Sarcomas are mesenchymal tumors that affect the retroperitoneum in 15% of cases.1,2 28% of sarcomas originate in smooth-muscle cells, and are called leiomyosarcomas2; 2% of which are vascular in origin.3
There are currently close to 300 published cases of retroperitoneal leiomyosarcomas that are vascular in origin4; most of these arise from the middle segment of the inferior vena cava1 and are usually locally aggressive tumors.
We present the case of a 73-year-old male with no prior medical history of interest that came to our consultation complaining of abdominal pain in the right upper quadrant and flank, of one-month duration accompanied by a sensation of postprandial fullness. During physical examination, a non-painful abdominal mass was palpated in the right flank. Abdominal ultrasound revealed a subhepatic heterogeneous mass measuring 30cm that occupied the right hemi-abdomen, and compressed the hepatic hilum and displaced the right kidney.
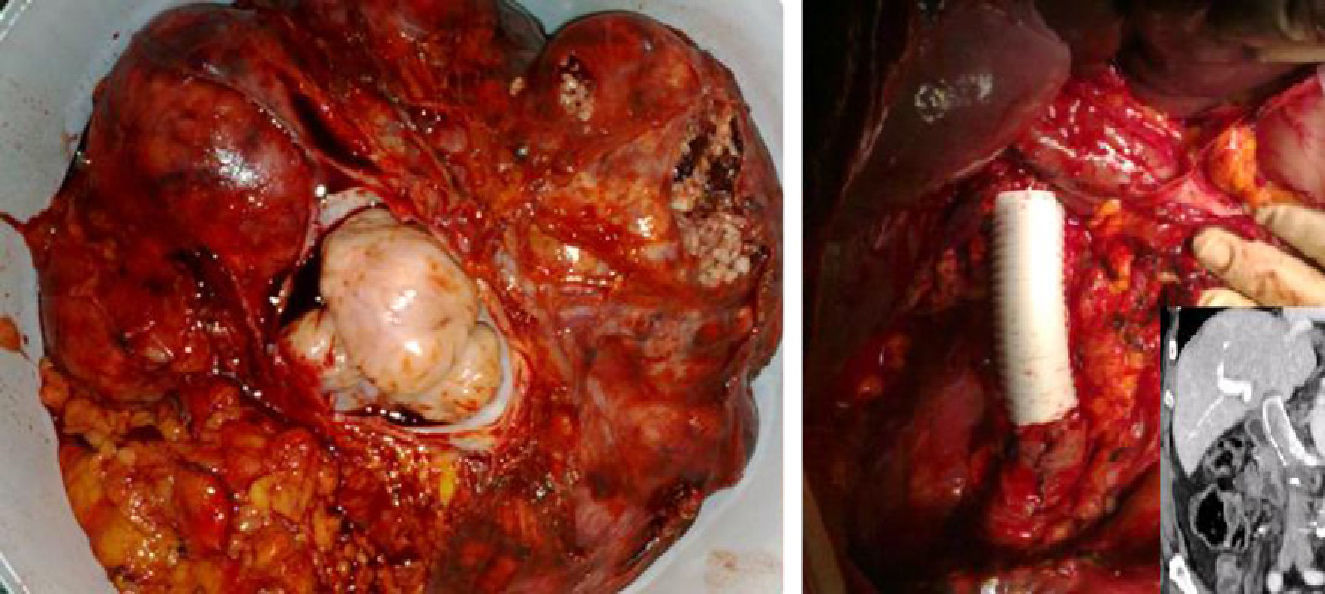
Abdominal CT showed a solid 30-cm mass with heterogeneous contrast uptake which displaced the adjacent structures and areas of necrosis in the interior, permeable inferior vena cava and a 3-cm lesion in segment iv of the liver compatible with hepatic metastasis (Fig. 1). Positron emission tomography (PET) demonstrated hypermetabolic areas in the mass described and the liver lesion of segment iv.
In the percutaneous biopsy sample, fragments of mesenchymal tissue with fusiform cells with elongated cytoplasm were observed, some with irregularly shaped atypical nuclei; immunohistochemistry was positive for vimentin, alpha smooth muscle actin, desmin and S100 protein, and negative for cytokeratins (AE1-AE3) and CD117 (C-KIT), compatible with leiomyosarcoma.
The patient was treated surgically, confirming the diagnosis of retroperitoneal leiomyosarcoma in the right hemi-abdomen measuring 40cm in diameter with important collateral vascularization that infiltrated the inferior vena cava, renal vein and right kidney, in addition to a metastatic lesion in segment iv. The tumor was resected en bloc together with the right kidney, with resection of the inferior vena cava (respecting the left renal vein) and substitution with a ringed polytetrafluoroethylene (PTFE) prosthesis measuring 10cm in length (Fig. 2), with end-to-end proximal and distal anastomoses using a continuous polypropylene suture. Due to intraoperative hemodynamic instability, it was decided to treat the liver metastasis at another time.
The pathology study confirmed the diagnosis of high-grade leiomyosarcoma originating in the inferior vena cava with endoluminal growth and disease-free resection margins. The pathology report concurred with the immunohistochemical staining pattern of the preoperative biopsy.
Four weeks afterwards, a left hepatectomy was performed, which confirmed the diagnosis of liver metastasis of leiomyosarcoma in segment iv, with disease-free resection margins.
The patient is currently being followed in the ambulatory setting and is disease free 8 months after the initial procedure.
Primary leiomyosarcomas of the inferior vena cava are rare, slow-growing malignant tumors that present non-specific symptoms such as abdominal pain, palpable abdominal mass or edemas of lower extremities in cases of obstruction of the vena cava. In cases of renal affectation, they may cause renal vein thrombosis, nephrotic syndrome and/or arterial hypertension.1 Due to the lack of symptoms, by the time these tumors are diagnosed they are usually large-sized masses that affect adjacent structures.
Survival depends on complete resection, which can be difficult due to the location and the involvement of vascular structures and neighboring organs.4,5
The only curative option is a complete resection of the tumor, as it is not very sensitive to chemo- or radiotherapy. It is usually necessary to perform large retroperitoneal dissections for complete resection of the tumor. If there is involvement of the inferior vena cava, segmental resection is necessary, requiring the ligation of multiple collateral veins and, if the flow is preserved in the inferior vena cava, reconstruction is necessary with prosthetic materials. PTFE is the most commonly used material since it achieves adequate long-term results, with infection and thrombosis being the most frequent complications. The use of ringed prostheses reduces the risk of thrombosis by avoiding compression.4
The sarcoma classification of the AJCC/UICC is based on the size of the primary tumor (T) and its depth (a or b), the presence of infiltrated lymph nodes (N) or metastasis (M) and histologic grade (G). Nonetheless, the three most important prognostic factors for retroperitoneal sarcomas are the possibility of R0 resection, histologic grade and the presence of metastasis.2,6
The prognosis is poor: mean 5-year survival post-resection is 28%–34%1–3; the incidence of metastasis and local recurrence is 36%.1 Complete resection combined with adjuvant therapies are the best therapeutic strategy in these patients.
In conclusion, since the prognosis of patients diagnosed with retroperitoneal leiomyosarcoma depends on the possibility of complete tumor resection, an aggressive therapeutic approach from a surgical standpoint is warranted, occasionally requiring multiple-organ resection and vascular reconstruction with prosthetic material.
Please cite this article as: Carvajal López F, García Domingo MI, Herrero Fonollosa E, Camps Lasa J, Cugat Andorrà E. Leiomiosarcoma de vena cava inferior con metástasis hepática. Resección multiorgánica con reconstrucción vascular. Cir Esp. 2013;91:394–395.