With the purpose of decreasing the existing variability in the criteria of preoperative evaluation and facilitating the clinical decision-making process, our hospital has a protocol of preoperative tests to use with ASA I and ASA II patients. The aim of the study was to calculate the economic impact caused by clinicians’ non-adherence to the protocol for the anaesthesiological evaluation of ASA I and ASA II patients.
MethodsA retrospective study of costs with a random sample of 353 patients that were seen in the consultation for Anesthesiology over a period of one year. Aspects related to the costs, patient's profiles and specialties were analysed, according to the degree of fulfilment of the protocol.
ResultsThe lack of adherence to the protocol was 70%. 130 chest X-rays and 218 ECG were performed without indication. This generated an excess costs of 34 € per patient. Taking into account the expenses of both tests and the attended population undergoing ambulatory surgery during the one-year period, an excess spending for the hospital of between 69,164 € and 83,312 € was estimated.
ConclusionsClinical variability should be reduced and the creation of synergies between the different departments should be enhanced in order to adjust the request for unnecessary complementary tests to decrease health care and to improve the quality of patient care.
Con el propósito de disminuir la variabilidad en la petición de pruebas preoperatorias y facilitar la toma de decisiones, nuestro centro ha establecido un protocolo de pruebas preoperatorias para pacientes ASA I y ASA II tratados mediante cirugía mayor ambulatoria (CMA). El objetivo del estudio fue calcular el impacto económico relacionado con la falta de adherencia de los profesionales al protocolo establecido.
MétodosEstudio de costes retrospectivo con un muestreo aleatorizado simple de 353 pacientes atendidos en la consulta de anestesia durante un año. Se analizaron aspectos relacionados con los costes, así como el perfil de pacientes y especialidades según el grado de cumplimiento del protocolo establecido.
ResultadosLa falta de adherencia al protocolo fue del 70%. Se realizaron 138 radiografías de tórax y 218 electrocardiogramas no indicados, lo que supuso un exceso de coste medio de 34 € por paciente. Teniendo en cuenta el coste de ambas pruebas y la población atendida en CMA durante el año evaluado, la falta de adherencia al protocolo supuso un exceso de coste anual para el centro entre 69.337 € y 84.727 €.
ConclusionesEs preciso reducir la variabilidad clínica y favorecer la creación de sinergias entre los diferentes servicios para adecuar la petición de pruebas complementarias, disminuir los costos de la atención y mejorar la calidad asistencial.
The objective of preoperative evaluations is to provide information about the physical and mental health status of patients, to assess their risks for anaesthesia/surgery, and to outline a plan for anaesthesia/analgesia as well as perioperative care. As the physical status of patients correlates with different surgical risks in the American Society of Anesthesiologists (ASA) classification,1 it is necessary to properly select and evaluate patients to undergo surgical intervention. Hence, anaesthesia evaluations include a series of diagnostic tests in order to detect previously undiagnosed diseases, thereby guaranteeing that the patient has met certain safety criteria before surgery. These tests, however, are often routinely requested, with no specific clinical indication, based on the erroneous concept that they are a substitution for proper patient medical history and physical examination.2 These tests are an unnecessary expense, have questionable diagnostic value, are generally useless, and their impact on the final results of the operation is very limited. Meanwhile, patients are being subjected to studies that are not free of risks themselves. This reduces the quality of the healthcare received while considerably increasing costs per patient, in addition to other indirect costs such as travel expenses, lost productivity at work, etc. Although many preoperative tests are low cost, if we consider the elevated number of patients treated who are classified as ASA I and II, the final result is a needless expenditure of millions of euros for the public healthcare system.3 With the current search for ways to guarantee the sustainability of the Spanish national healthcare system, increased efficacy in the administration of these resources is a highly relevant goal.
The protocol for ordering preoperative studies at our centre is based on the recommendations of the Spanish Society for Anaesthesia, Reanimation and Pain Therapy and the Spanish Association of Major Ambulatory Surgery. The protocol establishes the criteria by which diagnostic tests should be requested for patients who are scheduled for low-risk surgery, according to ASA grade. At our hospital, this information had been distributed to all the surgical departments that conduct major ambulatory surgery (MAS).
Although many studies have discussed the existence of great variability in performing the same procedure within the healthcare system of our country, to our knowledge there have been no studies estimating the cost attributable to the variability in preoperative evaluations for MAS.
The main objective of this study was to calculate the economic impact associated with clinical variability and lack of adherence to the protocol established in our hospital for the anaesthesia evaluation of ASA I and II patients. As a secondary objective, the authors proposed to report and analyse patient profiles and surgical specialties according to the degree of protocol compliance.
MethodsWe conducted a retrospective cost minimisation study using a simple randomised sample of cases that had been treated in the anaesthesia consultation of the MAS unit over a period of 12 months (June 2012 – May 2013).
Regarding preoperative testing, the protocol establishes that patients classified as ASA I and II who are scheduled for low-risk surgery (usually ambulatory procedures) should have complete blood work-up with coagulation, glycemia, creatinine, urea and ions. In patients over the age of 45 and heavy smokers (more than 20 cigarettes/day), chest X-ray should be ordered (CXR). Systematic electrocardiogram (ECG) was not recommended in ASA I or II patients. With these minimal recommendations, the anaesthesiologist in charge of the preoperative evaluation of a patient could decide whether to order other complementary studies, if necessary.
A cost minimisation analysis had been used to assess alternatives with the same effectiveness and same healthcare result, and the protocol of our hospital was considered the least expensive alternative.
The pilot study, which included an independent sample of 76 patients, showed that in 65% (95%CI 56–74) of cases the protocol had not been correctly applied. The estimated sample size (322) was then calculated according to the prevalence of Non-compliance with the protocol (patients in whom the established protocol was not followed over the total number of cases analysed) for a finite population and an absolute precision of 5%, with a 95% confidence interval. To avoid possible losses, the sample size was increased by 10% (353).
Data were collected from a review of computerised medical files, the anaesthesia unit records (specific application of the Anaesthesia and Recovery Department) and anaesthesia office visit forms. The costs of the complementary tests were obtained from the analytical accounting system at our hospital.
Included for study were those patients evaluated in the anaesthesia unit for MAS during the study period. All had undergone a complete anaesthesia evaluation and medical history. ASA III and IV patients were excluded. The study protocol was approved by the Ethics Committee for Clinical Research at our hospital in September 2013 (code 228/13).
We recorded patient demographic data, ASA physical status, preoperative tests (CXR and ECG), medical history, and the surgery department requesting preoperative evaluation. Given these data, we assessed the correct or incorrect application of the protocol.
We applied to each patient the excess cost of these tests (CXR or ECG) that had been ordered without having been indicated by the protocol, and we calculated the mean cost per patient in whom the protocol had not been followed. The percentage of Non-compliance with the protocol was calculated overall and for each variable of interest. To estimate the excess annual cost, we created 2 extreme scenarios utilising the upper and lower limits of the confidence intervals for the variables defining cost: one scenario of minimal annual cost, resulting from a minimal Non-compliance with the protocol and a minimal number of ASA I and II patients treated in one year (lower limits of the 95%CI); and, another scenario of maximum annual cost, resulting from a maximum Non-compliance with the protocol and a maximum number of ASA I or II patients treated in one year (upper limits of the 95%CI).
- a)
Minimal excess annual cost=patients treated in one year×(lower limit of the 95%CI for ASA I–II patients)×(lower limit of the 95%CI of non-protocol ASA I–II patients)×(mean cost per patient in whom the protocol was not followed).
- b)
Maximum excess annual cost=patients treated in one year×(upper limit of the 95%CI for ASA I–II patients)×(upper limit of 95%CI for non-protocol ASA I–II patients)×(mean cost per patient in whom the protocol was not followed).
We completed a descriptive analysis of the variables. Percentages and means were calculated for the categorical variables, and standard deviation and 95% confidence interval were used for the quantitative variables. We determined the total number and percentage of patients in whom the established protocol was not adhered to for preoperative studies. The characteristics of the patients associated with Non-compliance with the protocol were studied with a difference in proportions test (Chi-squared) for the categorical variables and means (Student's t) for the quantitative variables, with previous confirmation of their normal distribution.
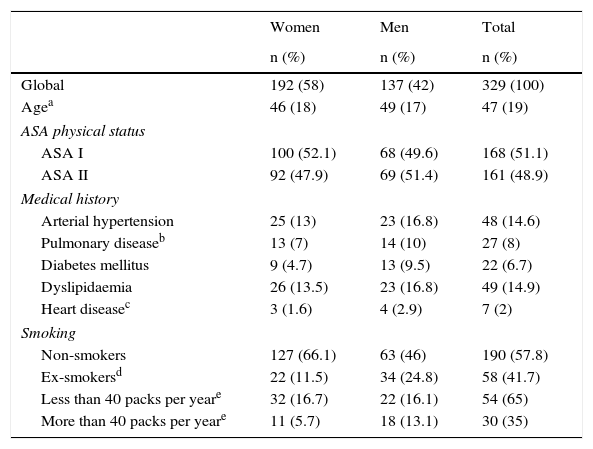
ResultsOur study included 353 patients, 329 of which (93.2%; 95%CI: 90.1–95.4) belonged to ASA physical status classes I and II. The population characteristics studied are described in Table 1. The remaining 6.8% were ASA III and therefore excluded from the study.
General Patient Characteristics According to Sex.
| Women | Men | Total | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Global | 192 (58) | 137 (42) | 329 (100) |
| Agea | 46 (18) | 49 (17) | 47 (19) |
| ASA physical status | |||
| ASA I | 100 (52.1) | 68 (49.6) | 168 (51.1) |
| ASA II | 92 (47.9) | 69 (51.4) | 161 (48.9) |
| Medical history | |||
| Arterial hypertension | 25 (13) | 23 (16.8) | 48 (14.6) |
| Pulmonary diseaseb | 13 (7) | 14 (10) | 27 (8) |
| Diabetes mellitus | 9 (4.7) | 13 (9.5) | 22 (6.7) |
| Dyslipidaemia | 26 (13.5) | 23 (16.8) | 49 (14.9) |
| Heart diseasec | 3 (1.6) | 4 (2.9) | 7 (2) |
| Smoking | |||
| Non-smokers | 127 (66.1) | 63 (46) | 190 (57.8) |
| Ex-smokersd | 22 (11.5) | 34 (24.8) | 58 (41.7) |
| Less than 40 packs per yeare | 32 (16.7) | 22 (16.1) | 54 (65) |
| More than 40 packs per yeare | 11 (5.7) | 18 (13.1) | 30 (35) |
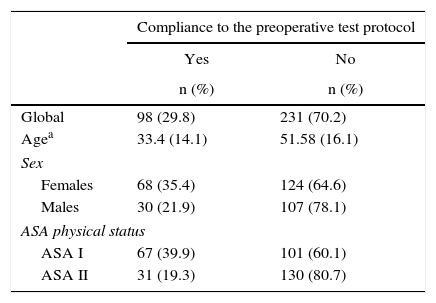
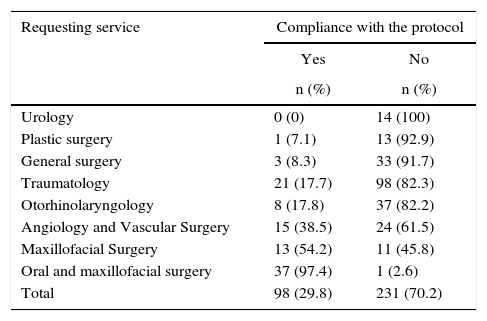
Overall, Non-compliance with the protocol was observed in 70% (95%CI: 65–75) of cases (Table 2). The departments with higher non-compliance rates were Urology, Plastic and Reconstructive Surgery and General Surgery, in which 100, 93 and 92% of patients were not evaluated according to the protocol, respectively. The Oral and maxillofacial surgery Department, on the other hand, presented a non-compliance rate of only 3% (Table 3).
Compliance With the Protocol for Requesting Preoperative Tests According to Age, Sex and Physical Status.
| Compliance to the preoperative test protocol | ||
|---|---|---|
| Yes | No | |
| n (%) | n (%) | |
| Global | 98 (29.8) | 231 (70.2) |
| Agea | 33.4 (14.1) | 51.58 (16.1) |
| Sex | ||
| Females | 68 (35.4) | 124 (64.6) |
| Males | 30 (21.9) | 107 (78.1) |
| ASA physical status | ||
| ASA I | 67 (39.9) | 101 (60.1) |
| ASA II | 31 (19.3) | 130 (80.7) |
Compliance With the Protocol According to the Surgical Service Requesting Preoperative Anaesthesia Evaluation.
| Requesting service | Compliance with the protocol | |
|---|---|---|
| Yes | No | |
| n (%) | n (%) | |
| Urology | 0 (0) | 14 (100) |
| Plastic surgery | 1 (7.1) | 13 (92.9) |
| General surgery | 3 (8.3) | 33 (91.7) |
| Traumatology | 21 (17.7) | 98 (82.3) |
| Otorhinolaryngology | 8 (17.8) | 37 (82.2) |
| Angiology and Vascular Surgery | 15 (38.5) | 24 (61.5) |
| Maxillofacial Surgery | 13 (54.2) | 11 (45.8) |
| Oral and maxillofacial surgery | 37 (97.4) | 1 (2.6) |
| Total | 98 (29.8) | 231 (70.2) |
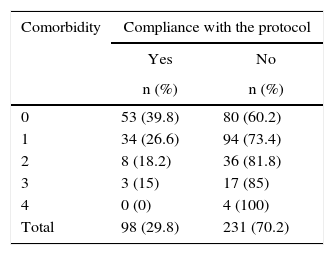
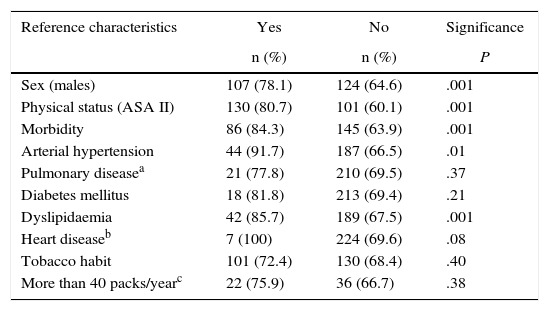
With regards to patient characteristics, Non-compliance with the protocol occurred in a higher percentage of men than in women (P<0.001) and in more ASA II patients than ASA I (P<0.001). Likewise, it was observed that, in hypertensive and in dyslipidaemic patients, Non-compliance with the protocol was higher compared to those who did not present these characteristics (P<.001). The mean age of the patients in whom the protocol was not followed was 51.5±16.1, while the mean age of patients in whom the protocol was followed was 33.4±14.1. This difference was statistically significant (P<.001). No statistically significant differences were found in smokers, diabetics, or those with pulmonary or heart diseases (Table 6). Meanwhile, a directly proportional relationship was found between Non-compliance with the protocol and the number of patient comorbidities (Table 4).
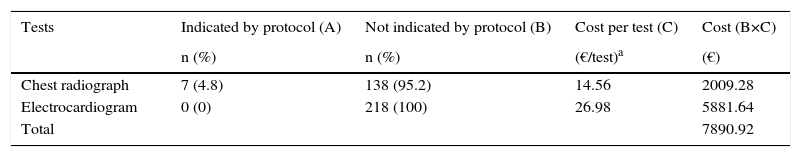
As for the preoperative studies, a total of 138 CXR and 218 ECG were ordered without indication (see Table 5).
Tests Done According to the Protocol and Associated Cost.
| Tests | Indicated by protocol (A) | Not indicated by protocol (B) | Cost per test (C) | Cost (B×C) |
|---|---|---|---|---|
| n (%) | n (%) | (€/test)a | (€) | |
| Chest radiograph | 7 (4.8) | 138 (95.2) | 14.56 | 2009.28 |
| Electrocardiogram | 0 (0) | 218 (100) | 26.98 | 5881.64 |
| Total | 7890.92 |
Percentage of Non-compliance With the Protocol According to the Presence (Yes) or Absence (No) of Reference Characteristics.
| Reference characteristics | Yes | No | Significance |
|---|---|---|---|
| n (%) | n (%) | P | |
| Sex (males) | 107 (78.1) | 124 (64.6) | .001 |
| Physical status (ASA II) | 130 (80.7) | 101 (60.1) | .001 |
| Morbidity | 86 (84.3) | 145 (63.9) | .001 |
| Arterial hypertension | 44 (91.7) | 187 (66.5) | .01 |
| Pulmonary diseasea | 21 (77.8) | 210 (69.5) | .37 |
| Diabetes mellitus | 18 (81.8) | 213 (69.4) | .21 |
| Dyslipidaemia | 42 (85.7) | 189 (67.5) | .001 |
| Heart diseaseb | 7 (100) | 224 (69.6) | .08 |
| Tobacco habit | 101 (72.4) | 130 (68.4) | .40 |
| More than 40 packs/yearc | 22 (75.9) | 36 (66.7) | .38 |
The total excess cost in the sample studied was €7890.92. The number of patients of the sample in whom the protocol was not followed was 231, and the mean excess cost per patient due to non-compliance was €34.16 (95%CI: 33.06–35.26).
According to our calculations, the minimum annual excess cost due to non-compliance with the protocol was €69,163.91, while the maximum annual excess cost was €83,312.48.
- a)
Minimum annual excess cost=3423 patients treated×(0.91 ASA I–II patients/patients treated)×(0.65 patients with protocol non-compliance/ASA I–II patients)×(€34.16/patients with protocol non-compliance)=€69,163.91.
- b)
Maximum annual excess cost=3423 patients treated×(0.95 ASA I–II patients/patients treated)×(0.75 patients with protocol non-compliance/ASA I–II patients)=2448×(€34.16/patient with protocol non-compliance)=€83,312.48.
The main findings of this study have been the limited adherence to the protocol by the surgery units in a population of healthy patients proposed for low-risk ambulatory surgical procedures, and the consequent increase in costs incurred by our hospital. Several reasons, such as tradition, inertia, fear of medical or legal repercussions, etc., together with the demonstrated slowness with which scientific advances are implemented in daily clinical practice,4,5 may explain these results.
As for CXR, there is no evidence that its use improves postoperative results, not even in patients with a risk of perioperative pulmonary complications. Most authors concur that these tests should be limited to patients in whom new symptoms or signs are observed, in terminal renal failure, decompensated heart failure and when the results are expected to influence clinical management.6–9 In our study, only 5% of the patients had indications for this test, meaning that the remainder were unnecessarily exposed to radiation and expenses were unnecessarily incurred. We are not aware of whether this test may have led to changes in the anaesthesia approach for the patients of the sample, as this aspect was not an objective of our study.
ECG, which is not indicated in ASA I and II patients, was likewise done in a considerable percentage of patients (66%). The hospital protocol established very specific criteria for its use, which coincide with the most widely accepted guidelines from the American Heart Association and European Society of Cardiology, according to which ECG is considered an intervention that is not useful and may even be harmful.10,11 Other groups argue that its use can be contemplated in patients over the age of 65, unless there are other ECG results from the previous year,12 or in ASA II patients with cardiovascular disease, or when the patient is taking cardiotoxic drugs or presents mild renal or respiratory disease.13 With this perspective, the associated diseases of ASA II patients could have justified the use of ECG in 17% of the cases.
The protocol allowed for lab work-ups. Although rarely indicated in healthy patients by other publications, coagulation studies should be done in patients with a history of haemorrhage and hematomas, liver disease or metastasis, severe malnutrition, vitamin K deficiency and treatment with anticoagulant drugs.14,15
Among the surgery services evaluated, compliance with the protocol was quite higher in the specialty of oral and maxillofacial surgery. Even though all the patients studied had low anaesthetic risk, because of the differential characteristics of the patients treated in the oral and maxillofacial surgery unit (young population with a mean age of 24, lower morbidity rate and usually treated with wisdom tooth extraction), it is possible that the anaesthesia risk perceived by the staff is lower than that of other specialties. This lower perception of risk could lead to fewer diagnostic tests being ordered for preoperative evaluation when compared to other surgical services. The authors are unaware of other studies dealing with this topic, so it should be explored in future research.
The recommended guidelines were more frequently followed in ASA I patients and those with fewer comorbidities. The results observed according to associated diseases show that only in patients with hypertension or dyslipidaemia was there less protocol compliance; no correlation was found with other diseases such as asthma, chronic obstructive pulmonary disease or diabetes. It is difficult to justify these findings because, although the surgeons may have considered that more studies were justified in hypertensive patients, other systemic disease like diabetes should have been considered similarly. Despite having found no differences in the application of the protocol between non-smokers and smokers, adherence to the protocol did seem to be lower in patients who smoked more than 40 packs per year and in ex-smokers, probably because they had stopped smoking due to other comorbidities.
The estimated cost involved in doing these extra tests was considerable. Nonetheless, this cost can vary depending on the indicator selected. Although the costs were estimated for ASA I and II patients in whom the protocol was not followed, as we have seen, the adherence varies between patients from the two groups and perhaps the cost for each group could have been calculated in greater detail. However, as the same protocol is applied to both groups, we felt it was better to calculate the costs jointly.
Since this study has been conducted with an eye on costs from the standpoint of healthcare providers, it is necessary to comment that other indirect costs have not been taken into consideration. For instance, we did not calculate the consumption of resources derived from the implementation of a new policy for ordering tests (informing staff and promoting the protocol, training sessions, etc.). Furthermore, we also did not contemplate the derived indirect costs, such as the loss of productivity and travel expenses of patients and their families in order to have unnecessary tests such as those described, including the needless radiation of patients treated with CXR. In spite of this, we believe that the results of our study can be useful to assess potential savings and the feasibility of a policy aimed at reducing clinical variability in the situation described.
This study has detected a high lack of compliance by staff with the protocol for preoperative evaluation testing in patients with low anaesthesia risk treated in the MAS setting. This was especially significant in male patients who were of older age, ASA II and had some sort of morbidity. The economic impact was important and avoidable.
We, the authors, support implementing and promoting strategies based on continuous evaluation of the practices and policies for ordering preoperative tests at different hospitals. Quantitative studies are recommended to help determine the excess cost attributable to this phenomenon. Qualitative studies including medical professionals as well as patients would also provide more information about the factors implicated in the lack of protocol compliance, thereby identifying critical points where intervention is necessary. It is essential to improve the understanding and training of medical professionals involved in this process to improve the application of current protocols. These actions can promote the reduction in clinical variability while improving healthcare costs, quality of care and safety of our patients.
AuthorshipGil-Borrelli was responsible for the study design, analysis and interpretation of the data and writing of the manuscript. Agustí and Zaballos were involved in the study design and data acquisition/collection. Pla and Díaz contributed with the data analysis and interpretation, as well as the critical review and final approval of the manuscript.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Gil-Borrelli CC, Agustí S, Pla R, Díaz-Redondo A, Zaballos M. Economic impact of clinical variability in preoperative testing for major outpatient surgery. Cir Esp. 2016;94:280–286.
Part of this study was used in 2 oral communications presented at the Spanish Society for Quality Healthcare Conference held in October 2014, in Madrid, under the title: Quality and efficiency of anaesthesia evaluations for major ambulatory surgery in ASA I and II patients.