Annular pancreas is a rare congenital anomaly that is usually diagnosed in newborns. Its diagnosis in adults is uncommon and is one of the few congenital anomalies of the gastrointestinal tract that can debut with symptoms in adults.1
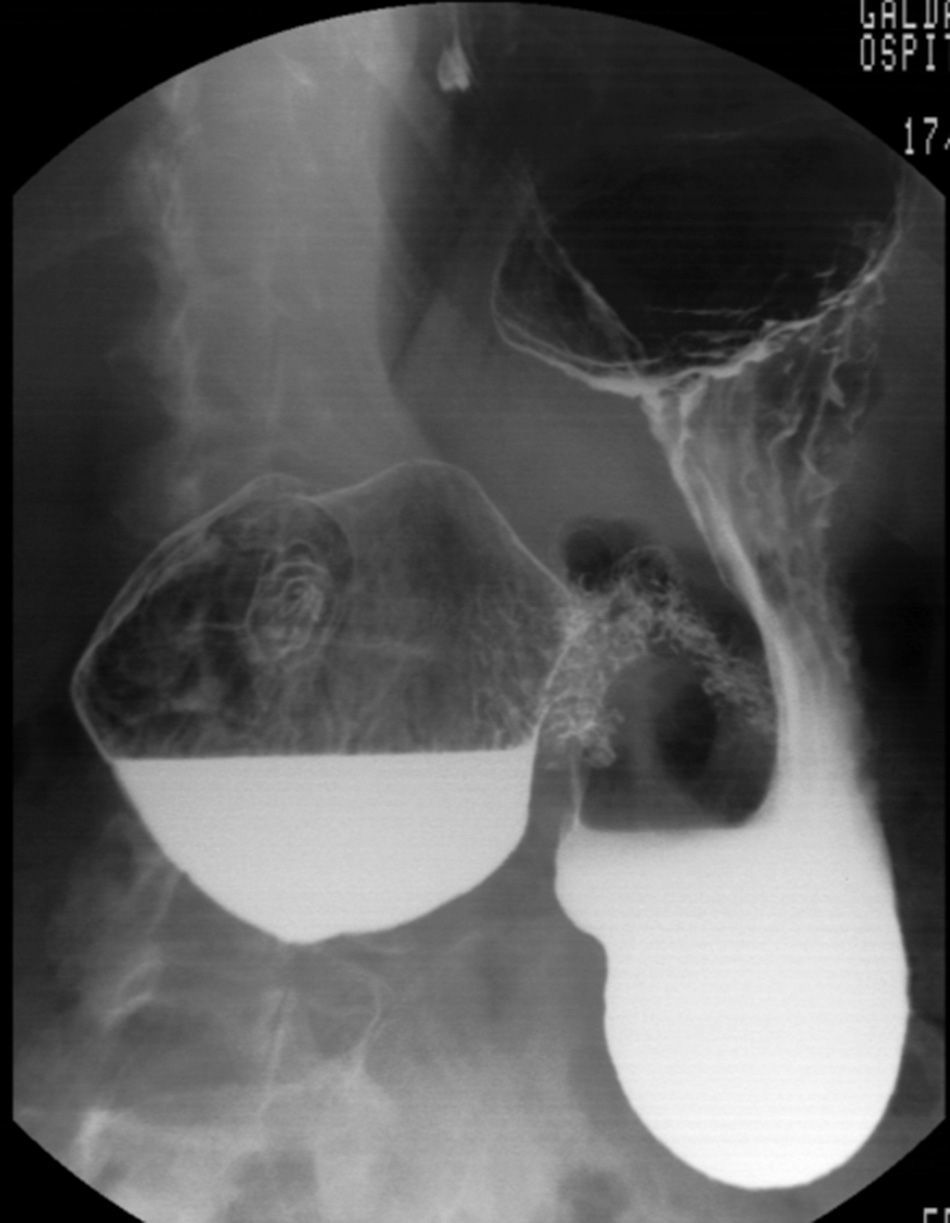
We present the case of a 65-year-old woman who reported ongoing dyspepsia and vomiting episodes over the prior 2–3 months. Gastroscopy demonstrated stenosis of the second portion of the duodenum due to an extrinsic compression. Both the barium contrast study (Fig. 1) as well as CT demonstrated dilatation of the duodenal bulb, with difficult passage of the contrast to the rest of the duodenum and stenosis of the proximal second portion of the duodenum, suggestive of annular pancreas. MRI confirmed the diagnosis of annular pancreas encompassing the second portion of the duodenum.
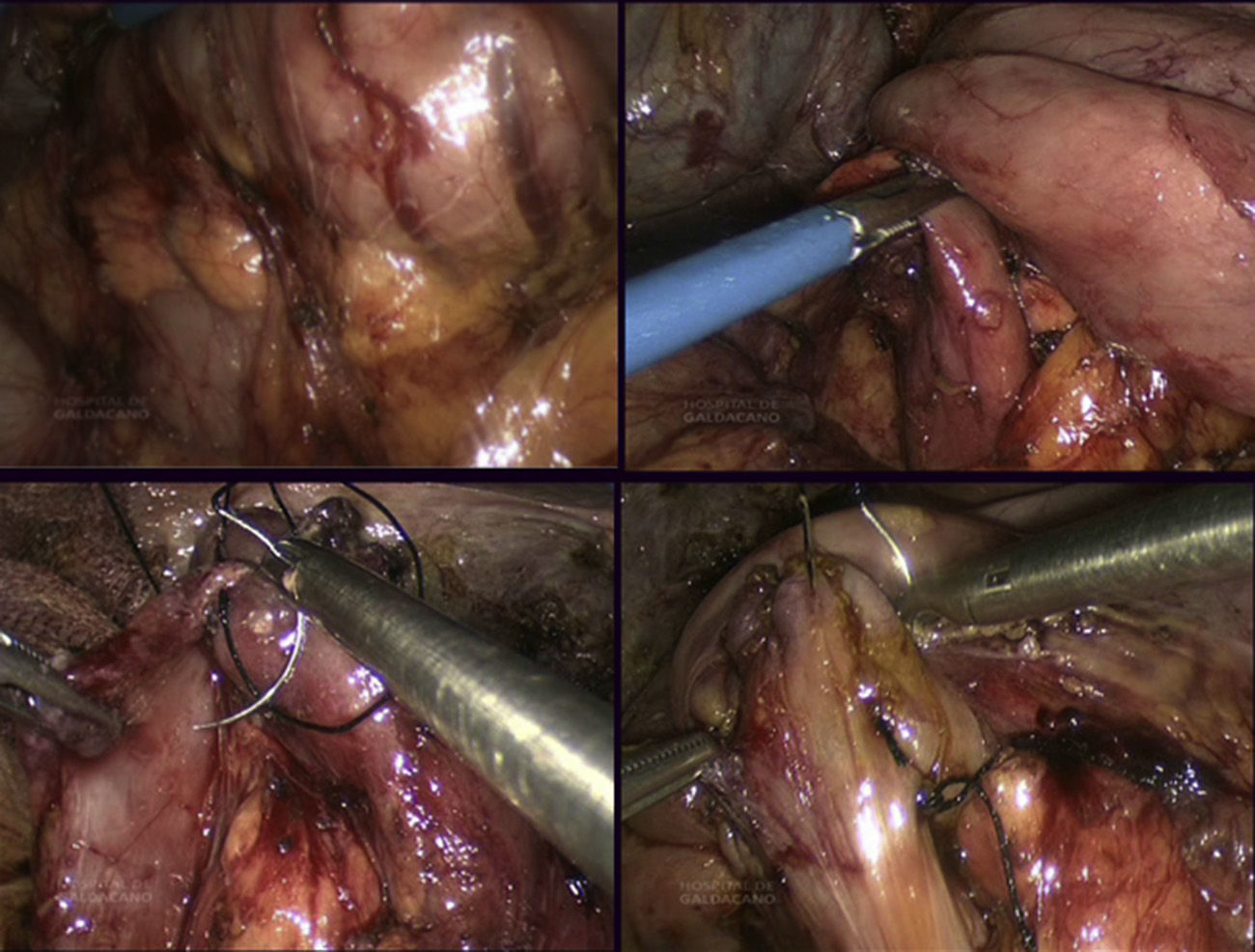
With this diagnosis, the patient underwent laparoscopic surgery in the French and anti-Trendelenburg positions, with the surgeon standing between the legs. The optics used were 0°, and 4 trocars were situated in the upper right quadrant (2×12mm, supraumbilical and anterior axillary line; 2×5mm, right subxiphoid and mean axillary line). Laparoscopy confirmed the preoperative findings of dilatation of the first duodenal portion and pancreatic tissue surrounding the second portion. After an extensive Kocher maneuver, a monoplane manual side-to-side duodenoduodenal anastomosis was created with 2/0 silk sutures (Fig. 2). The postoperative period was uneventful and the patient was discharged on the fifth day after having tolerated oral intake. Currently, after a two-year follow-up, the patient continues to be asymptomatic.
The incidence of annular pancreas is one out of every 12000–15000 newborns and one out of every 70 children born with Down syndrome.2 In more than 70% of cases, it is associated with other malformations such as atresia or duodenal stenosis, intestinal malrotation, esophageal atresia and cardiovascular anomalies.2 Its diagnosis in adults is uncommon (3 out of 20000 autopsies)3 and is made during the study of a duodenal obstruction.
In adults, only 33% of cases are symptomatic,1 which depends on the degree of stenosis caused by the ring of pancreatic tissue and its location. The main form of presentation is vomiting, which in 90% of cases is the vomiting of food, and not bilious vomiting, because the most frequent location is preampullary.2 Other types of presentations are pancreatitis, peptic ulcer and obstructive jaundice. An association has also been demonstrated with pancreatic and bile duct tumors.1,4
In children, the diagnosis is usually established with prenatal ultrasound when polyhydramnios and images of double bubbles are observed, typical of duodenal obstruction.2 In adults, intestinal obstruction is studied by means of gastroscopy, barium swallow, CT, MRI and/or ERCP. Proximal dilatation of the duodenum, compression defect of the 2nd portion and distal narrowing are observed. However, in a review by Urayama et al.,5 in 40% of cases the definitive diagnosis was confirmed at the time of surgery. With the development and evolution of imaging techniques, this percentage is dropping.
The treatment of choice is surgical, and a large variety of surgical techniques as well as endoscopic procedures have been described.5 Having ruled out dissection of the pancreatic ring due to the high rate of pancreatic fistulas, the most common technique is bypass, be it gastrojejunal, duodenojejunal or duodenoduodenal.
Today, all of these anastomoses can be done laparoscopically.6–8 In our opinion, the duodenoduodenal bypass is the best option, when feasible, as it avoids the biliary gastric reflux of the gastrojejunal technique and the probability of blind loop syndrome of the duodenojejunal option.7,8
Duodenoduodenal anastomosis can be performed following the Kimura diamond technique9 or side-to-side, as in our patient. Some authors believe that this anastomosis is more difficult in adults6 because the duodenum is less mobile; in fact, we have found no cases in the literature describing the laparoscopic technique in adults. However, we believe that chronic obstruction of the second duodenal portion makes the first portion very dilated, which facilitates the duodenoduodenostomy technique after extensive duodenal mobilization using a Kocher maneuver.
As for prognosis, in children it depends on the association with other malformations. In adults, there are authors that recommend pancreaticoduodenectomy due to the high risk of a coexisting pancreatic neoplasm, especially if there is bile obstruction. If not, a very close, life-long follow-up is necessary due to the high risk for malignant degeneration.
Please cite this article as: Badiola I, Las Navas E, Sanz A, Estraviz B, Ibañez FJ. Duodenoduodenostomía laterolateral laparoscópica por páncreas anular del adulto. Cir Esp. 2014;92:630–631.
A video of this surgery was presented at the 29th Spanish National Congress of Surgery.