Mucinous tumors of the appendix are a rare pathology, with a prevalence below 0.5%. Clinical presentation usually occurs during the sixth decade of life, and mucinous tumors can clinically mimic acute appendicitis. The aim of this study is to describe the clinical and demographic variables, therapeutic procedure and diagnosis of these tumors. We analyze the association between mucinous tumors and pseudomyxoma peritonei (PP), as well as the association with colorectal and ovarian tumors.
MethodsA retrospective study was performed including patients who underwent an appendectomy between December 2003 and December 2014.
ResultsSeventy-two mucinous tumors of the appendix were identified among 7717 patients reviewed, resulting in a prevalence of 0.9%. Mean age at presentation was 64 years, 62% patients were female and 38% males. An incidental diagnosis was made in 43% of patients. Mucinous tumors of low malignant potential were significantly related to the presence of pseudomyxoma peritonei, identified in 16 (22%) of the cases. We also observed an increased risk of ovarian mucinous tumors in patients with a diagnosis of appendiceal mucinous neoplasm. In our sample, 22 (30.5%) patients showed a synchronous or metachronous colorectal cancer.
ConclusionsAppendiceal mucinous tumors are frequently an incidental finding. The diagnosis of mucinous tumors of low malignant potential is a factor associated with the development of pseudomyxoma peritonei. Histologic tumor grade and the presence of peritoneal dissemination will determine surgical treatment that can vary, from appendectomy to cytoreductive surgery.
El tumor mucinoso de apéndice tiene una incidencia inferior al 0,5% entre todos los tumores digestivos. Suele presentarse en la sexta década de la vida, con una clínica parecida a la de la apendicitis aguda. El objetivo de este estudio es describir los aspectos demográficos, clínicos, diagnósticos y terapéuticos de estos tumores. Además, se analiza la asociación entre tumores mucinosos con pseudomixoma peritoneal (PP) y la relación que presentan con los tumores de ovario y colorrectales.
MétodosSe realizó un estudio retrospectivo de todas las apendicectomías practicadas en nuestro centro desde diciembre de 2003 hasta diciembre de 2014.
ResultadosEntre 7.717 apendicectomías diagnosticamos un tumor mucinoso apendicular en 72 pacientes, lo que representa una incidencia de 0,9%. La edad media era de 64 años; eran mujeres el 62% y hombres, el 38%. El diagnóstico fue incidental en el 43% de los casos. El PP se presentó en 16 casos (22%), con una asociación estadísticamente significativa entre este tumor y el tumor de bajo potencial maligno. La cirugía programada se realizó en 42 casos y la urgente en 30. De los 72 tumores mucinosos del apéndice, 22 (30,5%) también presentaron cáncer de colon sincrónico o metacrónico.
ConclusionesLos tumores mucinosos de apéndice son con frecuencia hallazgos incidentales. El PP se asocia con un tumor mucinoso de bajo potencial maligno y el tratamiento puede comprender desde una apendicectomía hasta una cirugía citorreductiva, dependiendo del grado histológico del tumor y de la diseminación peritoneal.
Appendiceal tumors are a heterogeneous group of neoplasms, with an incidence of less than 0.5% of all gastrointestinal tumors.1 Mean age at presentation is in the sixth decade of life,2,3 and males are more frequently affected than females. The form of presentation is variable, but the most frequent symptom is abdominal pain in the right iliac fossa,4 often creating confusion with acute appendicitis at diagnosis. The definitive diagnosis is usually made during surgery or incidentally in the analysis of histological specimens, which represents less than 1% of all appendectomy specimens.5–7 Mucinous tumors represent about 8% of appendiceal neoplasms and can cause cystic dilation of the appendix due to accumulation of gelatinous material.
The classification of mucinous tumors of the appendix (MTA) is controversial when they lack aspects of malignancy but are associated with peritoneal mucin dissemination. Low-grade tumors confined to the appendix are clinically benign, whereas those that spread to the peritoneum may have a different clinical outcome. On the other hand, those tumors with invasion of the appendiceal wall or high degree of atypia may have an aggressive evolution and are considered adenocarcinomas.8 According to the classification by Pai and Longacre,9 mucinous appendiceal tumors are divided into mucinous cystadenoma (MC), mucinous tumors of uncertain malignant potential (M-UMP), mucinous tumors with low malignant potential (M-LMP) and mucinous adenocarcinoma (MA). Mucinous ascites known as pseudomyxoma peritonei (PMP) is present in more than 50% of these patients, and its presence indicates a more advanced stage and poorer prognosis. It may present as low-grade (diffuse peritoneal adenomucinosis) or high-grade (diffuse peritoneal carcinomatosis).10
Currently, the tendency is to differentiate these according to their histological grade (high or low), according to the classification of the American Joint Committee on Cancer.11 The term “mucocele” has become obsolete.
The main objective of this study is to describe the epidemiology, diagnosis and treatment of mucinous tumors. The secondary objectives are to analyze its association with ovarian and colorectal tumors, as well as invasion of the peritoneum in the form of PMP.
MethodsThis is a retrospective study of a consecutive series of patients with appendiceal mucinous tumors who had been treated surgically at our hospital from December 2003 to December 2014. Recommendations of the hospital Ethics Committee have been followed. The study was conducted based on existing pathology reports. Before 2005, the Misdrajii classification12 was used, and afterwards the Pai et al. classification was utilized.9 Reports prior to 2005 were reclassified to homogenize the criteria. Patients who presented PMP were referred to specialized centers, where the treatment was complemented with cytoreductive surgery and HIPEC.
Patient follow-up was done in the outpatient setting both one and six months post-op. At all office visits, colonoscopy was performed as part of the follow-up study for this type of tumor.
We recorded data for demographic characteristics (age, sex), forms of clinical presentation, diagnostic tests, intraoperative findings, surgical techniques performed and histological examination of the resected surgical speciemns. Diagnoses made by pathological analysis, after no preoperative or intraoperative suspicion, were considered incidental findings. Furthermore, we analyzed the association between the different types of mucinous tumors with the appearance of PMP, colorectal and ovarian tumors. To define PMP, we used the Ronnet et al. classification,10 which determines that pseudomyxoma can be presented as low-grade (or disseminated diffuse peritoneal adenomucinosis) and high-grade (or diffuse peritoneal carcinomatosis). Patient follow-up was completed in December 2015.
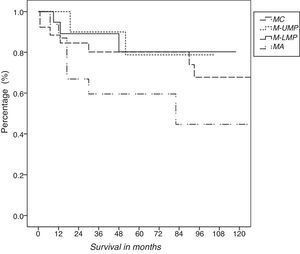
Statistical AnalysisCategorical variables were expressed by frequencies, while quantitative variables were expressed by median and range. For comparison of the categorical variables, the chi-squared test was used. Survival was calculated in months from surgery to the review date or death using Kaplan–Meier curves. Data analysis was performed using the SPSS version 20.0 statistical program. A P value ≤.05 was considered significant.
ResultsAmong the 7717 appendectomy specimens, 72 patients were diagnosed with MTA, representing a frequency of 0.9%; 62% were women, with a mean age of 64 (range: 27–92).
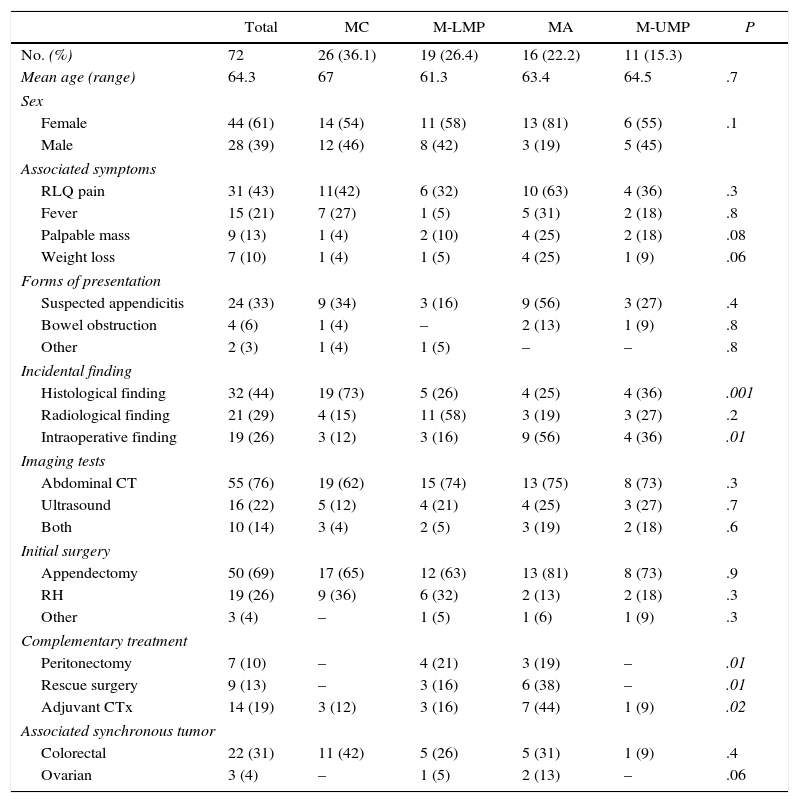
In terms of symptoms, 31 patients (43%) presented abdominal pain in the right iliac fossa. Other common signs and symptoms were fever, palpable mass and weight loss. The imaging tests used for diagnosis were ultrasound and computed tomography. After these imaging studies, in 21 patients (29%) an appendiceal tumor was suspected (Table 1).
Mucinous Tumor Characteristics According to the Pai et al. Classification.
| Total | MC | M-LMP | MA | M-UMP | P | |
|---|---|---|---|---|---|---|
| No. (%) | 72 | 26 (36.1) | 19 (26.4) | 16 (22.2) | 11 (15.3) | |
| Mean age (range) | 64.3 | 67 | 61.3 | 63.4 | 64.5 | .7 |
| Sex | ||||||
| Female | 44 (61) | 14 (54) | 11 (58) | 13 (81) | 6 (55) | .1 |
| Male | 28 (39) | 12 (46) | 8 (42) | 3 (19) | 5 (45) | |
| Associated symptoms | ||||||
| RLQ pain | 31 (43) | 11(42) | 6 (32) | 10 (63) | 4 (36) | .3 |
| Fever | 15 (21) | 7 (27) | 1 (5) | 5 (31) | 2 (18) | .8 |
| Palpable mass | 9 (13) | 1 (4) | 2 (10) | 4 (25) | 2 (18) | .08 |
| Weight loss | 7 (10) | 1 (4) | 1 (5) | 4 (25) | 1 (9) | .06 |
| Forms of presentation | ||||||
| Suspected appendicitis | 24 (33) | 9 (34) | 3 (16) | 9 (56) | 3 (27) | .4 |
| Bowel obstruction | 4 (6) | 1 (4) | – | 2 (13) | 1 (9) | .8 |
| Other | 2 (3) | 1 (4) | 1 (5) | – | – | .8 |
| Incidental finding | ||||||
| Histological finding | 32 (44) | 19 (73) | 5 (26) | 4 (25) | 4 (36) | .001 |
| Radiological finding | 21 (29) | 4 (15) | 11 (58) | 3 (19) | 3 (27) | .2 |
| Intraoperative finding | 19 (26) | 3 (12) | 3 (16) | 9 (56) | 4 (36) | .01 |
| Imaging tests | ||||||
| Abdominal CT | 55 (76) | 19 (62) | 15 (74) | 13 (75) | 8 (73) | .3 |
| Ultrasound | 16 (22) | 5 (12) | 4 (21) | 4 (25) | 3 (27) | .7 |
| Both | 10 (14) | 3 (4) | 2 (5) | 3 (19) | 2 (18) | .6 |
| Initial surgery | ||||||
| Appendectomy | 50 (69) | 17 (65) | 12 (63) | 13 (81) | 8 (73) | .9 |
| RH | 19 (26) | 9 (36) | 6 (32) | 2 (13) | 2 (18) | .3 |
| Other | 3 (4) | – | 1 (5) | 1 (6) | 1 (9) | .3 |
| Complementary treatment | ||||||
| Peritonectomy | 7 (10) | – | 4 (21) | 3 (19) | – | .01 |
| Rescue surgery | 9 (13) | – | 3 (16) | 6 (38) | – | .01 |
| Adjuvant CTx | 14 (19) | 3 (12) | 3 (16) | 7 (44) | 1 (9) | .02 |
| Associated synchronous tumor | ||||||
| Colorectal | 22 (31) | 11 (42) | 5 (26) | 5 (31) | 1 (9) | .4 |
| Ovarian | 3 (4) | – | 1 (5) | 2 (13) | – | .06 |
MA: mucinous adenocarcinoma; MC: mucinous cystadenoma; M-LMP: mucinous tumor of low malignant potential; M-UMP: mucinous tumor of uncertain malignant potential.
Statistically significant P values are in italics.
Source: Based on the Pai et al.9 classification
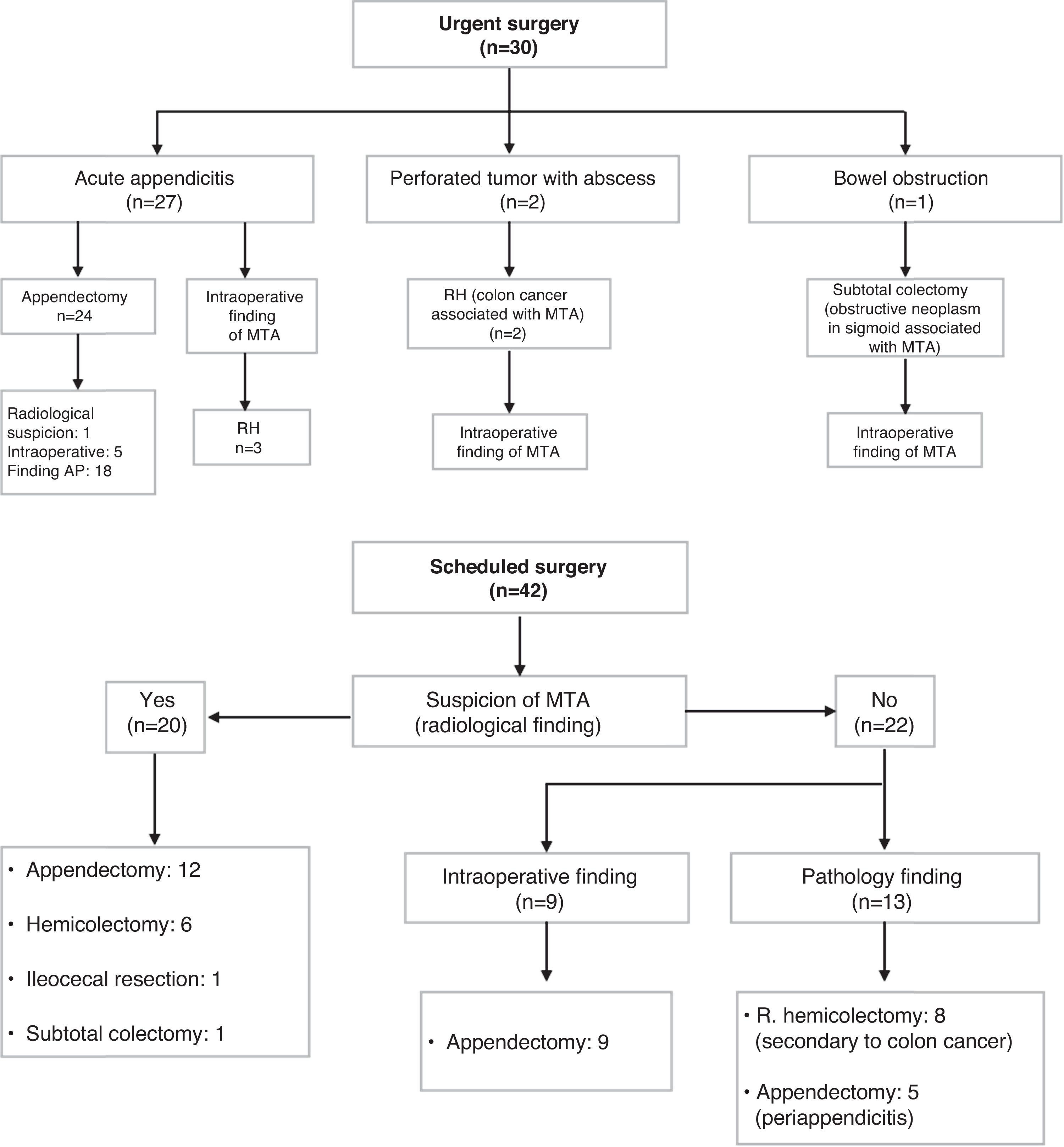
Thirty surgeries (42%) were performed urgently (24 appendectomies, 5 right hemicolectomies and a subtotal colectomy for obstructive sigmoid tumor with cecal perforation and intraoperative finding of MTA). Out of the 5 right hemicolectomies that were performed on an urgent basis, 3 were due to suspected malignant tumor of the appendix with presence of mucoid material and peritoneal implants. The 2 remaining surgeries were due to bowel obstruction with a change in diameter at the transverse colon secondary to synchronous neoplasm and intraoperative suspicion of associated MTA.
A total of 42 scheduled surgeries (58%) were performed, 26 of which were appendectomies, 14 right hemicolectomies, one ileocecal resection, and a subtotal colectomy for an appendiceal tumor infiltrating the sigmoid colon and bladder. Out of the 14 right hemicolectomies, 6 were performed for radiological suspicion of appendicular tumor. One was performed after the intraoperative histological analysis of the appendix, in which invasion of the surgical margins was observed. The remaining surgeries were indicated for disease in another region; the diagnosis of MTA was incidental after the intraoperative histological study (Fig. 1).
The most common type of mucinous tumor in our series was MC (26 cases, 36.1%), followed by M-LMP (19 cases, 26.4%), adenocarcinoma (16 cases, 22.2%) and M-UMP (11 cases, 15.3%). In total, 31 cases (43%) were diagnosed as incidental findings after analysis of the histological specimen. In addition, an appendiceal tumor was observed intraoperatively in 20 patients (28%).
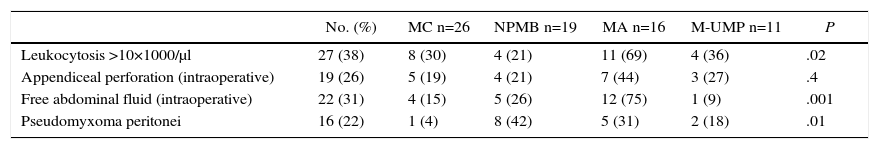
Out of the 72 mucinous tumors at the time of diagnosis, 16 (22.2%) presented PMP. Out of the 19 patients with M-LMP, 8 presented PMP: 3 in the form of diffuse peritoneal adenomucinosis and 5 as diffuse peritoneal carcinomatosis (Table 2). In addition, a statistically significant association was observed between the appearance of PMP and M-LMP (P<.05).
Clinical Correlation With the Histological Type of Mucinous Tumor.
| No. (%) | MC n=26 | NPMB n=19 | MA n=16 | M-UMP n=11 | P | |
|---|---|---|---|---|---|---|
| Leukocytosis >10×1000/μl | 27 (38) | 8 (30) | 4 (21) | 11 (69) | 4 (36) | .02 |
| Appendiceal perforation (intraoperative) | 19 (26) | 5 (19) | 4 (21) | 7 (44) | 3 (27) | .4 |
| Free abdominal fluid (intraoperative) | 22 (31) | 4 (15) | 5 (26) | 12 (75) | 1 (9) | .001 |
| Pseudomyxoma peritonei | 16 (22) | 1 (4) | 8 (42) | 5 (31) | 2 (18) | .01 |
MA: mucinous adenocarcinoma; MC: mucinous cystadenoma; M-LMP: mucinous tumor of low malignant potential; M-UMP: mucinous tumor of uncertain malignant potential
Statistically significant P values are in italics.
Furthermore, after examination of the appendectomy specimens, 8 patients required a second surgery, and right hemicolectomies were performed due to invasion of the surgical margins. In one patient, an ileocecal resection was carried out.
MTA was associated with an ovarian mucinous tumor in 3 cases. Out of these, 2 had MA of the appendix. An associated synchronous or metachronous colorectal tumor was also observed in 22 cases (30.5%).
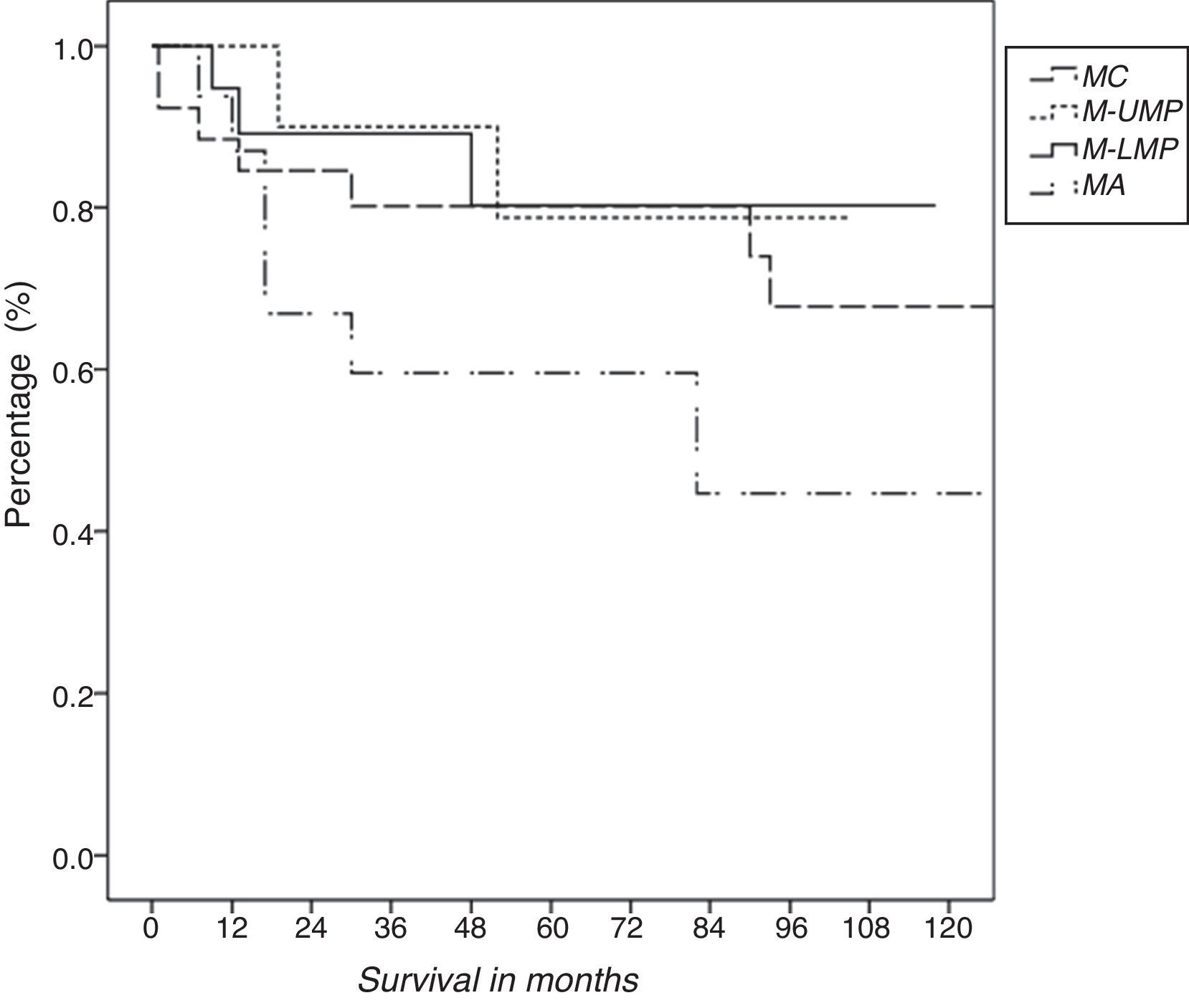
Overall survival of patients with MTA was 73%. Actuarial survival after 1, 3 and 5 years was 91, 78 and 74%, respectively (Fig. 2). There were 18 deaths, 7 of which were caused by the tumor.
DiscussionThe term “mucocele” was first used by Rokitansky12 in 1842 to refer to the cystic dilatation of the appendiceal lumen with the accumulation of mucus in its interior. This encompasses a wide variety of tumors, from simple retention cysts to invasive adenocarcinomas. Currently, it is recommended to use the term “mucinous tumors” to refer to this pathology.
The presentation is non-specific, varying from totally asymptomatic forms to abdominal pain in the right iliac fossa similar to acute appendicitis, palpable mass, gastrointestinal bleeding or urological symptoms.4,8
Preoperative diagnosis is difficult due to the lack of specific symptoms. The definitive diagnosis is usually an incidental finding during a surgical intervention, radiological study or in the pathology study of an appendectomy specimen.3,4
Computed tomography is considered the imaging technique of choice, which is diagnostic in less than 50% of cases. However, this test is useful for detecting the presence of localized PMP and recurrences after surgical treatment.13 The presence of irregularities in the appendiceal wall and increased thickness of the soft tissue can predict tumor malignancy.14,15 Another test used is magnetic resonance imaging, which is useful for detecting tumor rupture, extra-appendiceal mucin and to differentiate mucinous tumors from other intra- and retroperitoneal pathologies.
Misdraji et al.16 classified mucinous tumors as low-grade (absence of architectural destruction, confined to the appendix or with dissemination to the peritoneum) or adenocarcinomas (invasive destruction). Afterwards, Pai and Longacre9 added 2 new categories of mucinous tumors: M-UMP and M-LMP. M-LMP disseminate to the peritoneum, but they are not clearly invasive and are responsible for most cases of PMP. Macroscopically, they are indistinguishable from MC, but microscopically the difference is that the neoplastic cells of the tumors with low malignant potential invade the appendix wall and disseminate beyond the appendix in the form of peritoneal implants and ovarian involvement. Although there is still no unanimity in the classification and nomenclature, the World Health Organization proposes classifying these tumors as adenoma, low-grade mucinous tumor and adenocarcinoma.17 However, there is still much controversy about which classification should be used to define MTA.
The treatment of choice is surgical and can vary from appendectomy to right hemicolectomy.18 If the finding is incidental during surgery, conversion from laparoscopy to laparotomy is recommended due to the dissemination of mucin and the need to explore areas like the colon or ovaries. However, García-Lozano et al.19 have reported that it is possible to finalize surgery laparoscopically with careful tumor manipulation.
On the other hand, if the appendix is perforated but there are no affected margins or lymphatic invasion, the treatment of choice is appendectomy plus HIPEC. If, in contrast, positivity is demonstrated for surgical margins but there is no lymph node involvement, ileocecal resection and HIPEC should be carried out. If the HIPEC cannot be done, close patient follow-up would be necessary.20
Right hemicolectomy is reserved for MA since there is a high risk for lymph node metastasis.21,22 Turraga et al.23 consider right hemicolectomy a surgical technique where the lymphadenectomy aids in the staging of patients with a high probability for lymph node metastases. Sugarbaker24 also recommends right hemicolectomy in patients with local lymph node or ileocolic involvement observed in the biopsy or if there are inadequate resection margins. Certainly, right hemicolectomies should not be routinely done in patients diagnosed with MTA, and each case should be individualized. Recently, a new concept has been introduced, which is radical appendectomy, as an alternative to right hemicolectomy, a technique that requires increased use in order to assess the results in future studies.25
With regard to PMP treatment, Sugarbaker proposes aggressive surgical treatment that has a great impact on survival and disease-free survival.24 Surgery consists of the resection of the parietal and visceral peritoneal surfaces associated with the excision of organs, such as the stomach, gallbladder, right colon and rectum/sigmoid colon plus adjuvant therapy with HIPEC. This type of chemotherapy is useful after the instillation of the cavity with mucolytic agents that act as “cytoreducers” when releasing the mucus deposits, allowing them to drain and thereby obtaining better perfusion of chemotherapy. At our hospital, we do not have HIPEC available, which is why we refer patients who require this type of treatment to specialized medical centers. In our study, we observed that, out of the 19 patients with M-LMP, 8 presented PMP (P<.05). This association was not significant in the case of MA or M-UMP.
An association has also been reported between any type of appendiceal tumor and the appearance of a synchronous colorectal tumor; therefore, frequent follow-up of these patients is recommended.26 This finding has been confirmed in our series, in which 22 (30.5%) patients with MTA presented colon neoplasia. Conversely, in another series, the presence of an appendiceal tumor has also been observed in 7 out of 169 appendectomy specimens resected at the same time as a colon tumor.23 In one of the most extensive series in our country including 35 patients with MTA, this relationship was also identified, and follow-up colonoscopy was therefore recommended.27 At our hospital, patient follow-up after the finding of an appendiceal tumor, either benign or malignant, involves periodic colonoscopies.
Furthermore, a significant association has also been reported between appendiceal mucinous adenocarcinomas and mucinous ovarian tumors. It has been observed that both tumors have a similar histology,28 which indicates a primary appendiceal origin that affects the ovaries.29
In conclusion, MTA can present as acute appendicitis, although they are also frequent incidental findings when examining histology specimens. Treatment will depend on the histological grade of the tumor and the presence of PMP. Patients with tumors of the appendix should be closely followed up with periodic colonoscopies given the risk of an associated colorectal tumor.
Authorship/collaborationsOana Anisa Nutu: study design, article composition.
Alberto Marcacuzco: data collection, critical review and approval of the final version.
Alejandro Manrique: critical review and approval of the final version; study design.
Jorge Calvo Pulido: analysis and interpretation of the results; critical review and approval of the final version.
Iago Justo: data collection; analysis and interpretation of the results.
María García Conde: data collection; analysis and interpretation of the results.
Félix Cambra: data collection; study design.
Carlos Jiménez-Romero: study design; article composition.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Nutu OA, Marcacuzco Quinto AA, Manrique Municio A, Justo Alonso I, Calvo Pulido J, García-Conde M, et al. Tumores mucinosos del apéndice: incidencia, diagnóstico y tratamiento quirúrgico. Cir Esp. 2017;95:321–327.