Surgically site infections (SSIs) are a major problem that limits the benefits of surgical interventions. The cumulative incidence of SSIs in colon surgery and compliance with antibiotic prophylaxis as well as the causes of non-compliance were evaluated.
MethodsMulti-centre prospective surveillance study between 2012 and 2019 in seven hospitals of the Canary Health Service using an active epidemiological surveillance system. SSIs was defined according to the criteria of the Centers for Disease Control and Prevention.
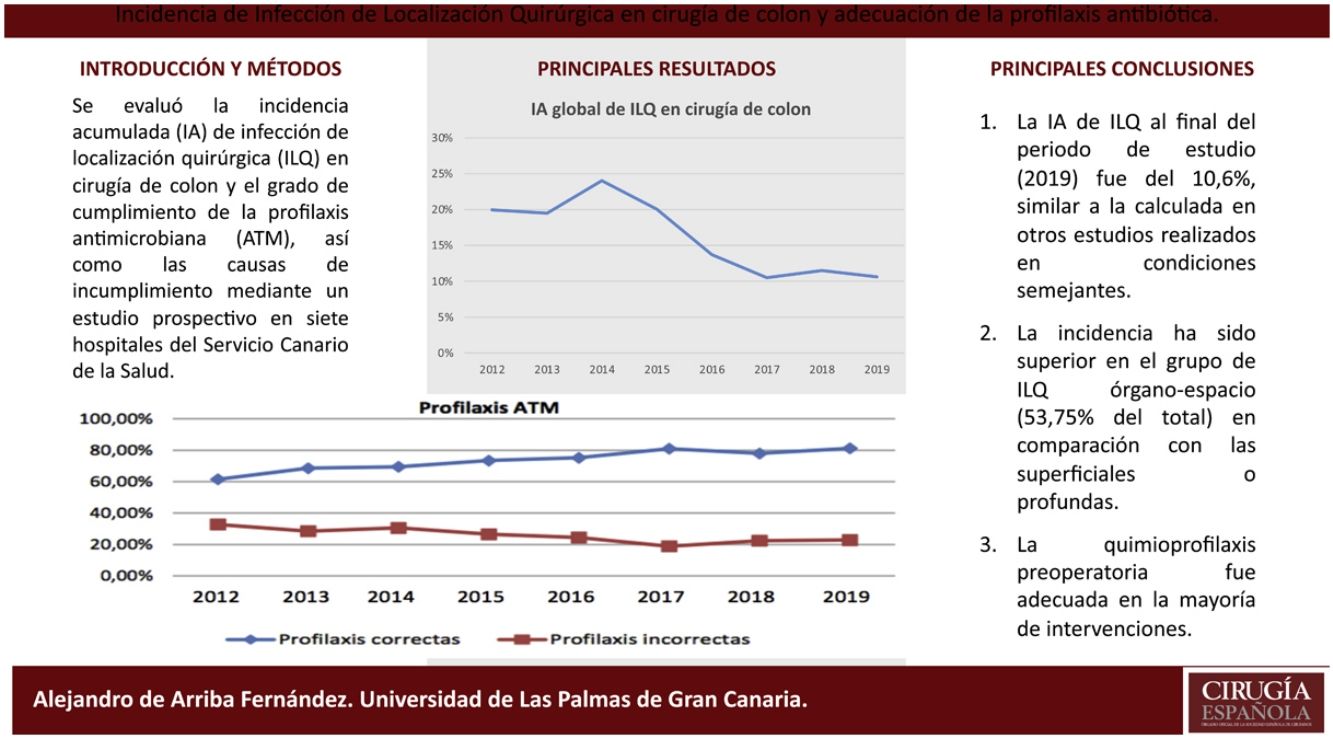
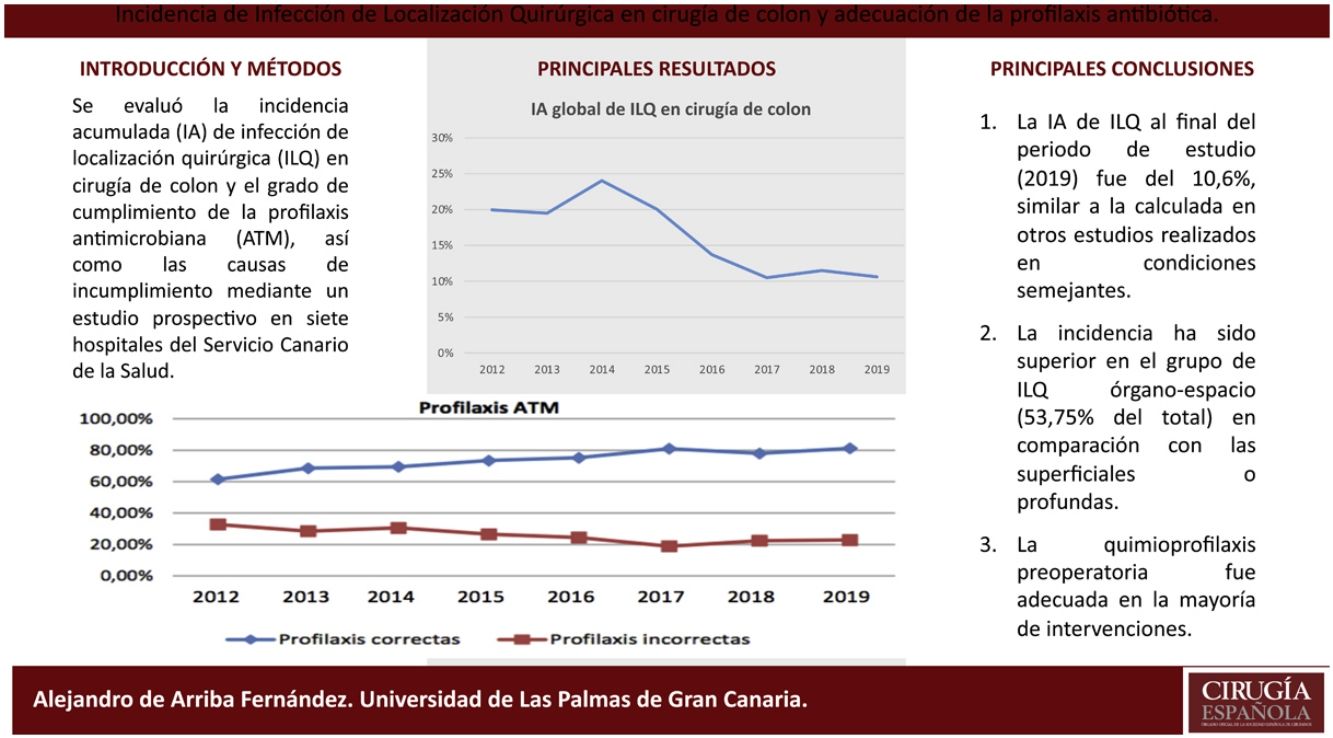
ResultsIn 2019, the cumulative incidence of SSIs was 10.6% (n = 80), which implies maintaining the downward trend since 2012. The appearance of SSIs was more frequent during admission (76%). Surgical prophylaxis was adequate in 81.2%, the main causes of inadequacy being the excessive duration of the antimicrobial prescription (49%) and failure in the indication (33%). The incidence was higher in the group of organ-space infections (53.75% of the total) compared to superficial and deep infections.
ConclutionThe cumulative incidence of SSIs obtained is similar to that calculated in other studies carried out under similar conditions. Preoperative chemoprophylaxis was adequate in most of the interventions.
Las infecciones de localización quirúrgica (ILQ) son un importante problema que limitan los beneficios de las intervenciones quirúrgicas. Se evaluó la incidencia acumulada de ILQ en cirugía de colon y el cumplimiento de la profilaxis antibiótica, así como las causas de su incumplimiento.
MétodosEstudio prospectivo observacional multicéntrico entre los años 2012 y 2019 en siete hospitales del Servicio Canario de Salud mediante un sistema de vigilancia epidemiológica activa. Se definió ILQ de acuerdo con los criterios de los Centers for Disease Control and Prevention.
ResultadosEn el año 2019 la incidencia acumulada de ILQ fue del 10,6% (n = 80), lo que supone mantener la tendencia descendente desde el año 2012. La aparición de ILQ fue más frecuente durante el ingreso (76%). La profilaxis quirúrgica fue adecuada en el 81,2%, siendo las principales causas de inadecuación la duración excesiva de la prescripción del antimicrobiano (49%) y los fallos en la indicación (33%). La incidencia ha sido superior en el grupo de ILQ órgano-espacio (53,75% del total) en comparación con las superficiales o profundas.
ConclusiónLa incidencia acumulada de ILQ obtenida es similar a la calculada en otros estudios realizados en condiciones semejantes. La quimioprofilaxis preoperatoria fue adecuada en la mayoría de intervenciones.
Surgical site infections (SSIs) are a major public health and patient safety problem that limit the potential benefits of surgical interventions.1,2 Patients who develop an SSI are more likely to have higher mortality, longer stays in hospital and in critical care units, and are more likely to be readmitted. All this, coupled with an increase in additional tests and additional antibiotic use, leads to a significant increase in costs.3,4
According to data from the 2019 EPINE report, the prevalence of nosocomial infections in Spain is 7.15%, and SSIs are the most frequent, a situation that has been continuously repeated since 2015.5
Colon surgery is, together with appendicular surgery, the surgery with the highest risk of infection in the abdominal area, and SSIs are the most frequent complication among patients undergoing elective colorectal surgery.6,7 Prophylactic antibiotic therapy is routinely administered in the perioperative period to prevent SSIs.8 The first dose of antibiotic should be administered within 60 min prior to incision, so that therapeutic levels have been achieved in blood and tissues prior to contamination. Antibiotics should be chosen according to the type of intervention and prophylaxis should not be prolonged beyond the first 24 h after the intervention.9
Surveillance with adequate feedback of data to surgeons has proven a key component of strategies to reduce the risk of SSIs.10 An effective surveillance system is an essential element of any programme aiming to reduce nosocomial infection (NI) rates.11 The purpose of epidemiological surveillance is to provide the information necessary for the control and prevention of communicable diseases in the population.12
We evaluated the cumulative incidence (CI) of SSIs in colon surgery and compliance with antibiotic prophylaxis, as well as the causes of non-compliance.
MethodsProspective observational epidemiological study analysing the incidence of SSIs in colon surgery in a Spanish region and their course over 8 years (2012–2019) using an epidemiological surveillance system. The degree of compliance with antibiotic prophylaxis and the causes of non-compliance in colon surgery were evaluated: indication, duration, initiation, and non-repetition.
The 7 hospitals of the Canary Islands’ health system with teaching accreditation provided data: 4 type I hospitals, with more than 500 beds, and 3 type II hospitals, with less than 500 beds.
The inclusion criteria were elective and urgent colon surgery (understood as incision, resection, or anastomosis of the large intestine, including large intestine to small intestine or small intestine to large intestine anastomosis), single procedures were included, or procedures associated with others (excluding rectal surgery), and classified as clean-contaminated or contaminated surgery. The codes used were ICD-9-CM: 17.3 (laparoscopic partial excision of large intestine), 45 (incision, intestinal removal, and anastomosis), and 46 (exteriorisation of large intestine).
Exclusion criteria were confirmed or suspected infection at the time of surgery, or antibiotic treatment that was not antibiotic prophylaxis.
The surveillance system for nosocomial infections in the Canary Islands (SVINCAN) included active surveillance of SSIs after discharge for a period of 30 days after surgery. Readmissions were used as a method of capturing SSIs appearing after the date of discharge. Consultations in primary or specialist care centres were not taken into account.
Preventive medicine services performed clinical follow-up and periodic monitoring (every 24 or 48 h) of patients admitted for and undergoing colon surgery. The sources of information were medical records, nursing notes, clinical records, diagnostic techniques, and microbiological results, as well as direct contact with the medical and care team in the surveilled areas.
The criteria for defining SSIs and stratification by risk index are as established by the Centers for Disease Control and Prevention13 and the National Nosocomial Infections Surveillance System (NNIS).14 Interventions were grouped for analysis according to procedures established by the National Healthcare Safety Network.15
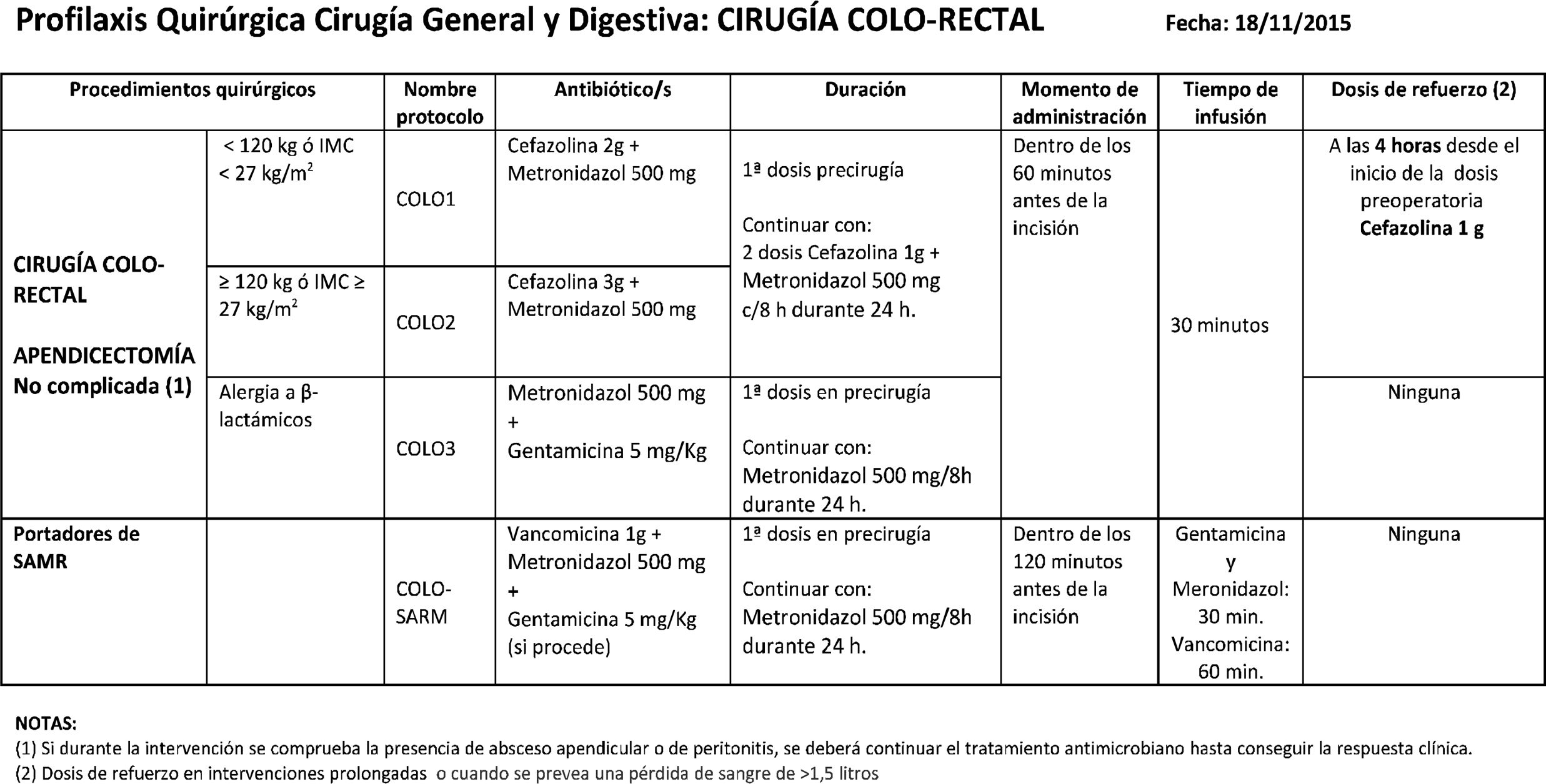
The adequacy of the antibiotic prophylaxis administered was analysed by comparing it with the antibiotic prophylaxis defined in the current antibiotic prophylaxis protocols in the hospitals studied (Table 1). The adequacy of the antibiotic administered, the administration route used, the dose and time of administration of the antibiotic were studied. For the latter, both previous and intraoperative doses were considered, if indicated, as well as doses after the operation. No common protocol for the use of oral antibiotic prophylaxis and/or mechanical colon preparation was used in the centres studied.
Statistical analysisA descriptive analysis of the results was performed using frequency measures and percentages for categorical variables. Calculation of the CI of hospital-onset colon surgery SSI cases was set as the number of colon surgery SSI cases within each period in the numerator and the total number of stays during the surveillance period in the denominator. We calculated the CI for each indicator overall, by hospital group and adjusted by NNIS risk index. SPSS, v. 24 was used for the statistical treatment of data.
ResultsIn 2019, 754 surgical procedures to the colon were monitored; 16% less than the previous year. Of the total number of procedures, 73.20% were scheduled. Table 2 shows the number of procedures monitored according to NNIS index and hospital type.
N° of procedures surveilled according to the NNIS index and type of hospital.
| Group I hospitals | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
| RI 0 | 43 | 66 | 59 | 63 | 85 | 78 | 92 | 90 |
| RI 1 | 221 | 174 | 218 | 255 | 260 | 247 | 319 | 273 |
| RI 2 | 245 | 271 | 320 | 290 | 257 | 280 | 315 | 266 |
| RI 3 | 99 | 64 | 66 | 57 | 51 | 54 | 45 | 55 |
| Total | 608 | 575 | 663 | 665 | 653 | 659 | 771 | 684 |
| Group II hospitals | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
| RI 0 | 13 | 16 | 9 | 26 | 35 | 61 | 16 | 18 |
| RI 1 | 22 | 39 | 35 | 63 | 96 | 45 | 67 | 38 |
| RI 2 | 12 | 33 | 14 | 42 | 37 | 15 | 34 | 14 |
| RI 3 | 1 | 3 | 3 | 7 | 3 | 1 | 7 | 0 |
| Total | 48 | 91 | 61 | 138 | 171 | 122 | 124 | 70 |
NNIS, National Nosocomial Infection Surveillance; RI, Risk Index.
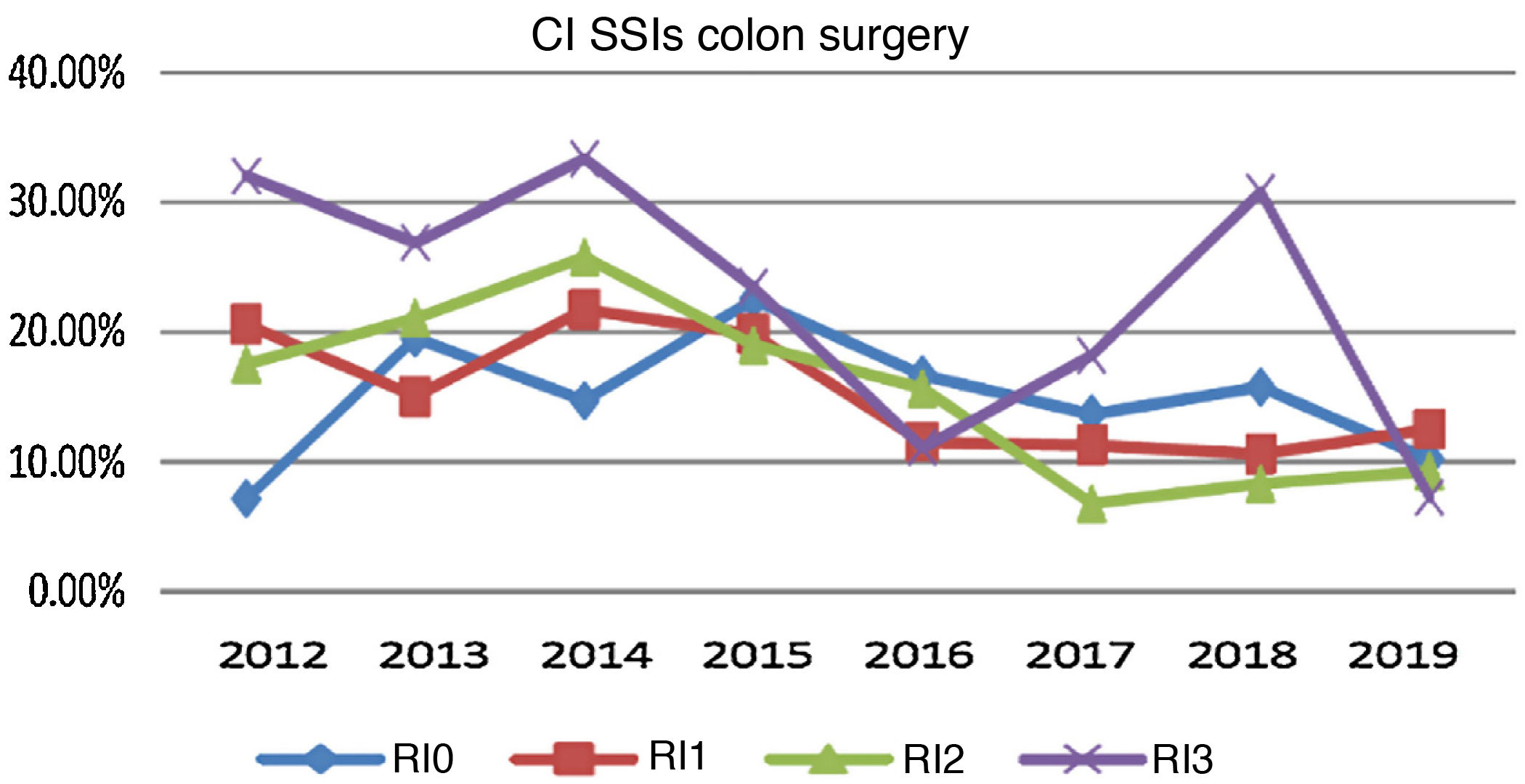
The cumulative incidence of SSIs in colon surgery by NNIS risk is shown in Fig. 1.
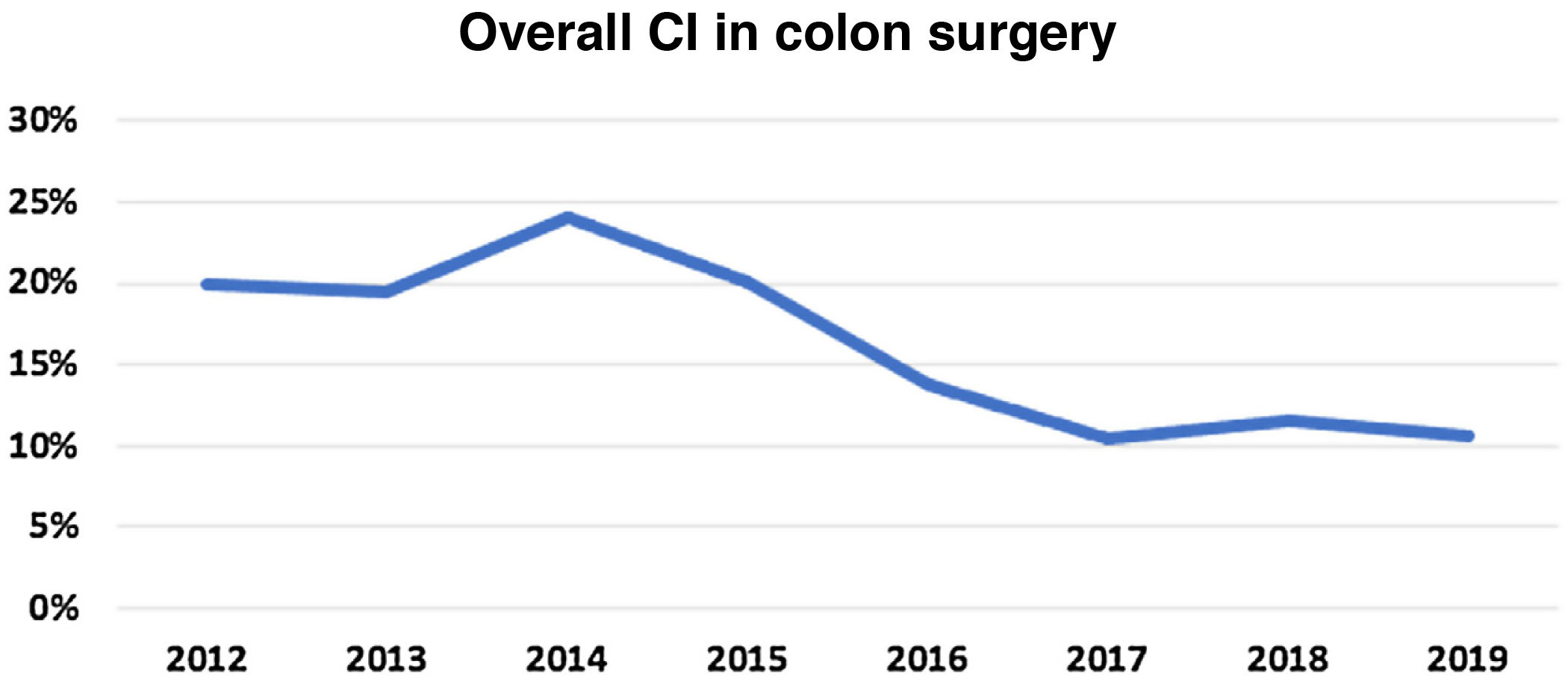
The overall CI of infection in 2019 for both scheduled and urgent interventions was 10.61%, a decrease of one percentage point from the previous year (Fig. 2).
If we consider depth of infection, there was an upturn in superficial infections in 2019. In the case of organ-space SSIs, the behaviour was the opposite, with a decrease in 2019, although without a return to the figures of previous years. Fig. 3 shows the percentage distribution of SSIs in overall colon surgery, according to depth of infection and type of hospital.
Based on the time of onset of SSIs, in 2019 the highest number of infections occurred during admission, accounting for 76% of all infections (slightly lower than in previous years). In 2012, 95% of SSIs occurred during admission.
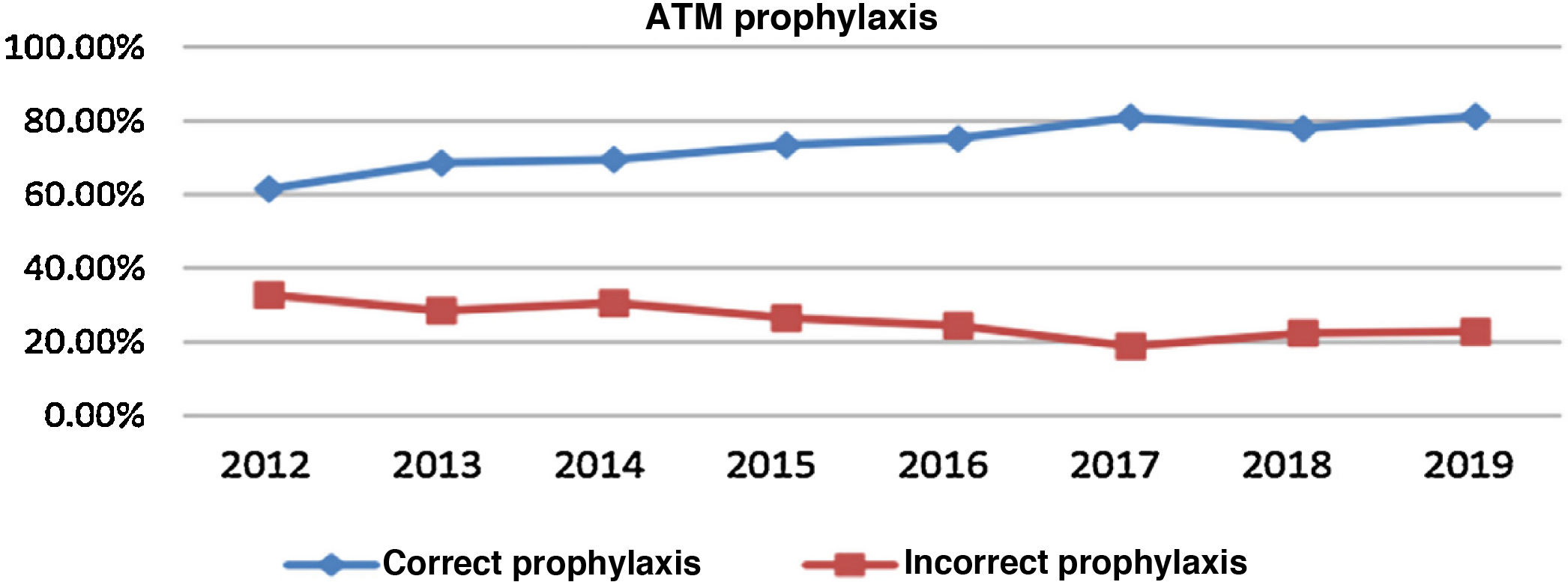
Correct prophylaxis increased by 20% over the study period, from 61% in 2012 to 81% in 2019 (Fig. 3).
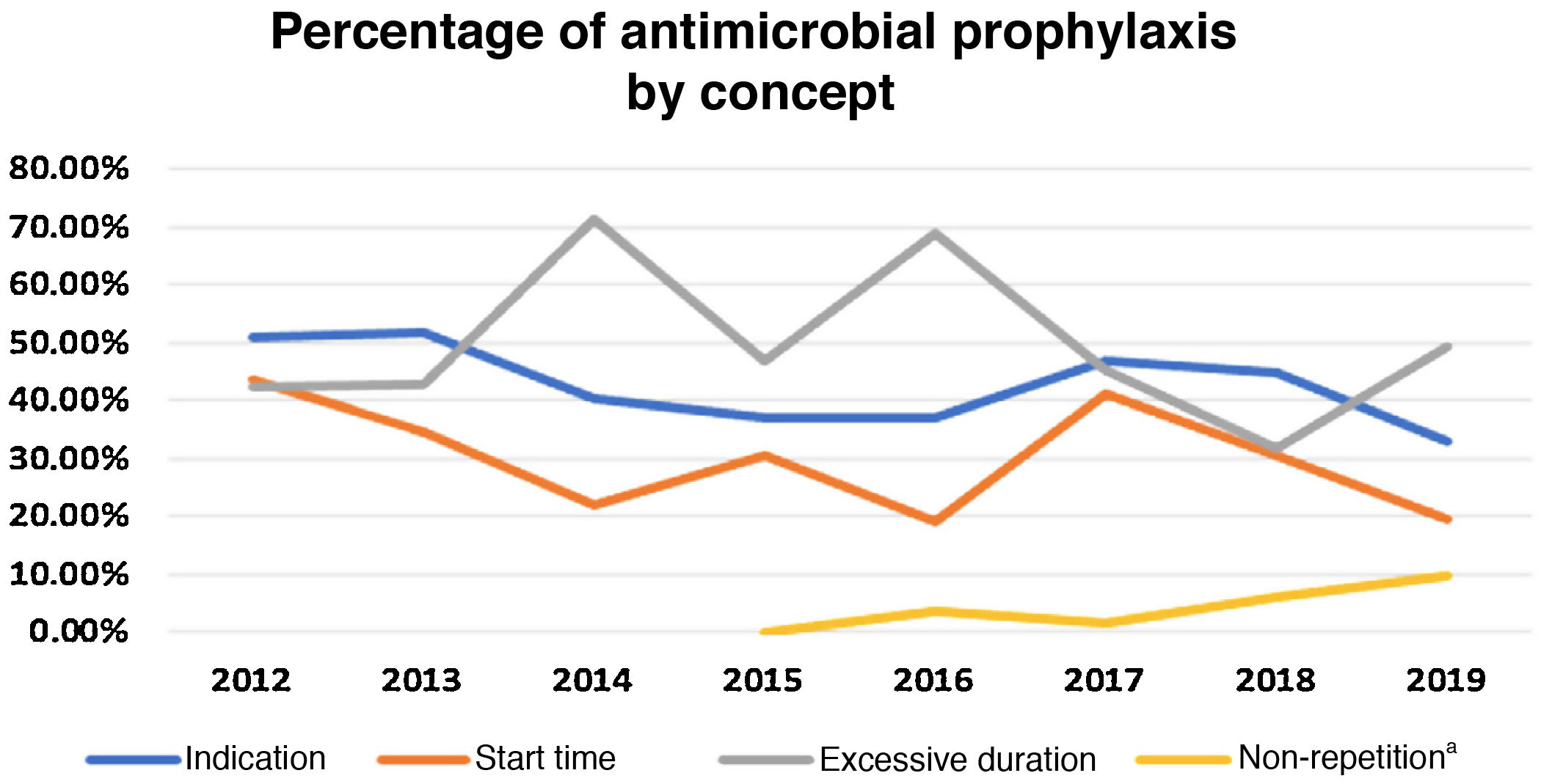
Of the total incorrect prophylaxis given in 2019 (19.92%), 33.1% was due to an error in the indication (antimicrobial not adjusted to that stated in the protocol), 19.72% due to administration outside the stipulated time (>60 min from drug administration to skin opening or initiation of therapy after incision), 49.30% due to excessive duration of antimicrobial prescription, and 9.86% due to non-repetition of antimicrobial in surgeries of long duration (the total may be more than 100, as there may be more than one cause of inadequacy). Fig. 4 shows the percentage of incorrect prophylaxis by concept.
DiscussionThe main finding is that the overall incidence of SSIs has decreased from 20% in 2012 to 10.6% at the end of the study period in 2019, with variations between years.
The observed incidence of SSIs is similar to that published by surveillance systems using the same methodology and the same diagnostic and classification criteria.16–21 Thus, the study by López-Barrachina et al.1 in 2017–2019 showed a CI of 10.6% and, recently, the Spanish Association of Coloproctology studied between 2013 and 2017 almost 2,000 elective colon surgery patients from 18 units across the country22 and found an CI of 11.4%, very similar to ours. The European Centre for Disease Prevention and Control published epidemiological surveillance data on SSIs for the period 2010–2011,23 colon surgery was the first procedure in terms of CI (9.5).
In this study, the high percentage of SSIs detected after discharge is striking, approximately 25% of cases in 2019. It is to be expected that SSIs are primarily detected during admission.
The overall adequacy rate of surgical prophylaxis in the latest year 2019 was 81.2%, an all-time high, having increased by 20% since the study began in 2012. The most common contributor to protocol non-compliance was excessive duration of antimicrobial prescription (49%) and indication errors (33%). We could not analyse incorrect prophylaxis and the incidence of SSIs in this study because the hospitals submitted data on an aggregated basis.
Other studies describe that prophylaxis can prevent 56% of infections and reduces deep infection by 47%.24 In the study by Del Moral et al. published in 2017, antibiotic prophylaxis was administered in 97.8% of patients, with an overall protocol compliance of 91.9%.6
Clinical studies showed a decrease in SSIs when oral prophylaxis combined with mechanical colon preparation was used. Oral antibiotic administration in the absence of mechanical colon cleansing appears to have efficacy in observational studies, but its effect is inferior to combined preparation.25 Our community is working to establish a common protocol to define the cases in which combined mechanical and antibiotic oral preparation is indicated to improve postoperative infection prophylaxis in colon surgery.
The results of this study have several limitations. The geographical scope was limited to a certain region, which may limit its external validity.
The great methodological variability makes it difficult to compare data and increases the complexity of interpretation; it may be that emergency surgery entails a higher rate of SSIs than elective surgery and is a confounding factor in the analysis of the results in terms of SSIs and compliance with protocols. We believe that a trend analysis to define whether the improvement in outcomes over the years of follow-up is statistically significant is indicated for future studies.
Readmissions were used as a method of identifying SSIs, and it is possible that there were several superficial infections diagnosed in consultations and not requiring admission. This could lead to an underestimation of cases of superficial infection. A possible solution would be to record the progression of the surgical wound at outpatient level, and consider using telemedicine through virtual consultation or monitor superficial SSIs through a mobile application for postoperative care, as this is an efficient and satisfactory tool for patients and has excellent clinical results.26
In conclusion, we found a decrease in the CI of SSIs in the last study period, which is within the desirable margins for this type of infection, similar to that calculated in other studies conducted under similar conditions. We believe that an observational study is needed to objectively evaluate other factors involved in the development of SSIs, such as, age, comorbidities, surgeon's experience, use or non-use of drains, etc. The causal germ is not analysed either, which may be, related to the increase in incidence in the last year analysed, this data may even be, useful for the authors' objective to act to prevent infection.
The adequacy of the antibiotic prophylaxis protocol was considered high at the end of the study period. We believe that several factors must have played a role, including the increased awareness of the surgical team after implementation of the surveillance programme. We believe it is important to maintain adequate administration of prophylaxis according to the defined protocols and to evaluate this adequacy in order to take the necessary measures to improve it and reduce the incidence of SSIs.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the microbiology laboratories of the hospitals of the Canary Islands Health Service and the hospitals and healthcare professionals participating in SVINCAN.
- -
Hospital General de Fuerteventura. Guadalupe Alemán Vega. Preventive Medicine Service. Pino Suárez Bordón. Microbiology Service. Type II hospital.
- -
Pablo Jadraque Jiménez. Hospital General de La Palma. Preventive Medicien Service. Type II hospital.
- -
María Lecuona Fernández. Complejo Hospitalario Universitario de Canarias de Tenerife. Microbiology and Infection Control Service. Type i hospital.
- -
Elena Dorta Hung and Josefina Panetta Monea. Complejo Hospitalario Universitario Insular Materno Infantil de Las Palmas de Gran Canaria. Preventive Medicine Service. Type I hospital.
- -
Teresa Montserrat Blasco. Hospital Universitario de Gran Canaria Doctor Negrín. Preventive Medicine Service. Type i hospital.
- -
Domingo Panizo Rivas. Hospital Doctor José Molina Orosa de Lanzarote. Preventive Medicine Service. Type ii hospital.
- -
Álvaro Torres Lana. Complejo Hospitalario Universitario Nuestra Señora de Candelaria de Tenerife. Preventive Medicine Service. Type I hospital.
- -
Nuria Bañón Morón. Specialist Care Service. Care Programme General Management.
- -
Elizabeth Hernández González. Care Programme General Manager.