In the management of hydrocephalus, the ventriculo-gallbladder shunt is justified in situations where the ventriculo-peritoneal shunt is not useful due to peritoneal involvement and/or when the ventriculo-auricular and ventriculo-pleural shunts are contraindicated.
Clinical caseA 27 year-old female with hydrocephalus at birth, managed with ventricle-peritoneal shunt, modified 3 times throughout her life due to repeated infections and other different reasons. She was admitted due to colitis caused by Clostridium difficile, presenting concomitant signs of intracranial hypertension and neurological impairment. This led to a review and change of the ventriculo-peritoneal shunt system, with distal dysfunction due to peritoneal thickening. Atrial and pleural shunts were not indicated because the risk of infection. As an alternative, it was decided to place the distal end of the catheter in the gallbladder. The patient recovered her neurological functions after the surgery.
ConclusionsDrainage alternatives may be needed in 5% of patients with valvular shunt dysfunction. The ventriculo-gallbladder is a good and viable option because it has an absorptive capacity of 1500cc liquid daily, besides being an excellent drainage through the bile duct. The abdominal surgery is easy to perform, and it is an alternative option in the failure of the ventriculo-peritoneal shunt.
En el manejo de la hidrocefalia, la derivación ventrículo-vesicular se justifica en situaciones en donde la derivación ventrículo-peritoneal no es factible por alteración del peritoneo, o cuando las derivaciones ventrículo-auricular y ventrículo-pleural están contraindicadas.
Caso clínicoPaciente femenina de 27 años con hidrocefalia al nacimiento, manejada con válvula de derivación ventrículo-peritoneal con recambio en 3 ocasiones por infección, es ingresada por colitis originada por Clostridium difficile. Presentaba de manera concomitante manifestaciones de hipertensión intracraneal con deterioro neurológico que obligaron a la revisión ventricular y a cambio de sistema de derivación ventrículo-peritoneal, con mal funcionamiento distal por engrosamiento del peritoneo. Ante la contraindicación de derivación auricular y pleural, se decidió colocar el catéter distal en vesícula biliar, logrando la recuperación de las funciones neurológicas.
ConclusionesEn el 5% de los pacientes que presentan disfunción valvular se deben buscar distintas alternativas de drenaje. La vesícula biliar es una buena opción, pues su capacidad de absorción le permite manejar hasta 1,500 cc diarios de líquido; además de ser un excelente drenaje a través de la vía biliar, presenta facilidad de realización, considerándose en la actualidad un procedimiento viable como segunda opción de derivación ante el fallo de la derivación ventrículo-peritoneal.
Approximately 40 out of every 100,000 people in the United States undergo surgery for ventricular shunts for the treatment of hydrocephalus. The majority of patients are children. Ventriculo-peritoneal shunts1 are most commonly used. Other options are the ventriculo-auricular shunt and the ventriculo-pleural shunt, used when the patient presents with abdominal abnormalities. An alternative is the ventriculo-gallbladder shunt. Its use has been justified in situations where the ventriculo-peritoneal shunt is not viable due to changes of peritoneium, generally caused by infection and when ventriculo-auricular and ventriculo-pleural shunts are contraindicated. The surgical technique is safe and effective, and is a useful procedure when other options cannot be indicated. When a patient presents with hydrocephalus and concomitant problems which require the use of this type of drainage of cerebrospinal fluid, we are committed to presenting the case. This is the objective of this paper.
Clinical caseA female patient aged 27 who was admitted to hospital after presenting with diarrhoea and general symptoms. The patient was recuperating from a ventriculo-peritoneal shunt replacement secondary to bacterial colonisation of the catheter in another hospital (June 06, 2014). During her stay there she received vancomycin for 21 days and ciprofloxacin for 10 days, apparently with no complications. Eight days prior to admittance she presented with loose bowel movements, nausea, vomiting and fever with no response to non specific treatment, which is why she went to this hospital. On admittance to the Emergency Department the patient presented with severe dehydration, drowsiness, fever, abdominal swelling, general abdominal pain on examination and enhanced peristalsis. The patient's clinical history was indirectly obtained (from her mother) who referred to: congenital hydrocephalus at 22 weeks of pregnancy, with a birth weight of 742g. Diagnosis at birth was congenital hydrocephalus, in addition to epilepsy. She spoke and responded correctly, although she had psychomotor limitations. A ventriculo-peritoneal shunt was inserted in 1986, a few days after birth, with replacement in 1989 due to malfunction, and in 2014 due to infection. The patient evolved favourable with regards to the diarrhoea. Initially she presented with leukocytosis of 15.7×103/μL with 36% segmented and 17% bandemia, hypocaliemia of 3.4 mEq/l and acidosis. A suspected diagnosis of infection by Clostridium difficile was made and testing for toxins A and B was requested. Since her hospital admittance she was administered metronidazol. Both toxins tested positive. The patient's diarrhoea improved, the leukocytosis fell to 11.2×103/μL and the bandemia to 6%, and her general condition improved. On the third day of hospital stay she presented with holocraneal, throbbing headache, projectile vomiting and drowsiness. An MRI scan was performed which showed dysfunction of the shunt system due to asymmetrical dilation of the ventricles, with severe transependymal migration, and intraventricular membranes forming heavy partitions and a complex system with detention of the left front horn, and agenesis of the corpus callosum. Puncture of the reservoir to obtain cerebrospinal fluid was performed, which reported turbidity and the presence of 1282leukocytes/mm3, as well as 40erythrocytes/mm3, proteins 107mg/dl and glucose 44mg/dl. We decided to carry out an endoscopic examination in addition to the imaging studies. The ventricular review showed changes of chronic ventriculitis including erythema and mottled haemorrhagic ependymal cells, thick membranes firmly attached to the ventricular walls forming partitions, causing detention of left front horn, turbid fluid with sediment and intraventricular catheter with thick membranes covering the majority of the orifices. Both ventricular catheters were removed, ventricular wash with 3l of physiological solution was performed, the membranes coagulating at their base were removed, as were the points of attachment. An opening was made at the frontal partition and the horn was rechanneled. A third ventriculostomy could not be performed since the ventricle floor was enlarged to the extent that it prevented visualisation of the cisterna and basilar artery. A new ventricular shunt system was inserted under direct view of the catheter tip and subsequently at peritoneal cavity, with a new right paramedian laparotomy (apparently virgin site), where under direct view and by probing, severe peritoneal enlargement with multiple partitions and firm attachments to intestinal flaps and epiplon were found, which impeded probing into the distal system. The patient evolved favourably with improvement, recovering her maximum state of alert and tolerating food orally. However, 36h later, she presented with progressive headache and vomiting on several occasions, with a tendency towards drowsiness. The reservoir presented an appropriate draining and filling function on examination, shown by computed tomography with the previously described ventricular morphology, with no transependymal migration of fluid and with an optimal proximal catheter location. Possible distal dysfunction was suspected, given the findings from the laparotomy, and this was surgically reviewed to confirm functioning and to insert a distal shunt in the gallbladder, since atrium and pleura shunts were contraindicated as a result of the chronic infection. In accordance with preoperative protocol, an ultrasound scan of the abdomen was performed which confirmed the presence of gall bladder, with no electrolytes inside it nor inflammatory alterations. Subcostal laparotomy was performed and the distal catheter was removed. This showed a continuous dripping of clear fluid. Cytochemical and culture testing of the fluid was carried out, dissection of the gallbladder's bottom, in addition to netting and puncture, removal of bile and probing of the distal catheter with a metallic connector to splint at anchorage and attachment point. The patient's evolution was favourable, with immediate postoperative recovery of maximum state of alert. The patient started walking 12h later and received food orally 24h following review. The cerebrospinal fluid tested as transparent and with no cells, and the culture tested negative to growth 4 days later. The patient remained in hospital until the antibiotic treatment had terminated and was discharged in a state of alert and walking, with wounds healing as intended.
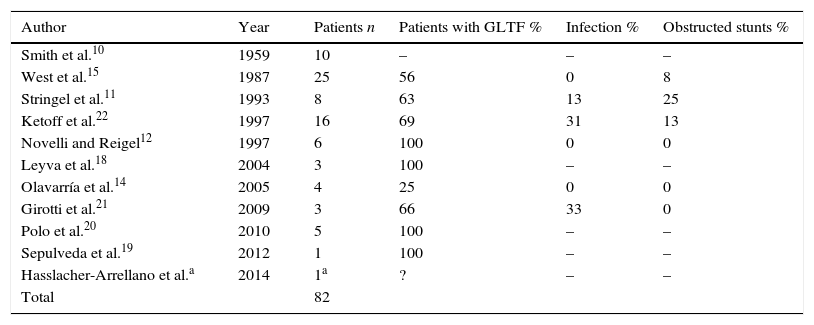
DiscussionThe ventriculo-peritoneal1 shunt is considered as the standard accepted technique for hydrocephalus management. Infection is the most significant complication caused by intracranial ventricular shunts, which affect between 1.5% and 38% of patients.2 Age seems to be an important risk factor, with infection rates among small children of up to 20%. Shunt infection may be associated with higher mortality, a higher risk of convulsive disorders and diminished intellectual performance. The ventriculo-pleural3 shunt is currently a frequently used alternative, which may present potential complications. Sometimes standard options are contraindicated4 due to special patient situations; at other times, the surgeon faces serious challenges which lead them to use unusual procedures for ventricular shunts. These are described in the literature for shunt valves connected to the pleural cavity, the pericardium,5 auricula,6 stomach, urethra, Fallopian tubes, bladder and saphenous veins,7,8 and the ventriculo-vena cava shunt.9 Another alternative (used in the case we are presenting) is the ventriculo-gallbladder shunt, initially reported by Smith et al.10 in 1959. To date under 100 cases have been reported in medical literature11–22 (Table 1).
Series of paediatric ventriculo-gallbladder stunts reported.
| Author | Year | Patients n | Patients with GLTF % | Infection % | Obstructed stunts % |
|---|---|---|---|---|---|
| Smith et al.10 | 1959 | 10 | – | – | – |
| West et al.15 | 1987 | 25 | 56 | 0 | 8 |
| Stringel et al.11 | 1993 | 8 | 63 | 13 | 25 |
| Ketoff et al.22 | 1997 | 16 | 69 | 31 | 13 |
| Novelli and Reigel12 | 1997 | 6 | 100 | 0 | 0 |
| Leyva et al.18 | 2004 | 3 | 100 | – | – |
| Olavarría et al.14 | 2005 | 4 | 25 | 0 | 0 |
| Girotti et al.21 | 2009 | 3 | 66 | 33 | 0 |
| Polo et al.20 | 2010 | 5 | 100 | – | – |
| Sepulveda et al.19 | 2012 | 1 | 100 | – | – |
| Hasslacher-Arrellano et al.a | 2014 | 1a | ? | – | – |
| Total | 82 |
–: no reported data; GLTF: good long term functioning.
Surgeons almost always avoid this shunt due to a lack of knowledge about changes in physiology and the presence of potential infection. The main function of the gallbladder in composition of bile is to absorb water and inorganic electrolytes.23 The range of fluid absorption by the gallbladder is approximately 16% of the total volume of the gallbladder per hour. The outcome of this is that there is a progressive increase in concentration of conjugated bile acids and a reduction in bicarbonate and chlorine concentrations. The result is a solution in which the concentrations of bile acid, sodium, potassium and calcium are high, with average potassium and calcium of 10 and 25meq/l, respectively. When a ventriculo-gallbladder shunt is performed, it is not viable to determine whether the cerebrospinal fluid from the gallbladder has been totally drained to the duodenum through the common duct or absorbed by the vesicular epithelium. Resistance of the vesicular epithelium to the osmotic passive fluid is high, with the need for a considerable osmotic gradient existing before water or cerebrospinal fluid can move in appropriate volume. It is known that bile re-absorption exists in the small intestine and that the gallbladder acts as a transitory reservoir, analogously to the serosal surface in the peritoneal cavity. Intra-abdominal pressure24 under normal conditions is 5mmHg (6.8cm H2O); this is transitorially increased with the Valsalva manoeuvre. Under pathological conditions this may increase to over 25mmHg (34cm H2O), which does not necessarily represent dysfunction of the valve, since all shunt valves have a one-way system which prevents the flow returning and as the intra-abdominal pressure again descends, the shunt function is repeated. Mean pressure of conventional shunt systems ranges between 8cm and 12cm of H2O. Central venous pressure at vena cava level ranges between 6cm and 12cm of H2O, right auricular pressure is 0–4cm H2O and at port system level is between 8cm and 14cm of H2O. In this respect, the study of 6 patients has confirmed that after the insertion of the ventriculo-gallbladder shunt there is reduction of approximately 20% of gallbladder ejection fraction. Follow-up of these patients shows that no ejection fraction changes present, nor shunt dysfunction, nor ventriculomegaly, with intestinal habits remaining normal. Due to the above, the gallbladder's ability to concentrate bile and absorb electrolytes remains unaltered, with successful absorption of cerebrospinal fluid. It has even been suggested that there is an advantage to the ventriculo-vesicular shunt over ventriculo-peritoneal shunts in the case of central nervous system neoplasms, since there is higher absorption difficulty in the peritoneum if the cerebrospinal fluid contains a higher quantity of proteins.14
An indication for specific ventriculo-gallbladder shunt usage is defective absorption of cerebrospinal fluid through peritoneal and pleural cavities, shown by the early formation of cysts.25 In general, the majority of patients treated with a ventriculo-gallbladder shunt has had an average of 3.9 ventricular shunts of a different type prior to using this approach (similar to the case we present). Ventriculo-peritoneal shunts may therefore present dysfunction due to peritonitis, peritoneal pseudocysts, pregnancy, ascites and infection, requiring an alternative drainage site. One of these is the gallbladder.26
The description of 18 patients in 2 small studies who presented with dysfunction11 in peritoneal level, auricular or pleural stunts caused by infection as the main cause, which led to defective absorption of cerebrospinal fluid. In another study on 25 children published in 1987, ventriculo-peritoneal shunt infection was also the most standard cause as an indication of the ventriculo-gallbladder shunt, using this approach as a rescue therapy.
Preparation for the use of the gallbladder should include an ultrasound scan of the gallbladder and bile dunts, particularly in cases of prior ventriculo-peritoneal shunts, and the use of prophylactic antibiotics. Contraindications are cholecystitis or bile duct disease, particularly the presence of salmonella; contaminated bile shown up by a culture is an absolute contraindication, as is the presence of systemic diseases predisposing to cholecystitis, particularly haemolytic diseases such as spherocytosis and sickle cell anaemia. Furthermore, if there is an intra-abdominal infection this will result in an early infection of the ventriculo-gallbladder shunt, and antibiotics should therefore be used in these cases to eliminate infection.
Surgical procedure is relatively simple and well tolerated. Subsequent follow-up is not free from complications, which when they present are similar to those of other shunt systems. In this regard, in the series of West and his team15 with 25 patients, infection occurred early in 25% of cases (prior to 2 months) and as a late complication in 37.5%. The most commonly found bacteria were Staphylococcus epidermidis. However, infection by Klebsiella pneumoniae, Candida albicans and Enterobacter cloacae were reported. Out of 5 infected patients, 2 responded to intravenous antibiotics and 3 required the removal of the ventriculo-gallbladder shunt and re-evaluation of the shunt. In another series11 of 8 cases, in 2 of them (25%), the need to remove the shunt was presented. In another series, 4% of cases presented with gallbladder atony, leading to temporary insufficiency of the shunt, which was resolved with the use of cholecystokinin. It was suggested that the use of narcotics and Oddi sphinter spasm were the cause of gallbladder atony. Gallstones17 were embedded in the distal part of the shunt causing abdominal pain, which necessitated check-up. The only reported death attributable to the ventriculo-gallbladder shunt was a bilious ventriculitis which caused the patient to have a neurogenic pulmonary oedema. Due to the above and in keeping with research studies, it may be said that the ventriculo-gallbladder stunt is similar in function to the ventriculo-peritoneal shunt and that long-term follow-up of patients means that between 60% and 70% still function correctly.19,20
Conclusions- •
Different drainage alternatives should be sought for 5% of patients presenting with dysfunction of the ventriculo-peritoneal shunt.
- •
The gallbladder is a good option due to its capacity for absorption, resulting in managing up to 1500cc of fluid daily (volume of cerebrospinal fluid normally produced per day by an adult, at around 0.35ml/min), apart from being an excellent drainage through the bile duct.
- •
Radiologic and ultrasound control is simple, as is vesicular pressure under the ventricular system.
- •
The procedure for inserting a ventriculo-gallbladder shunt and its safety for the treatment of non treatable hydrocephalus has increased over recent years. Experience with this procedure has increased due to it being more frequently performed.
- •
Indications have become more definitive. It is currently considered a viable procedure as a second shunt option when the ventriculo-peritoneal shunt fails, comparable with pleural and auricular stunts.
The authors have no conflict of interests to declare.
Please cite this article as: Hasslacher-Arellano JF, Arellano-Aguilar G, Funes-Rodríguez JF, López-Forcén S, Torres-Zapiain F, Domínguez-Carrillo LG. Derivación ventrículo-vesicular: una alternativa en el tratamiento de hidrocefalia. Cir Cir. 2016;84:225–229.