The high morbidity and mortality of emergency surgery have led to the use of endoluminal self-expanding metal implants (stents) in the management of intestinal occlusion.
The purpose of this study was to review the results of the management of intestinal occlusion treatment in a Colorectal Surgery Unit in those patients who had a stent implant, and the relationship between chemotherapy and complications.
Materials and methodsA retrospective study was carried out on patients treated with a stent in a university hospital between 2004 and 2010.
ResultsA total of 93 patients were treated, of whom 77 were considered palliative for a stage IV neoplasm of the colon with non-resectable metastases or due to a performance status >2. Other indications were 7 ASA IV patients with acute renal failure, 6 with benign disease, and 3 due to other causes.
The technical success and clinical success of the procedure were 93.5% and 78.5%, respectively. Delayed occlusion was 19.3% and perforation 6.4%. There were migration (2.1%) and intestinal bleeding (2.1%) and 1.1% with tenesmus. No significant differences were seen between complications and chemotherapy.
The overall mortality was 17.2%.
ConclusionsStents, as a definitive treatment option in palliative patients with and without chemotherapy, is an alternative treatment that is not exempt from complications. We believe that in patients with mortality risk factors and patients with tumours with non-resectable metastases it could be the initial treatment of choice.
La elevada morbimortalidad de la cirugía de urgencias, ha favorecido la utilización de prótesis endoluminales metálicas autoexpandibles (stents) en el manejo de la oclusión de colon.
El objetivo del estudio fue revisar los resultados en el manejo en una Unidad de Cirugía Colo-rectal del tratamiento de la oclusión de colon, en aquellos pacientes a los que se les colocó un stent y la relación entre quimioterapia y complicaciones.
Material y métodosSe realizó un estudio retrospectivo de los pacientes tratados con un stent entre 2004 y 2010, en un hospital universitario.
ResultadosFueron tratados 93 pacientes, 77 se consideraron paliativos por neoplasia de colon estadio IV con metástasis irresecables, compresión extrínseca o infiltración de neoplasia extracólica irresecable o por un performance status > 2. Otras indicaciones fueron 7 pacientes ASA IV con insuficiencia renal aguda, 6 por enfermedad benigna y 3 por otras causas.
Los éxitos técnico y clínico del procedimiento fueron del 93,5% y del 78,5% respectivamente. La oclusión tardía fue del 19,3% y la perforación del 6,4%. Migración y hemorragia digestiva 2,1% cada una y el tenesmo del 1,1%. No observamos diferencias significativas entre complicaciones y tratamiento con quimioterapia.
La mortalidad global fue del 17,2%.
ConclusionesLos stents como tratamiento definitivo en pacientes paliativos con y sin quimioterapia son una alternativa terapéutica no exenta de complicaciones. Creemos que en pacientes con factores de riesgo de mortalidad y pacientes con tumores con metástasis irresecables podría ser el tratamiento inicial de elección.
Colon obstruction represents the primary cause for emergency colorectal surgery, occurring in over 70% of cases distal to the splenic flexure of the colon.1 The most common cause is colorectal cancer (CRC), followed by other pelvic neoplastic processes such as prostate, urinary bladder, and ovarian cancer.2
The incidence of obstruction increases with age, and generally occurs in patients with associated comorbidities3 and in advanced stages of neoplastic disease.4 In its evaluation and management, after the initial revival process, the diagnosis and staging of the disease must include an estimation of life expectancy, identifying which patients will be eligible for curative treatment and which will be considered for palliative care.
The traditional treatment for colon obstruction is emergency surgery, attempting to resolve during the same surgical procedure the obstruction itself and the underlying cause. Reconstruction of intestinal transit in emergency surgery has been proposed as the initial treatment objective, though this requires a series of circumstances that are not always present, and therefore, a primary anastomosis is not always possible.
The technological advances made in recent decades have allowed for the development of new treatment options, modifying protocols and treatment strategies for certain conditions such as colon obstruction.
The placement of implants in the gastrointestinal tract led to the use of colonic stents (endoluminal self-expanding metal implants) by Dohmoto5 in 1991 as an alternative to surgical treatment for colon obstruction. The high mortality and morbidity rates of emergency surgery,6 along with the high rate of colostomies, have led to a diversification of the treatment indications for stents since their first description in the treatment of malignant left colon obstruction in palliative patients.
In spite of the simplicity and benefits reported by several different publications on this technique, with low rates of morbidity and mortality,7,8 its use has come into question, especially in patients receiving chemotherapy treatment, due to the risk of severe complications.9,10
The objective of this study is to review the results from the treatment of colon obstruction in a colorectal surgery unit, focusing on patients treated using the placement of a self-expanding metal stent, and to assess a possible relationship between systemic chemotherapy treatment and the appearance of complications.
Materials and MethodsWe performed an observational study among all patients who were treated in the colorectal surgery unit at the Hospital Universitari de Bellvitge following the placement of a colon implant between the months of January 2004 and September 2010. Part of the group of patients included in this study were also included in a previously published paper.10
The patient data were obtained from a prospective database including information on all patients with colorectal ailments treated at this hospital.
The indications for the placement of a stent were: patients with colon obstruction distal or adjacent to the splenic flexure with the following characteristics:
- 1.
Palliative:
- -
stage IV CRC with non-resectable metastases,
- -
CRC performance status (WHO) greater than 2,
- -
extrinsic compression or compression due to non-resectable extracolonic neoplastic infiltration.
- -
- 2.
Bridge to surgery: CRC patients with high surgical risk (ASA IV) with associated acute kidney failure, or transferred from other institutions;
- 3.
Benign pathology: stenosis of the anastomosis from the colon surgery.
We excluded patients with suspected perforated colon and with tumours in the mid-low rectum (less than 7cm from the anal margin).
We defined complete colon obstruction as the total absence of gases and/or faeces during at least the past 24h, associated with abdominal distension, with or without nausea and vomiting, and abdominal X-ray showing dilated colon. The diagnosis was confirmed using a Gastrografin® enema (Bayer-08970, S. Joan Despí, Barcelona, Spain) or an abdominal CT scan with intravenous and oral contrast.
An incomplete obstruction, such that of patients diagnosed with stenosing colon cancer via colonoscopy, was diagnosed using an enema that allowed for the filiform passage of contrast medium in patients who complained of intermittent, cramping abdominal pain, but with the passage of gases and faeces. In these cases, the implant was placed on a semi-elective basis within 5days by the interventional radiology team. A complete obstruction was treated as an emergency case by the on-call interventional radiologist.
Stage IV was defined as a distant metastasis in any location (liver, lungs, bones, peritoneum, retroperitoneal lymph nodes, and suprarenal glands) diagnosed by CT scan. We considered patients to be palliative when non-resectable hepatic or extra-hepatic metastases were present. Hepatic metastases were considered to be non-resectable when involving more than 70% of the hepatic parenchyma or in the case of multiple bilateral metastases, portal involvement, bilateral venous infiltration, infiltration of 3 hepatic veins, or metastatic nodules in the vascular pedicle. Extra-hepatic disease was considered non-resectable in the case of peritoneal carcinomatosis, bilateral pulmonary metastases, retroperitoneal nodules, and bone metastases.
The evolution of the different phases of management was defined as:
- -
Technical success: correct placement of a stent through the stenosis;
- -
Clinical success: clinical and radiological evidence of resolution of the obstruction within 48h of the stent placement, with no complications related to the stent insertion (absence of decompression and colon perforation);
- -
Delayed obstruction: appearance of occlusive symptoms in stented patient after a period of correct functioning and after ruling out the possibility of faecal impaction;
- -
Delayed perforation: perforation of the colon following a period of correct stent functioning;
- -
Other complications: bleeding, migration, and tenesmus;
- -
Mortality: we considered this as death within 30days of the attempted treatment, regardless of the clinical or technical success of the stent placement.
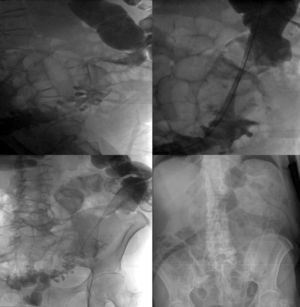
The procedure was performed under conscious sedation in the interventional radiology unit. The combination of a Gastrografin® enema and the fluoroscopy-assisted manipulation of the guide and catheter allows for the localisation and demarcation of the tumour, bringing the stent catheter to the point of stenosis. The same enema tube can be used as an entry point for the material used in the procedure, using the same technique as for vascular accesses, following the steps described in Fig. 1.
Abbocath Teflon needle puncture (Hospira Venisystems, IL 60045 USA). Insertion of the Terumo hydrophilic guide (Terumo Co., Tokyo 151-0072, Japan). Placement of the 7F CORDES introducer (CORDES Co., FL 33014, USA). Progression of the guide and a catheter until surpassing the level of obstruction. Exchanging the hydrophilic guide for a rigid Amplatz Super Staff guide (Boston Scientific, FL 33166, USA). Catheter and introducer removal to allow for passage of the catheter through the rigid guide carrying the Wallflex Enteral® stent (Boston Scientific, Natick MA 01760-1537, USA). Release of the stent 6.9cm or 12cm in length and 25mm in diameter, centred in the stenosis.
Continuous variables were expressed as a mean, median, and range in parentheses. Categorical variables were represented as absolute numbers and percentages. We used the Kaplan–Meier method for the survival analysis, and survival curves were compared using the log-rank test. Statistical significance was set a priori at P<.05 (SPSS 12®, Chicago, IL 60606-6412, USA).
ResultsA total of 93 patients were treated with a colon implant. Of these patients, 69.8% were male (65 men, 28 women) with a mean age of 70years (range: 19–90years). The location of the obstruction was distal to the splenic flexure of the colon in 89 patients and adjacent to it in 4.
The obstruction was complete in 84 patients and incomplete in 9. The on-call interventional radiologist placed the stent in an emergency setting in complete cases, and on a semi-elective basis in incomplete cases.
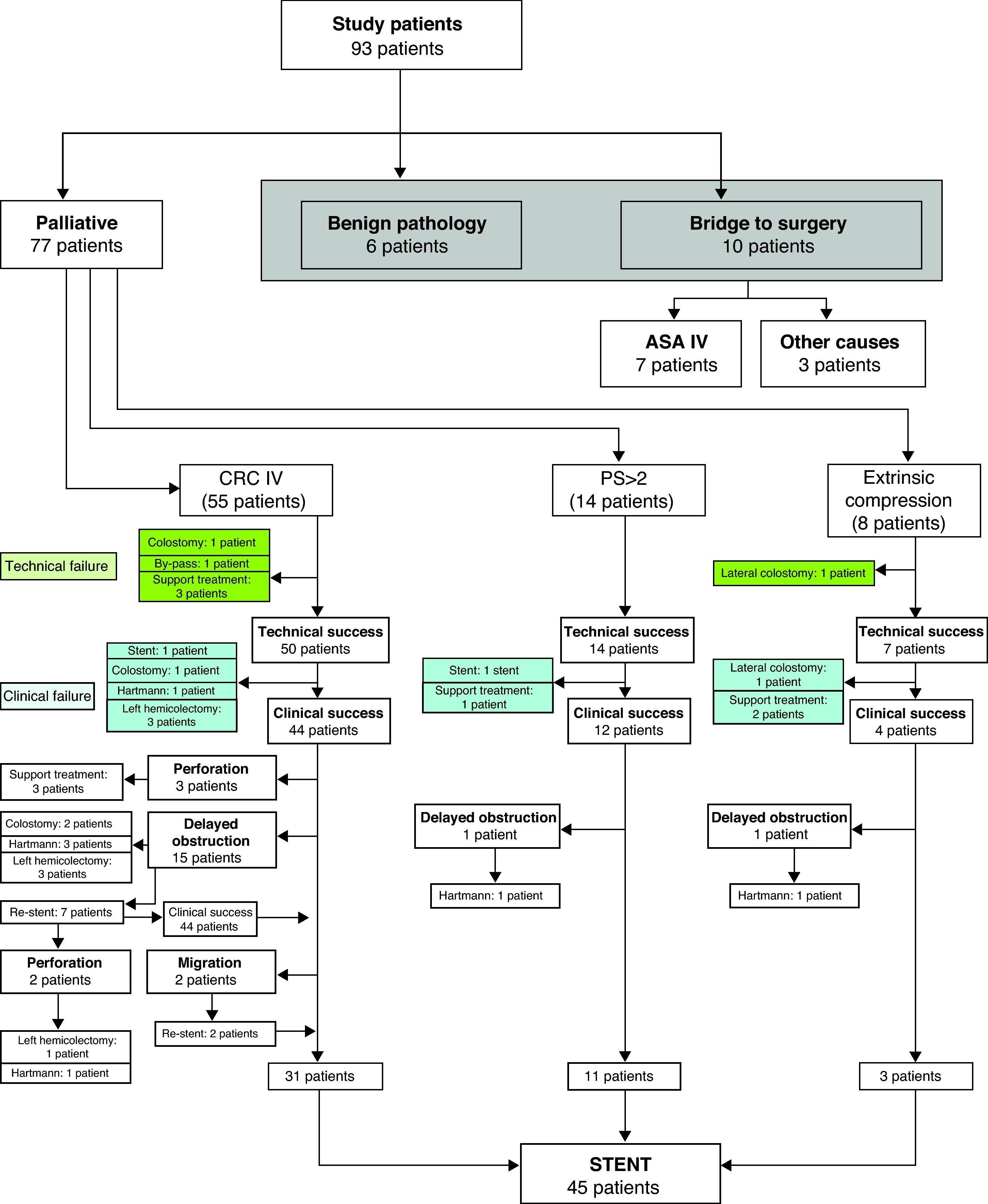
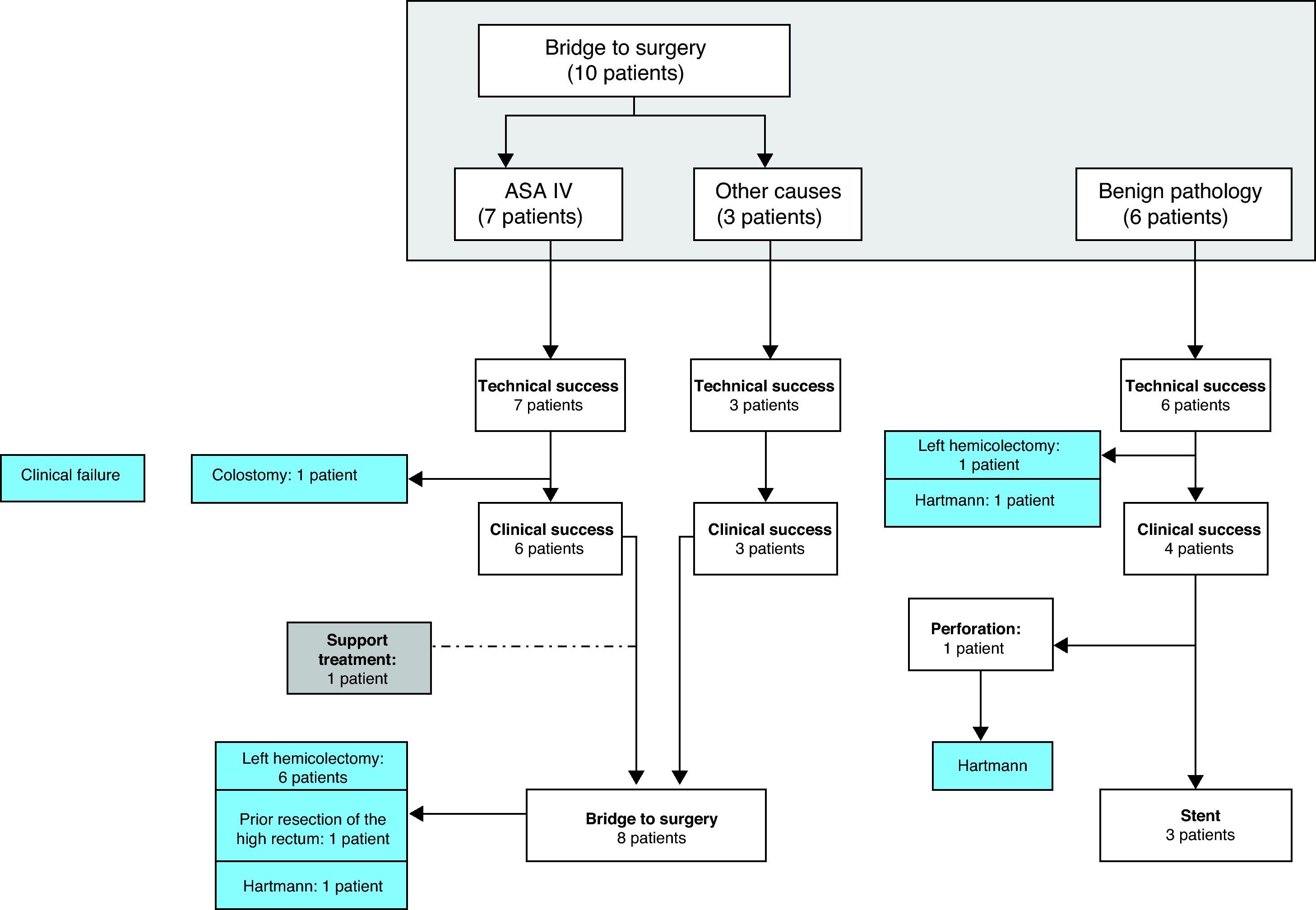
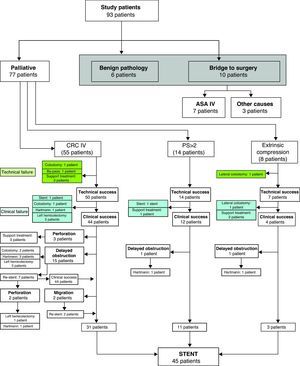
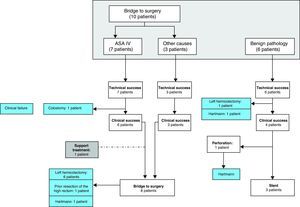
The stent was indicated as a palliative measure in 77 patients (82.7%): 55 for stage IV CRC, 14 for performance status, and 8 for extrinsic compression (Fig. 2). The other indications were: 7 ASA IV patients; 3 ASA III-IV patients who were referred from other hospitals, as a bridge treatment to surgery; and 6 patients with benign conditions (Fig. 3).
The origin of the primary tumour in patients with obstruction due to extrinsic compression was carcinomatosis from colorectal neoplasia in 2 cases, and non-colorectal neoplasia in 3 (gall bladder, stomach, and breast). Three cases were due to direct neoplastic infiltration (cervix: 1, prostate: 2).
Of the 10 patients who received treatment as a bridge to surgery (ASA IV: 7, referred from other hospitals: 3), 8 were surgically treated within 6weeks of placing the stent. One patient died following stent placement due to respiratory failure and another required surgery.
Of the 6 patients with benign obstruction, the stenosis was located at the surgical anastomosis in 5, and the other patient had stenosing diverticular disease.
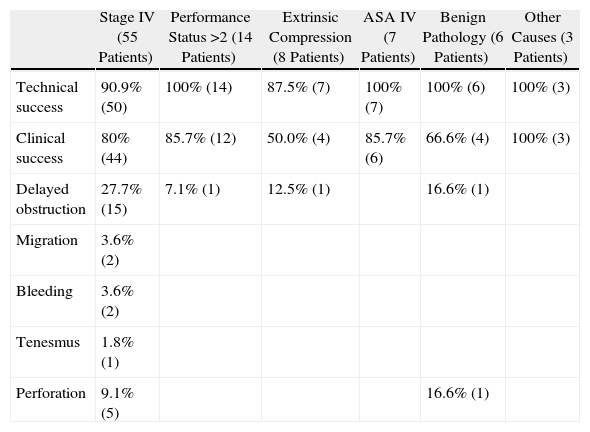
The technical and clinical results, morbidity rates, and management of complications are summarised in Table 1 and Figs. 2 and 3.
Stent Results and Complications.
| Stage IV (55 Patients) | Performance Status >2 (14 Patients) | Extrinsic Compression (8 Patients) | ASA IV (7 Patients) | Benign Pathology (6 Patients) | Other Causes (3 Patients) | |
| Technical success | 90.9% (50) | 100% (14) | 87.5% (7) | 100% (7) | 100% (6) | 100% (3) |
| Clinical success | 80% (44) | 85.7% (12) | 50.0% (4) | 85.7% (6) | 66.6% (4) | 100% (3) |
| Delayed obstruction | 27.7% (15) | 7.1% (1) | 12.5% (1) | 16.6% (1) | ||
| Migration | 3.6% (2) | |||||
| Bleeding | 3.6% (2) | |||||
| Tenesmus | 1.8% (1) | |||||
| Perforation | 9.1% (5) | 16.6% (1) |
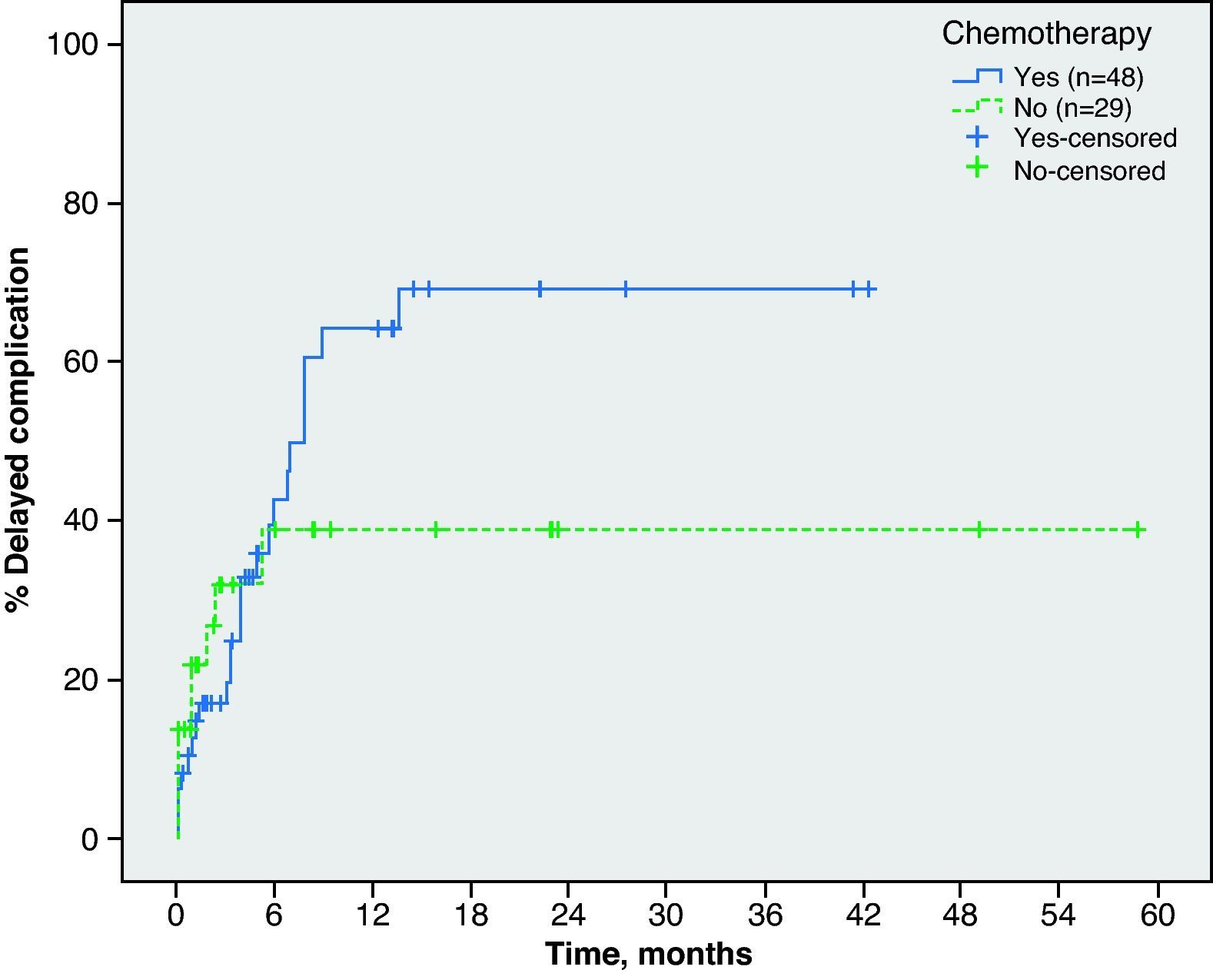
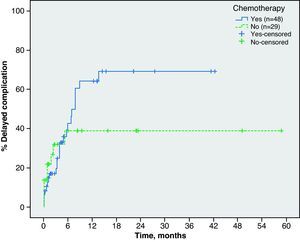
In palliative patients, we examined the possible relationship between the appearance of complications and chemotherapy treatment. After 6months since the stent placement, 46.3% of the 48 patients who received chemotherapy had one or more complications, as compared to 38.9% of the 29 patients who did not receive systemic therapy (P=.458) (Fig. 4). None of the patients with a performance status >2 underwent chemotherapy.
Overall, the procedure was a technical success in 87 patients (93.5%), whereas the clinical success rate regardless of the cause of obstruction was 78.5%.
The incidence of delayed obstruction was 19.3% and the incidence of delayed perforation was 6.4%. Other complications such as migration and GI bleeding occurred in 2.1% of patients, and tenesmus in 1.1% (Table 1).
Lastly, of the 93 patients with indications for a stent, 56 patients (60.2%) were satisfactorily treated with one or more stents. Of the 83 patients whose intended treatment was the placement of a permanent stent, 24 (28.9%) required a surgical procedure. Of these, 17 required an ostomy (1 temporary), with a postoperative mortality rate of 29.1%.
The overall mortality rate in this study was 17.2%, with 16 deaths.
The mean hospitalisation stay was 9.8days (range: 1–46days).
DiscussionFollowing the initial description of using stents to treat distal colon obstruction as a definitive treatment in palliative patients with advanced neoplastic disease (between 2004 and 2009), our strategy was to re-establish intestinal transit by placing an intraluminal stent with the intention of this being a permanent treatment. In this manner, the patient can start or continue palliative chemotherapy, avoiding surgery unless the patient's staging changes due to systemic treatment. In the case of extrinsic colon compression due to a non-resectable tumour, we adopted the same therapeutic attitude, as well as in patients with a high performance status, whose physical condition limits their life expectancy, with the goal of providing the palliative treatment that most effectively controls symptoms.
Another established indication is the use of stents as a decompression treatment in order to avoid the need for emergency surgery and to improve the clinical condition of the obstruction patient.11 Here the goal is to reduce postoperative morbidity and mortality and to facilitate elective laparoscopic resection in a greater percentage of patients.12 This technique is considered safe, with no significant differences in global survival between 3 and 5years compared to the emergency surgery,13–15 in spite of the fact that we still do not know the full consequences of clinically asymptomatic microperforations16 and the presence of tumour cells in the bloodstream after stent placement.17 On the other hand, a recently published multicentre randomised study concluded that colonic stents have no important clinical advantages over emergency surgery.18
Our experience in the use of stents as a bridge to surgery is limited to ASA IV patients with kidney failure, since resection with a primary anastomosis is the primary treatment option in our protocol for intestinal obstruction, except for patients with prognostic factors of postoperative mortality,19 because of the positive short and long-term results demonstrated in emergency surgery.20
The experience with the use of stents to treat benign stenosis is limited, although they have been used to treat stenosing diverticular disease, anastomotic stenosis, radiation stenosis, and Crohn's disease. Results vary with regard to efficacy and safety, with a high rate of complications, making this a treatment recommendable only in certain circumstances.21 Our experience involved only 6 patients, 4 of which had complications requiring surgical treatment.
In spite of the initial enthusiasm surrounding the use of stents as a non-aggressive treatment for patients with malignant colon obstruction, morbidity rates can be high and determine the success of treatment. Even in medical teams with experience in complex endoscopic techniques, morbidity rates can exceed 50%.22 Among the complications stand out migration of the stent and re-obstruction, this last being the most common complication in our study, occurring in 19.3% of cases (27.7% of palliative patients with stage IV CRC), whereas migration only occurred in 4.5% of cases. This difference is probably due to the fact that we do not use covered implants in our hospital. Perforated colon is the most severe complication that can occur during the placement of a stent or after a period of correct functioning, with a varying incidence that can reach 16%.23 Different authors have pointed out the complications produced in patients receiving chemotherapy,9,22,24 but with no clear relationship established with regard to the location or size of the tumour, or the level of obstruction. In our results, the incidence of complications 6months after the stent placement in patients receiving chemotherapy was 46.3%, compared to 38.9% in patients that did not receive systemic treatment, with no statistically significant differences.
Mean survival after a patient has been diagnosed with stage IV CRC and non-resectable metastasis has increased in recent years due to the implementation of new chemotherapy regimens, reaching almost 2years.25 This appears to be related to an increase in the number of complications in patients with colonic stents. We currently know that some of these chemotherapy regimens can produce a histological response with a tumour regression rate as high as 64.3%,26 but we still do not know its direct relationship with complications, in particular tumour perforation. On the other hand, the increased survival rates also increase the length of time in which patients may have a complication.
The mortality rate in our study was 17.2%, and up to 29.1% when complications were treated surgically. These values are higher than those recently published,22 which may be explained by the inclusion of palliative patients in which the treatment of complications was strictly supportive, as well as by the high incidence of severe complications of stents in patients with increased survival.
The management of distal colon obstruction is a complex process, especially in palliative patients, and may be influenced by the geographical location of the patients, the level of experience and specialisation of the surgeon, and the available resources at the hospital.27–29 The use of intracolonic stents as a definitive treatment in palliative patients with and without chemotherapy is a treatment alternative that is not free of complications. We believe that in patients with mortality risk factors and with non-resectable tumour metastasis, this could be the initial treatment of choice. Even so, more prospective, randomised studies are needed to determine the true role of stents in these processes.
Conflict of InterestThe authors have no conflicts of interest to declare.
The authors would like to thank Bernat Miguel, data manager, Unidad Colo-rectal (colorectal unit), Hospital Universitari de Bellvitge and IDIBELL, for managing the data, and Anna Blanco, clinical nurse at the la Unidad Funcional de Cáncer Colo-rectal (colorectal cancer functional unit), Bellvitge University Hospital, for her help in case management.
Please cite this article as: Frago R, et al. Complicaciones del tratamiento de la oclusión del colon distal con prótesis endoluminales. Cir Esp. 2011;89:448–55.