephalic direction.
ObjectiveThe aim of this study was to identify whether the abduction of the arm decreases the skin-plexus distance, making the perineural insertion of the catheter easier and for a better analgesia. This relationship between the arm and the insertion of catheter has not yet been established.
Material and methodsThe study included 58 adult patients, undergoing forearm and hand surgery, initially divided into two groups, adduction and abduction. Ultrasound-guided infraclavicular block was performed, enabling the catheter tip to be positioned adjacent to the posterior cord. The group of patients with high technical difficulties were allowed to reposition the arm abduction. A record was made of the number of punctures, redirects, ease of insertion of the catheter, and skin-plexus distance.
ResultsThe abduction of the arm moved the clavicle towards the cephalad and separated it from the linear transducer, this allowed to manoeuvre the needle right angle and redirect it. The skin-plexus distance did not decrease significantly with arm position.
ConclusionsArm abduction allows better scanning, facilitates the infraclavicular puncture, and catheter introduction.
La infusión perineural de anestésico local brinda mejor analgesia postoperatoria que la administración por vía intravenosa de opioides o antiinflamatorios en cirugía del miembro superior. Para colocar un catéter en el plexo braquial, el abordaje adecuado es el infraclavicular debido a que ofrece mayor estabilidad muscular. La abducción del brazo aparentemente coloca al plexo braquial más superficial, y que eleva en sentido cefálico la clavícula.
ObjetivoEl objetivo de este trabajo es identificar si la abducción disminuye la distancia piel-cordón y facilita el procedimiento de introducción del catéter por ultrasonido, asegurando una analgesia óptima. Esta posición del brazo y su relación con la colocación del catéter no se habían descrito anteriormente.
Material y métodosSe incluyó a 58 pacientes adultos, sometidos a cirugía de antebrazo y mano, divididos en 2 grupos por colocación de la extremidad en abducción y aducción, se realizó un bloqueo infraclavicular mediante ecografía, colocando la punta del catéter adyacente al cordón posterior. En los pacientes del grupo en aducción con dificultad técnica elevada se permitió cambiar el brazo a abducción. Se registraron el número de punciones y de redirecciones, la facilidad de introducción del catéter y la distancia piel-plexo.
ResultadosLa abducción del brazo desplazó cefálicamente la clavícula y la separó del transductor lineal, lo que permitió maniobrar la aguja en su angulación y redirección correcta, la distancia plexo a piel no disminuyó de manera significativa con la posición del brazo.
ConclusionesLa abducción del brazo permite un mejor rastreo en los bloqueos supraclaviculares guiados por ultrasonido y facilita la punción infraclavicular con la introducción del catéter.
The approach of the brachial plexus via infraclavicular with perineural administration of local anaesthesia during surgery of the upper limb offers better analgesia by covering the entire upper limb, including the musculocutaneous nerve area, compared to the axillary or interscalene approach1,2. The catheter placed in this site has stability and resistance to traction thanks to the mechanical stability that the pectoralis major and minor muscles exert3,4. Previous studies informed that the infraclavicular block can be made through neurostimulation and other localization techniques, where differences between effectiveness and latency time5,6 were informed. The coracoid technique provides the most safety regarding pulmonary complications and allows for efficient placement of the catheter tip at the same level of the brachial plexus cords7,8. Nowadays, it has been demonstrated that the success rate is higher when the perineural catheter is placed using ultrasound guidance9–13, and the single injection around the posterior cord is as efficient as the multiple injection technique14. It was also observed that the abduction of the arm raises the brachial plexus to the surface15,16. In order to ensure better analgesia, the catheter tip should reach the perineural sheath next to the posterior cord17–19, as the axillary artery acts as a barrier for the diffusion of the local anaesthetic between the medial and lateral cords20. If the brachial plexus can be located in a more superficial way by abduction, the catheter will more easily reach it, thereby increasing the success rate.
The aim of this study was to identify if the position of the arm facilitates the insertion and placement of the infraclavicular catheter using ultrasound scan. Although this approach is the most used in brachial plexus, this important technical detail for continuous procedures had not been previously explained.
Material and methodsAn observational and clinical study was conducted, prior written informed consent form, of 58 adult patients classified as I-III according to the classification of the American Society of Anesthesiologists (ASA), scheduled for surgery of upper limb, forearm or hand.
Patients with a body mass index >35, kidney disease or renal failure, a history of neuropathies, ASA >IV, dementia and severe coagulation alterations were excluded.
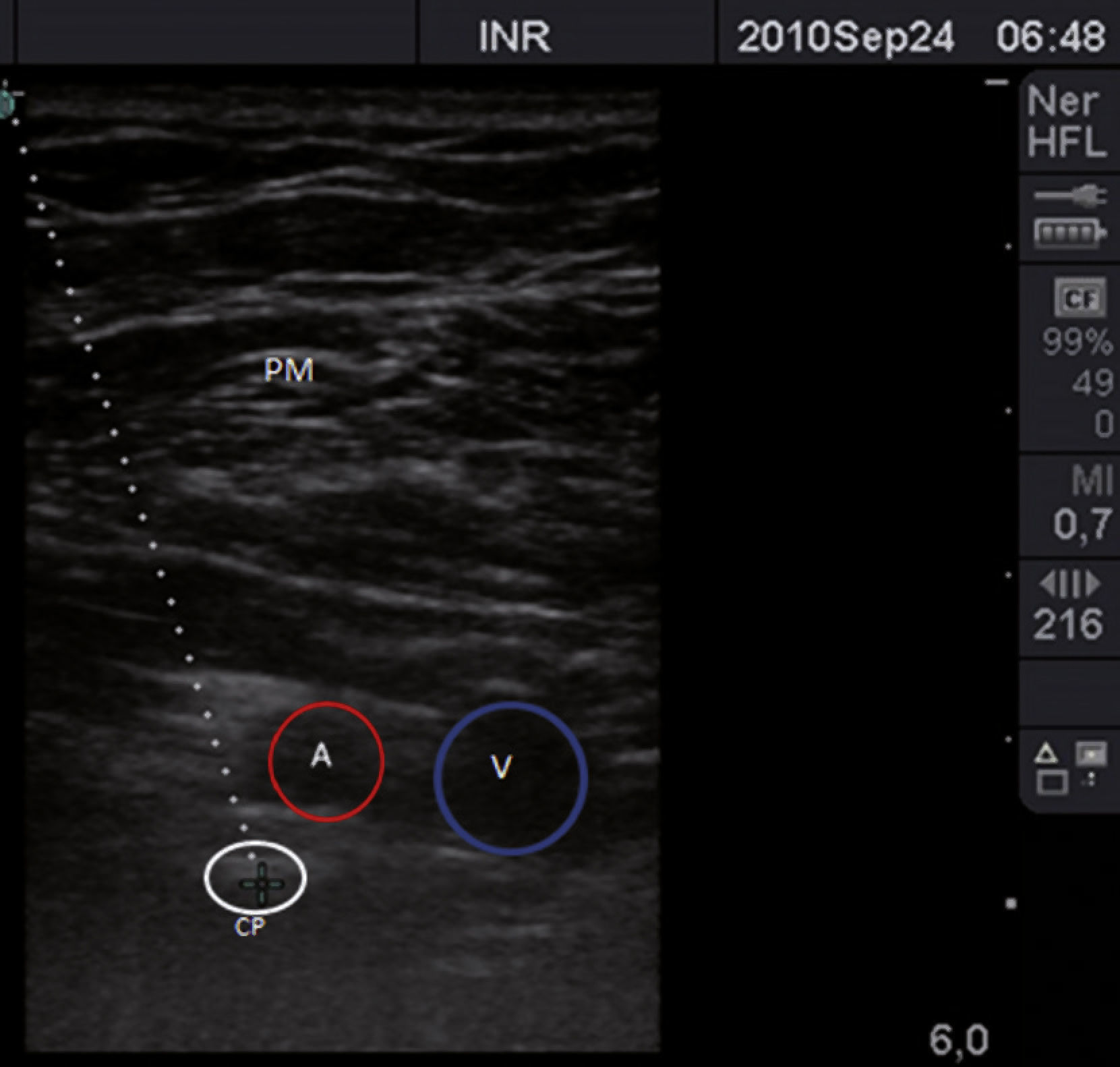
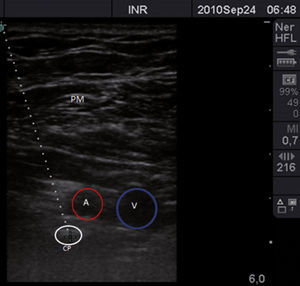
Initially, patients were divided into 2 groups, chosen consecutively: a group with arm in abduction and a group with arm in adduction. An ultrasound with high frequency linear transducer (13-15MHz) was used. The patients were placed in supine position, monitored in a non-invasive manner, and they were kept under conscious sedation. Consecutively, the arm was placed in adduction (Fig. 1) or in abduction (arm bent at 90) (Fig. 2).The long axis of the transducer was placed in the apex of the deltopectoral fossa, perpendicular to this region and underneath the coracoids in the parasagittal plane. The neurovascular structures were identified in the cross-sectional axis. The axillary artery was observed as reference to determine the brachial plexus cords; in a superior plane, the pectoralis major and pectoralis minor muscles were identified. The sonoanatomy found the axillary vein medial and caudal to the axillary artery (Fig. 3).
A Tuohy needle of 10cm and 18G was introduced under the clavicle, 0.5cm away from the cephalic end of the transducer, with in plane technique, advancing with 45-60 angulation in caudal direction, as shown in figure 4, until the posterior part of the axillary artery or the cranium posterior quadrant20 was reached. The guidewire was removed and, after aspiration, 30ml of local anaesthetic was administered, observing its distribution in “U” manner, or double bubble sign. If necessary, redirections were allowed, and even new punctures until diffusion was satisfactory. Afterwards, a 20 G catheter was introduced without passing the tip of the needle to avoid the arterial puncture; holding the catheter, the needle was removed half-way from the skin, it was stopped and the catheter was pushed 3 to 5cm more, removing the needle completely21,22, and the catheter was fixed to the skin in the anterior wall of the thorax. All the catheters were placed by the same anaesthesiologist, with the same surgical dose of ropivacaine 15ml 0.75% + 15ml lidocaine 2% with epinefrine. The motor block was assessed every 5min; the radial nerve was assessed with finger and arm extension, the median nerve with finger and wrist flexion, the cubital nerve was assessed with cubital flexion of the carpus and the 5th finger, and the musculocutaneous nerve with elbow flexion. The following scale was qualified: 0 = normal mobility, 1 = weakness and 2 = inability to produce movement. The sensitive block was assessed with puncture and response to cold in the distribution of these 4 nerves previously mentioned; median nerve in the palmar region of the index finger, cubital nerve in the palm of the little finger, musculocutaneous nerve in the antero-lateral region of the forearm in the back of the hand, with the following staging: 0 = normal sensitivity, 1 = analgesia (the patient can feel touch but not cold) and 2 = anaesthesia. The successful block was defined as a complete sensitive block in the area of the 4 nerves (musculocutaneous, median, radial and cubital) at 20min23. Pain was assessed with the visual analogue scale (VAS) at 6, 12 and 24hours after surgery, as well as the time of performance of the block and the time of placement of the catheter. Permeability and functionality were checked to document the number of punctures and redirections, the success rate, the time of insertion, the neurological injuries and the complications. Fig. 5
Based on the reports24, in which it is suggested that before catheter removal the patient is asked 3 questions to determine the satisfaction with the regional anaesthetic technique, the patients were asked a first question about the degree of satisfaction in 4 subjective categories with bipolar scale, which measures the positive, neutral and negative degree of every wording; the second question was if he would repeat the procedure in the future and, finally, which was the most uncomfortable component of the procedure. For each question, an explanation was requested for a negative answer.
The demographic data was analysed in a simple way with averages ± standard deviation and, in order to compare the study variable, a chi-square (x2) test was scheduled to obtain a statistically significant value of p<0.05, analysed with the SPSS programme, version 16, 2009, for Windows.
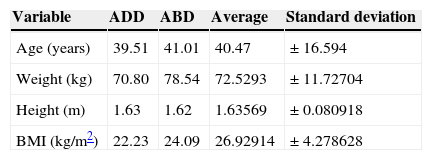
Results58 patients were included, 32 (55.2%) were men and 26 (44.8%) were women (Table 1). During the placement of the catheter, a single puncture was performed in 84.5% of the patients, 2 punctures were necessary in 8.5%, 3 were performed in 5.2% and up to 4 punctures were performed in 1.7%. The highest number of punctures was shown in the adduction group, confirming the criteria of the degree of difficulty due to the angulation of the clavicle that did not allow for correct placement of the transducer and, on the other hand, stopped the necessary angulation of the needle. These 3 criteria in order of appearance formed the degree of technical difficulty. Tables 2 and 3 describe the difficulty of inserting the catheter according to the position of the arm. The placement of the catheter was successfully performed with abduction of the arm in 48 patients (82.8%) and adduction of the arm only in 10 patients (17.2%). When identifying that the abduction variable was a constant success, this position was continued to be used in a preferential manner, until completing the cases to finish the total sample. When comparing the distance from the skin to the plexus, both in abduction and adduction, no statistically significant difference was found (p=0.9) (Table 4).The failure percentage was 3.33%; all these patients had the arm adduced. Complications appeared only in 17.2% of patients, such as paresthesia with the needle or catheter (6.9%), catheter output (5.2%), pain when removing catheter (1.7%), unsuccessful block (1.7%) and puncture of the axillary artery (1.7%).
Descriptive statistics of 58 patients subjected to infraclavicular catheter placement with ultrasound scan.
| Variable | ADD | ABD | Average | Standard deviation |
|---|---|---|---|---|
| Age (years) | 39.51 | 41.01 | 40.47 | ± 16.594 |
| Weight (kg) | 70.80 | 78.54 | 72.5293 | ± 11.72704 |
| Height (m) | 1.63 | 1.62 | 1.63569 | ± 0.080918 |
| BMI (kg/m2) | 22.23 | 24.09 | 26.92914 | ± 4.278628 |
ABD: abduction; ADD: adduction; BMI: body mass index.
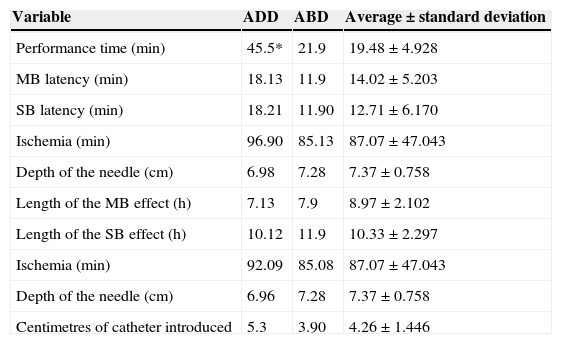
Descriptive statistics of the registered variables during the procedure of infraclavicular catheter placement with ultrasound scan in patients for superior limb surgery.
| Variable | ADD | ABD | Average ± standard deviation |
|---|---|---|---|
| Performance time (min) | 45.5* | 21.9 | 19.48 ± 4.928 |
| MB latency (min) | 18.13 | 11.9 | 14.02 ± 5.203 |
| SB latency (min) | 18.21 | 11.90 | 12.71 ± 6.170 |
| Ischemia (min) | 96.90 | 85.13 | 87.07 ± 47.043 |
| Depth of the needle (cm) | 6.98 | 7.28 | 7.37 ± 0.758 |
| Length of the MB effect (h) | 7.13 | 7.9 | 8.97 ± 2.102 |
| Length of the SB effect (h) | 10.12 | 11.9 | 10.33 ± 2.297 |
| Ischemia (min) | 92.09 | 85.08 | 87.07 ± 47.043 |
| Depth of the needle (cm) | 6.96 | 7.28 | 7.37 ± 0.758 |
| Centimetres of catheter introduced | 5.3 | 3.90 | 4.26 ± 1.446 |
ABD: abduction; ADD: adduction; MB: motor blockade; SB: sensitive blockade.
*p = 0.0019, statistically significant value.
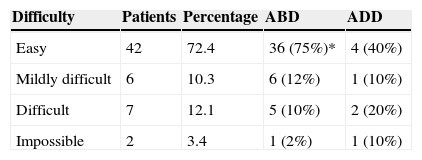
Classification of the assessment of the difficulty to introduce the catheter: based on the placement in the arm in abducted and adduced position.
| Difficulty | Patients | Percentage | ABD | ADD |
|---|---|---|---|---|
| Easy | 42 | 72.4 | 36 (75%)* | 4 (40%) |
| Mildly difficult | 6 | 10.3 | 6 (12%) | 1 (10%) |
| Difficult | 7 | 12.1 | 5 (10%) | 2 (20%) |
| Impossible | 2 | 3.4 | 1 (2%) | 1 (10%) |
ABD: abduction; ADD: adduction.
*p = 0.0012, statistically significant value.
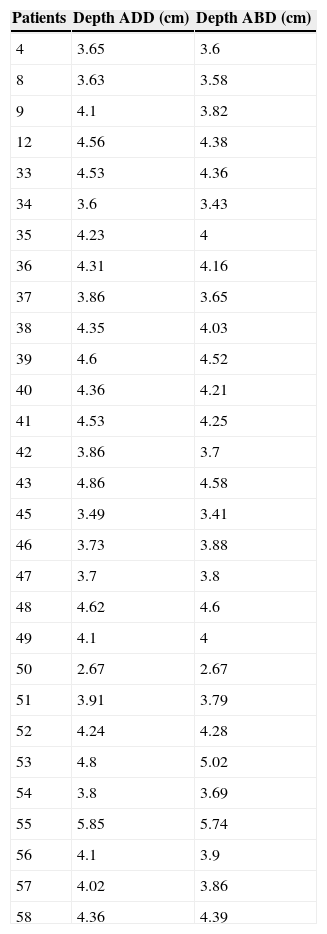
Skin-plexus distance of the infraclavicular approach.
| Patients | Depth ADD (cm) | Depth ABD (cm) |
|---|---|---|
| 4 | 3.65 | 3.6 |
| 8 | 3.63 | 3.58 |
| 9 | 4.1 | 3.82 |
| 12 | 4.56 | 4.38 |
| 33 | 4.53 | 4.36 |
| 34 | 3.6 | 3.43 |
| 35 | 4.23 | 4 |
| 36 | 4.31 | 4.16 |
| 37 | 3.86 | 3.65 |
| 38 | 4.35 | 4.03 |
| 39 | 4.6 | 4.52 |
| 40 | 4.36 | 4.21 |
| 41 | 4.53 | 4.25 |
| 42 | 3.86 | 3.7 |
| 43 | 4.86 | 4.58 |
| 45 | 3.49 | 3.41 |
| 46 | 3.73 | 3.88 |
| 47 | 3.7 | 3.8 |
| 48 | 4.62 | 4.6 |
| 49 | 4.1 | 4 |
| 50 | 2.67 | 2.67 |
| 51 | 3.91 | 3.79 |
| 52 | 4.24 | 4.28 |
| 53 | 4.8 | 5.02 |
| 54 | 3.8 | 3.69 |
| 55 | 5.85 | 5.74 |
| 56 | 4.1 | 3.9 |
| 57 | 4.02 | 3.86 |
| 58 | 4.36 | 4.39 |
Measure of the distance between the skin and the posterior cord in patients with arm position changed from ADD to ABD due to technical difficulty in the infraclavicular approach. There was no significant difference between both groups, p = 0.9.
ABD: abduction; ADD: adduction.
The VAS at 6hours was 0 in 98.3% of the patients; only one patient (1.7%) showed VAS of 7. At 12hours, the VAS was 0 in 53 patients (91.4%), 1 in one patient (1.7%), 4 in one patient (1.7%), 5 in one patient (1.7%) and 7 in 2 patients (3.4%). At 24hours, the VAS was 0 in 30 patients (51.7%), 3 in 12 patients (20.6%), 6 in 8 patients (13.7%), 7 in 6 patients (10.3%) and 8 in 2 patients (3.44%), with p=0.00411, with no significant value.
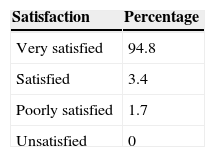
94.8% of the patients were very satisfied with the anaesthetic procedure, 3.4% were satisfied and 1.7% were poorly satisfied (Table 5). Although 53 patients (91.4%) defined the most unpleasant component of the entire procedure as the moment in which the needle went through the skin, the rest (8.6%) did not report any discomfort. 98.3% reported that, in case of requiring a new surgical procedure in the thoracic limb, they would prefer the same anaesthetic technique; only one patient (1.7%) said he would choose general anaesthesia.
DiscussionPosition of the arm changes the conditions in which the infraclavicular block is performed. Previous reports consider that the distance of the axillary artery to the skin is smaller when the arm is abducted. A report was made in oblique parasagittal plane, where it is referred that the position of the limb allows the image of the plexus to be clearer by diminishing the refraction of the ultrasound, apart from diminishing the probability of pneumothorax when separating the plexus from the chest wall15. However, Ruiz et al.16 reached the conclusion that the distance of the coranoid process to the neurovascular sheath (anatomical reference used in the placement of the transducer and neurostimulation) is constant, regardless of the position of the arm. The depth of the pleura does not change either, but it must be considered that the plexus is more superficial by abducting the arm though, nevertheless, Anyong et al.25 consider that this change in depth has a minimum clinical effect and the advantage lies in the displacement of the clavicle in a cranial direction, disappearing it from the needle track, called the Houdini effect, thus achieving greater space to manoeuvre the needle in order to introduce it in a more distant manner from the superior pole of the transducer and even see it better in its whole track. In this study, it was discovered that the plexus-skin distance decreases by abducting the arm. This is not statistically significant when compared to the measures obtained when adducing the extremity; indeed, the image is clearer and the limits of the vascular and neurological structures are more defined. Moreover, when introducing the needle there is no friction with the clavicle. This allowed us to perform a single puncture in 84.5% of the patients and, in case it was necessary, it was easier to redirect the needle, changing even the input angulation regarding the skin, a manoeuvre that was necessary to perform once in most of the patients. This image improvement enables the anaesthesiologist to be more specific with the identification of the posterior cord and to direct the tip of the needle towards it; the tip must be observed completely according to Tran et al.26 recommendation because, despite the use of ultrasound, a vascular puncture cannot be dismissed. Even Bigeleisen and Wilson15 indicate that in the abduction of the arm, the puncture of the axillary artery or vein is more likely when the multiple injection technique is performed by redirecting the needle to the medial cord, even though we did not redirect the needle with the purpose of placing it between the axillary vessels. Based on the aforementioned, our single vascular puncture was made with the arm abducted.
We used the double bubble sign, previously described by other researchers26,27, placing the local anaesthetic posterior to the axillary artery. Like Dingemans et al.28, we used a single injection, since it is considered that success does not depend on the number of injections, turning the single deposit of local anaesthetic into an easier, quicker and simpler technique. What is more, Sauter et al., 29 support our decision of single injection, affirming that the local anaesthetic must be administered in the cranealposterior quadrant regarding the axillary artery, referring to a clock face among 3 and 11. Since the administration in the posterior cord predicts greater success30, we placed the local anaesthetic there. Desgagnés et al.14 refer that the “U”, “doughnut” or “double bubble” sign provides a complete sensitive block in over 90% of the patients, referring to the single puncture technique, and the administration of the local anaesthetic through the needle. In our series, the success was 97.77% with the dose divided and administered through the needle and catheter. The latter matches with the assessment of Slater et al.31 who consider that the quality of anaesthesia obtained via catheter is as effective as when the local anaesthetic is only administered by needle, 90 vs. 92% success through catheter. In this study, a volume of 30ml of local anaesthetic was used, since Fuzier et al.32 considered this total dose sufficient, even though it was administered in a double injection in their work.
Furthermore, Ilfeld et al.23 affirm that the perineural catheter optimizes analgesia, both in single dose regimens and in infusion, and that the infraclavicular approach is a good option for this technique. In our series, we ascertained that in 89.7% of the patients, the catheter continued to be functional 12hours after placing it, with minimal complications, and a more frequent appearance of paresthesia during insertion when removing the catheter (6.9%). As regards the variable of technical difficulty observed through the parameters used by Anyong et al.25 it is possible to affirm that the insertion of the perineural catheter is relatively simple in most of the patients (72%) once the point of the needle has reached the posterior cord; the abduction of the arm technically facilitated the pass of the catheter, since it was introduced without difficulty in up to 88% of the cases with the limb in this position. Due to this reason, it is possible to recommend it with certainty. During the advance of the study, some patients from the adduction group were in excessive technical difficulty for puncture and handling of the Tuohy needle, due to the short distance between the transducer and clavicle. The aforementioned made redirections impossible, even the puncture site, because the point of the needle or its track matched that clavicular osseous structure, causing greater “discomfort” in the patient, altering the visualization of the cords without being able to maintain the quality of the image. Therefore, the transducer was placed again; in these cases, it was arbitrarily decided to change the position of the arm of the patient and to abduct it, achieving thus the handling of the needle and increasing the space for its manipulation25. In these cases, measures were taken regarding the superficiality of the brachial plexus to correlate with the position of the arm.
Bigeleisen and Wilson15 considered that the insertion time, quality and duration of the block are the same when it is performed with the arm adducted or abducted and with a single injection. We cannot confirm this information because we did not have comparative groups in that regard; however, the results are similar among each other when completing the dose via catheter, regardless of the position of the arm, showing a methodological weakness on that subject.
Taking into account that Bowens et al.30 indicated that puncture performance time with the administration of the local anaesthetic varies between 9 and 11minutes, in comparison, we can state that the time used in this study is acceptable; even with a difference of 8 more minutes, average of 19.48minutes, this time is subject to change depending on the user experience, according to Sandhu and Capan11, who referred that the learning curve for the intraclavicular block guided by ultrasound is 20 procedures, increasing at this point the level of success to 99%. As regards latency, we can expect that in 33±56min, the quality of the anaesthesia is appropriate to start a surgical procedure in the thoracic limb, including the placement of the perineural catheter.
A limitation to this study is that the assessment of the result regarding the position of the arm was not performed in a blind way, that is to say, the same anaesthesiologist that performed the block was responsible for assessing the motor block and the sensitive block, and the progress and the satisfaction of the patient.
The degree of patient satisfaction in our study was high, as was that informed by Bowens et al.30 who assessed pain during the infraclavicular block, mentioning a VAS of 35±27mm; likewise, in the postoperative period during 6, 12 and 24hours of charting, our results were similar with average VAS reports under 4, without statistically significant values. When the block was performed with neurostimulation, electrical stimulus was precisely referred to as the most painful component, but in our series, due to the use of ultrasound, patients reported more pain during the puncture of the needle into the skin.
ConclusionIn this study, the abduction of the arm moved the clavicle in a cephalic way and separated it from the linear transducer, which enabled manoeuvre of the needle in its angulation and redirection; the distance of the plexus to the skin did not diminish significantly with the position of the arm, but allowed for a better visualization of the neurovascular structures, facilitating the infraclavicular puncture and the insertion of the catheter.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Zaragoza-Lemus et al. Bloqueo infraclavicular continuo guiado por ultrasonido para cirugía de mano. Reporte técnico de la posición del brazo para la colocación del catéter perineural. Cirugía y Cirujanos. 2015; 83: 15-22.
Servicio de Anestesiología, 1.er piso. Instituto Nacional de Rehabilitación. Av. México-Xochimilco # 289, Col. Arenal de Guadalupe. Del. Tlalpan. C.P. 14389. México D.F., México. Teléfono: 59991000, ext. 11220.