The development of fecal incontinence after childbirth is a common event. This incontinence responds to a multifactorial etiology in which the most common element is external anal sphincter injury. There are several risk factors, and it is very important to know and avoid them. Sphincter injury may result from perineal tear or sometimes by incorrectly performing an episiotomy. It is very important to recognize the injury when it occurs and repair it properly. Pudendal nerve trauma may contribute to the effect of direct sphincter injury. Persistence of incontinence is common, even after sphincter repair. Surgical sphincteroplasty is the standard treatment of obstetric sphincter injuries; however, sacral or tibial electric stimulation therapies are being applied in patients with sphincter injuries not repaired with promising results.
El desarrollo de incontinencia fecal tras el parto es un hecho frecuente. Esta incontinencia responde a una etiología multifactorial en la que el elemento más frecuente es la lesión del esfínter anal. Existen diversos factores de riesgo, que es muy importante conocer y evitar. La lesión esfinteriana puede producirse por desgarro perineal o en ocasiones por la realización de una episiotomía de forma incorrecta. Es muy importante reconocer la lesión cuando se produce y repararla de forma adecuada. El traumatismo de los nervios pudendos puede incrementar el efecto de las lesiones esfinterianas directas. Es frecuente la persistencia de incontinencia a pesar de la reparación esfinteriana primaria. La esfinteroplastia quirúrgica es el tratamiento estándar de las lesiones esfinterianas obstétricas, sin embargo, las terapias de estimulación eléctrica sacra o tibial están siendo aplicadas en pacientes con lesiones esfinterianas no reparadas, con resultados prometedores.
Fecal incontinence is very frequent after childbirth. Prevalence studies in different populations and postpartum series of women at certain hospitals have reported global incontinence rates ranging from 4% to 59%.1–11 In our setting, a series of Spanish cohorts with more than 1000 nulliparous women found an incidence of immediate postpartum fecal incontinence of 7.3%.12
The variability in the incidences published is quite striking. This is perhaps because women often do not mention incontinence to their physician, obstetricians do not consider this problem in all cases, the degree of soiling may vary greatly and also vary over time, and measuring subjective symptoms is difficult.
The etiology of postpartum fecal incontinence is multifactorial, and its treatment requires multidisciplinary action. Therefore, its management is occasionally complex and accompanied by disheartening treatment results.
The objective of this article is to provide an update on different key aspects in obstetrical fecal incontinence by reviewing the literature. We also provide the experience of our own group in order to determine what type of management is best for this condition.
MethodologyWe have reviewed the existing literature in the PUBMED and COCHRANE databases. Search criteria included the following key words: postpartum fecal incontinence, obstetrical fecal incontinence, obstetrical injury and anal sphincter, perineal tears and anal sphincter, postpartum anal sphincter injuries. Included in the study were all those publications from 1990 to date.
Causes of Fecal Incontinence After ChildbirthDuring childbirth, there are several situations that can condition the development of injuries to the posterior compartment and potentially cause subsequent fecal incontinence.
First of all, perineal tears are frequent during delivery. These tears can occasionally affect the anal sphincter muscles, most frequently the external anal sphincter, which controls voluntary fecal continence. The rate of anal sphincter lesions is variable but ranges between 2% and 30% in different series.3,13–17
Episiotomies, which are sometimes done to favor the delivery of the fetus, can be strongly related with direct sphincter injuries by the episiotomy itself when done incorrectly and sphincter muscle fibers are cut.2,3,14,18
Another frequent lesion during childbirth is damage to the pudendal nerves.6,19–22 These injuries do not seem to be secondary to direct trauma during delivery, but instead to traction/stretching by the distension of the perineum during a lengthy labor.
Finally, the trauma to and injury of other perineal muscles, mainly the puborectalis and other components of the levator ani, can increase the injuries to the posterior compartment and sphincter apparatus, resulting in serious consequences.
The situation of the posterior perineal compartment with regard to the birth canal is the determining factor that frequently leads to injury of the compartment. Its shape forms a J, where the bottom of the J is the rectum. The axial forces developed during labor pivot on the posterior compartment, causing trauma.23
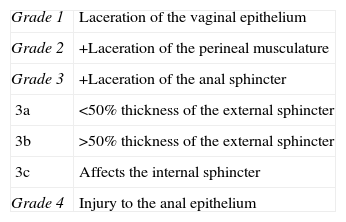
Classification of Perineal TearsThe classification of perineal tears caused during delivery is based on the injured anatomical layers in the mid and posterior compartments (skin, mucosa and musculature)24 (Table 1).
Classification of Obstetrical Tears.
| Grade 1 | Laceration of the vaginal epithelium |
| Grade 2 | +Laceration of the perineal musculature |
| Grade 3 | +Laceration of the anal sphincter |
| 3a | <50% thickness of the external sphincter |
| 3b | >50% thickness of the external sphincter |
| 3c | Affects the internal sphincter |
| Grade 4 | Injury to the anal epithelium |
Source: Sultan et al.24
It is based on the elements involved or damaged by the tear. The laceration generally initiates in the vaginal mucosa and can progress, depending on the intensity, and injure (from front to back) the perineal musculature, the external anal sphincter, internal anal sphincter, and, finally, the anal mucosa. This latter case would result in complete anovaginal contact; if it is not repaired, or done so incorrectly, a rectovaginal fistula could develop. When in doubt about which anatomical planes are affected during a tear, it should be classified as the higher grade.
Grade 3 and 4 injuries are those that affect the anal sphincter apparatus and can cause fecal incontinence.
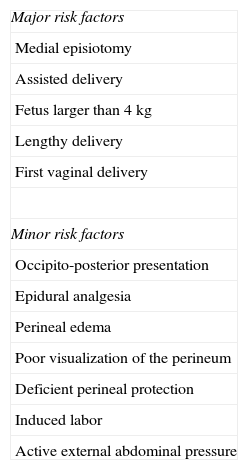
Risk Factors Related With Sphincter Lesions During DeliveryThere are a multitude of studies in the literature that try to apply scientific evidence to determine the factors of childbirth that favor the appearance of postpartum fecal incontinence or the production of sphincter lesions2,3,9,10,15,18,25,26 (Table 2).
Risk Factors for the Development of Fecal Incontinence After Childbirth.
| Major risk factors |
| Medial episiotomy |
| Assisted delivery |
| Fetus larger than 4kg |
| Lengthy delivery |
| First vaginal delivery |
| Minor risk factors |
| Occipito-posterior presentation |
| Epidural analgesia |
| Perineal edema |
| Poor visualization of the perineum |
| Deficient perineal protection |
| Induced labor |
| Active external abdominal pressure |
Episiotomy has been related with fecal incontinence due to direct sphincter injury.2,3,15,18 Some studies have demonstrated that systematic episiotomies have no advantages over their selective use in vaginal births, even in the case of operative vaginal deliveries.27–29 In the article by Signorello et al.18 the incidence of fecal incontinence was greater in the group of women who underwent medial episiotomy than in the group with spontaneous perineal tears. Medial–lateral episiotomy has the advantage over medial episiotomy of lower sphincter injury rates.2,30 This is due to the anatomical situation of the anal sphincter in a perineum that is distended during labor, in which the rectovaginal wall is thinning out and the anterior edge of the external anal sphincter is in close contact with the posterior vaginal edge. A medial skin incision may easily include muscle fibers of the external anal sphincter at a location (anterior) where the length of the sphincter is shorter and, therefore, the damage may have greater repercussions.
Instrumented vaginal deliveries are a risk factor for fecal incontinence.2,3,9,10,13–15,25,31 The use of forceps or vacuum is related to sphincter injuries during vaginal manipulation.17 The rate of injuries and aftereffects can be relatively high when sphincter functionality is reviewed in detail after operative deliveries; this rate may be higher with forceps than with vacuum extraction. In a randomized study of 130 women in whom anorectal function was studied after delivery by means of an incontinence questionnaire, endoanal ultrasound and anal manometry, a fecal incontinence rate of 59% was found in the forceps delivery group, while the rate in the vacuum group was 33%, with statistically significant differences. The sphincter injury rates were 56% in the forceps group and 49% in the vacuum group, with no statistical significance.31
In theory, elective Cesarean sections would avoid the perineal trauma of a vaginal birth and would reduce the probability of secondary incontinence. Studies have confirmed this correlation,25,32 and it has become a possible indication for a scheduled C-section at the request of the patient. Although there is no clear data from randomized series, 2 systematic reviews have not demonstrated the supposed protective effect of elective C-section.8,33 These data seem to indicate the existence of other etiopathogenic factors for the development of postpartum fecal incontinence that are not associated with pelvic floor trauma during vaginal delivery. It has also been proposed that pregnancy itself may be a risk factor for fecal incontinence, regardless of the type of delivery.12,34 In a recent cross-sectional study of 1571 first-time mothers, 37% developed fecal incontinence at the end of pregnancy, affecting their quality of life.35
Other Causes for Postpartum Fecal IncontinenceThe appearance of postpartum fecal incontinence is a multifactorial process.3 Sphincter defects are associated with 50%–80% of cases of incontinence after childbirth.16,36 Although anal sphincter injury due to perineal tears is the most frequent cause, there are other causes that can cause incontinence themselves or in association with sphincter damage, resulting in worse consequences. The main cause is damage to the pudendal nerves.
Postpartum alternations to the pudendal nerves are more frequent and important than they seem.6,19,20,22 In one study19 that involved electrophysiological testing of the pudendal nerves after delivery, 46% of the group of women with incontinence but no documented sphincter injury had pudendal alterations. In this group, 44% of the sphincter injuries had not been recognized. In the group of women with recognized sphincter injury, 19% had electrophysiological alterations of the associated pudendal nerves. Nonetheless, 33% of the women who had undergone C-section also had damage to the pudendal nerves, which was associated with fecal incontinence in all cases. In this latter group, sphincter injuries were not demonstrated. These data seem to indicate that not even a Cesarean section can totally avoid the risk for incontinence. Perhaps lengthy labor can cause distension of the perineum and stretching of the pudendal nerves, even though a C-section is ultimately performed.
In recent years, the advances made in imaging techniques, such as magnetic resonance and 3-D vaginal/perineal ultrasound, have shown evidence of another type of obstetrical injuries that could be either the cause or coadjuvants in the development of fecal incontinence. These are deep injuries of the levator ani muscle and its different components.37 These injuries could be secondary to the perineal trauma during childbirth in any case.
Primary Tear RepairIt is important to recognize tears caused during delivery and determine the anatomical layers involved and, therefore, their grade. These tears must be repaired correctly in order to avoid later consequences.
When the injury affects the anal sphincter, reconstruction should be done more meticulously to avoid more serious sequelae.23 The repair can be done with regional anesthesia (epidural/spinal block), in the operating room, with adequate material and aseptic measures. It is important to suture plane by plane, started with the deepest plane and working up to the most superficial. There is no scientific evidence about what type of suture material to use or about whether continuous sutures or individual stitches are preferable.38 However, the sutures should stay within each plane, without tension and with good vascularization.
Some authors argue on the need to release the sphincter ends in order to repair them by overlapping and not with a mere apposition. There are several randomized studies comparing end-to-end repairs with overlapping, and they have found no differences in the fecal incontinence rates between the 2 techniques.39–43 However, in a randomized series44 and a later meta-analysis,45 the Fernando et al. group demonstrated that overlapping repairs may be associated with a lower incidence of fecal urgency, lower scores on postpartum incontinence scales and a lower risk for deterioration of incontinence symptoms 12 months later.
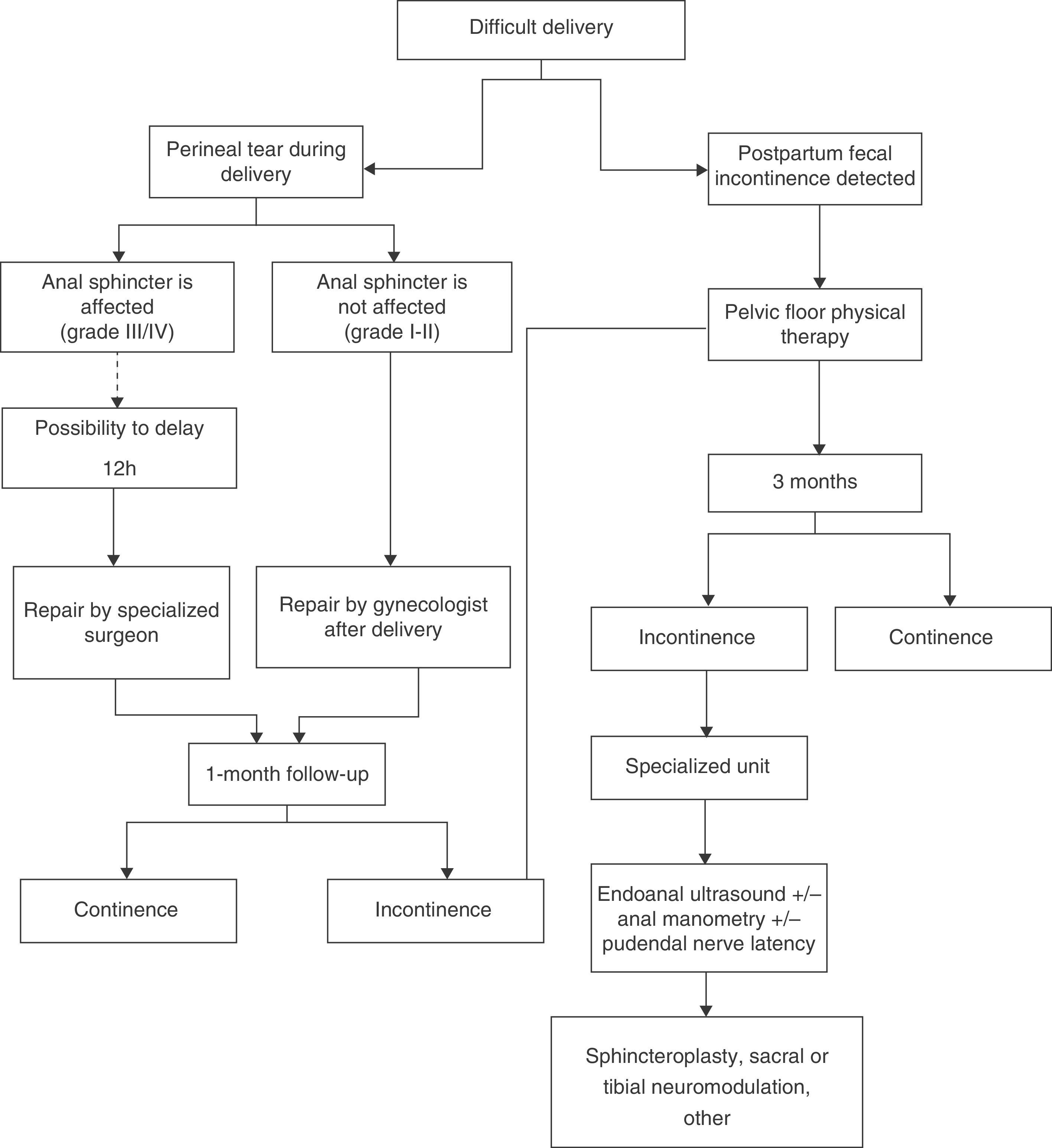
The complexity of the tear and, therefore, the repair required determine which professional should perform the repair: a gynecologist, general surgeon or proctologist.23 Surgical treatment of the sphincter is better left in the hands of surgeons with previous experience in anal reconstructive surgery, and perhaps they should be responsible for repairing Grade 3 and 4 injuries. There are data that indicate that, when the immediate repair of the obstetrical tear is done by a team trained in this type of techniques, 4-year postpartum incontinence rates do not differ from pre-birth rates.46 However, the organization of each hospital and the timing of the injury determine whether the repair can or cannot be done by an experienced team. In this regard, a randomized study demonstrated that deferring the repair for an average of 8–12h after the tear occurs does not lead to poorer functional results, infection or complication rates of the deferred sutures.47 This margin of time could be sufficient to organize deferred surgery by a surgeon with expertise in sphincter reconstructive techniques (Fig. 1).
Perioperative management is also important23 and should be individualized in each case. The use of wide-spectrum antibiotics is debatable. There is no scientific evidence that recommends their routine use,38 but they may be necessary in Grade 3–4 severe tears or when there has been much fecal contamination. The use of astringent medication after the repair is used to protect against possible direct mechanical trauma during the first bowel movement or fecal contamination. However, a randomized study seems to demonstrate that there are no functional, ultrasound or manometric differences after Grade 3 perineal tear repairs when astringent medication is administered compared with laxatives during the immediate postpartum. Conversely, the patient group that was prescribed laxatives had less pain during the first bowel movement, which was also earlier, while hospitalization was significantly shorter.48
Evolution of Postpartum IncontinenceThe rate of persistent sphincter injuries after primary repair is 70%–75%.19,49 In addition, the appearance of fecal incontinence after the repair is 50%–60%.8,19,49 Meanwhile, there are unrecognized sphincter injuries in 18%–45%8,19,20 and asymptomatic sphincter injuries in 30%.16
These data show that many women will have fecal continence problems after childbirth, either because a sphincter injury was not identified or because, even if the injury were recognized, there is a high frequency of repair failure.
Primary repairs can fail due to several causes: misidentification of the sphincter ends, retraction associated with recuperated muscle tone after pregnancy, incomplete suture along the length of the sphincter, and postoperative factors like hematoma or infection.50
In the mid-term, complete involution of obstetrical incontinence is possible in the first 3 months postpartum.23 Possible causes involved in this regression include the resolution of the trauma to the pudendal nerves or improved perineal muscle tone. Some studies, however, have demonstrated that the persistence of incontinence after 9 months is a strong predictive factor of the persistence of the symptoms.23,51
In the long term, the sequelae of incontinence may persist for years. There are data about the persistence of fecal incontinence symptoms of up to 40% in women after sphincter injuries or incontinence immediately after delivery in surveys done 12 years52 and even 27 years53 later. The risk for fecal incontinence in primiparous women increases over time, especially with more vaginal births.36,51 With successive pregnancies, the injuries from previous deliveries can become aggravated. A second vaginal birth can often trigger fecal incontinence in a woman with a subclinical sphincter lesion caused during the first delivery. There are authors who recommend offering to schedule a C-section in women at high risk or with previous sphincter injuries, after assessing the risks and benefits.54
Pre- and postpartum physical therapy of the pelvic floor can be useful to improve incontinence symptoms.55 Nonetheless, this functional improvement does not seem to maintain itself over time. In a controlled study in which women with postpartum urinary and fecal incontinence had pelvic floor physical therapy, improved symptoms were observed 1 year later in the treatment group,56 but this did not persist in the long term (6 years57 and 12 years58). The initial physiological compensation can likely improve with proper rehabilitation, but, in the long term, reactive processes and exposure to further obstetrical trauma lead to deteriorated function.
Occasionally, mild sphincter lesions become evident after menopause, coinciding with the physical involution of the pelvic floor, leading to the development of clinical fecal incontinence.8,59
Diagnosis of Residual InjuriesThe diagnosis of injuries caused during childbirth should begin at the postpartum obstetrical office visit.23 It is important to have recorded and described any type of tear, which should be assessed afterwards. At this first consultation, the patient should be asked about possible symptoms of fecal incontinence, urgency or soiling. If any symptoms are detected, pelvic floor physical therapy is recommended.55
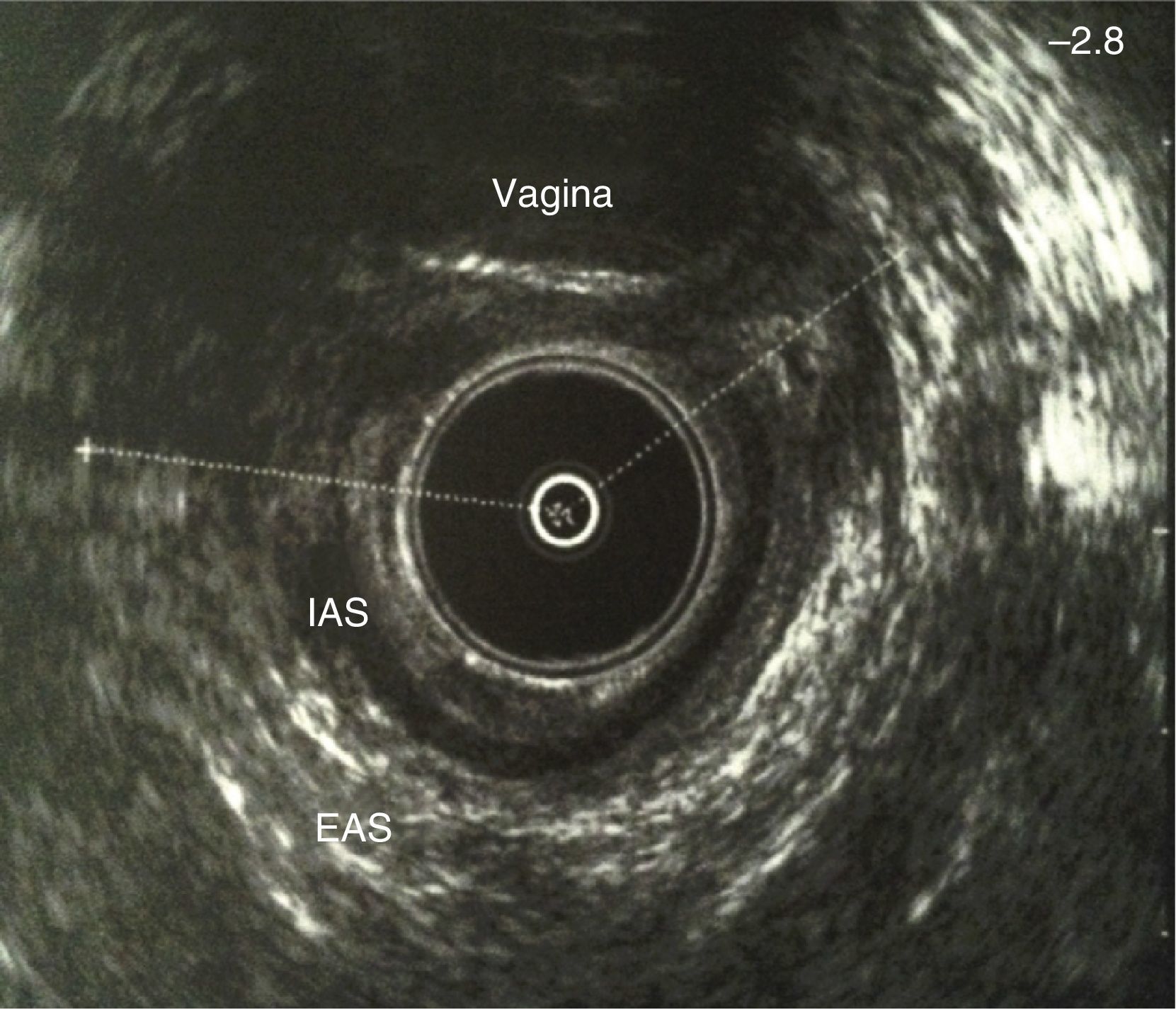
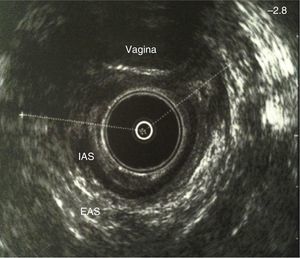
In cases of persistent incontinence for more than 3 months, when the time for a possible spontaneous involution has passed,23 the patient should be referred to a specialized unit for study and treatment (Fig. 1). The diagnosis of the sphincter injury is usually done with endoanal ultrasound (Fig. 2), which determines the grade of the injury and its extension, while providing essential information for a proper repair.60 Generally, the injuries affect the external sphincter and are occasionally associated with discontinuity of the internal sphincter. Ultrasound shows a solution of continuity of the hyperechoic layer, which corresponds with the external sphincter, or the hypoechoic layer, which corresponds with the internal sphincter, in the anterior region.59 It is important to measure the angle of the retracted muscle ends in order to assess the reliability of a potential surgical repair. Occasionally, fibrous areas can be observed between the muscle endings, depending on the time transpired since the injury.
The Stark scoring system,61 which assesses sphincter defects three-dimensionally (size, length and depth) using anal ultrasound, has been correlated with the long-term degree of fecal incontinence.62 It can also have prognostic utility and help determine which patients would benefit from an early secondary repair without waiting for a response to conservative measures.
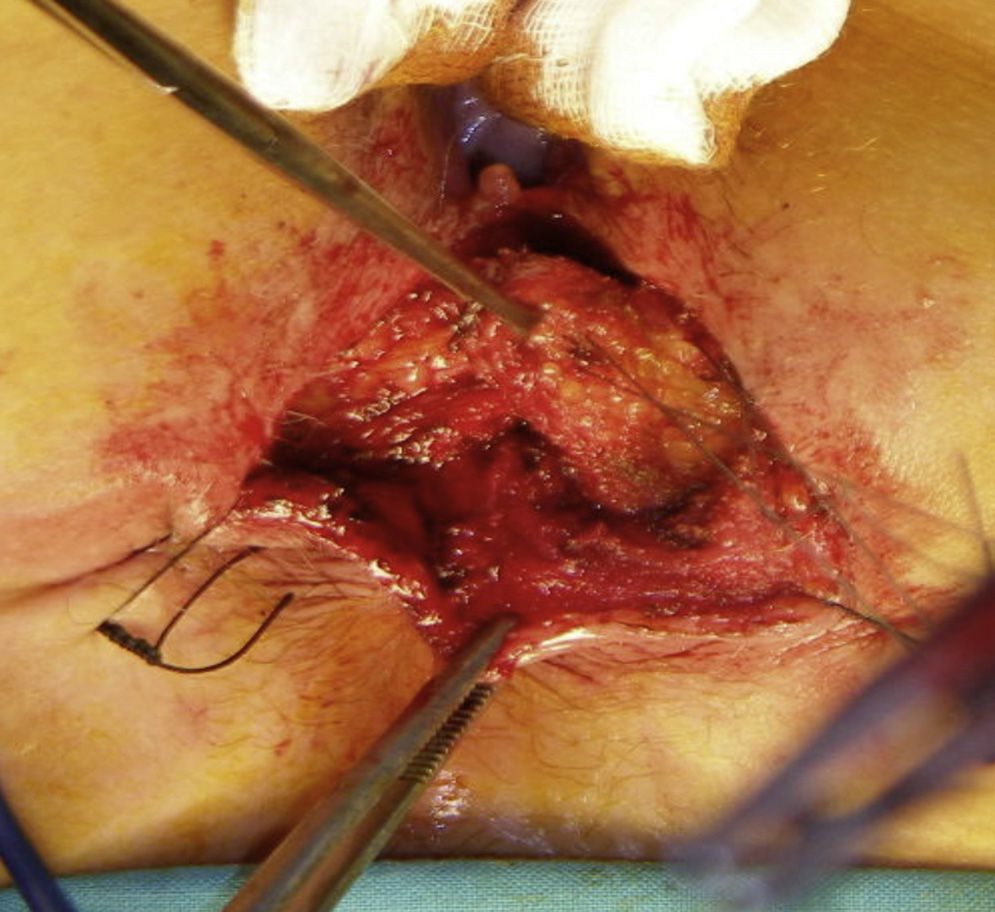
Secondary RepairSecondary repairs of obstetrical sphincter injuries are possible when diagnosed with endoanal ultrasound and when they are less than 120–180°. Sphincteroplasty consists of dissecting the sphincter ends, which are carefully released and overlapped without tension. It is recommended to not remove the fibrous scar tissue of the endings in order to create the suture, nor should the mucosa of the anal canal be cut60 (Fig. 3).
The results of sphincteroplasty are initially satisfactory in two-thirds of patients.63 These results, however, have been obtained in non-experimental studies with a limited number of cases. Furthermore, there are data that have demonstrated that the initial beneficial effects of sphincteroplasty may not endure over time.64–67 In the study by Halveson et al.64 with a mean follow-up of 69 months after sphincteroplasty, only 14% of the patients were totally continent. Another study65 evaluated a group of patients 3 and 40 months after sphincteroplasty and showed evidence of a reduction in the total rate of continence from 49% to 28% in this period, with an increased rate of fecal incontinence from 19% to 49%. In the study by Malouf66 after a mean follow-up of 77 months, out of a total of 38 patients who had not undergone stoma or any other surgery for incontinence, 100% presented some type of incontinence. Another study67 observed a significant variation of the Wexner scale score from 17.8 pre-op to 3.6 3 months after sphincteroplasty, and a worsened condition after 80 months with a mean score of 6.3. Separate dissection and repair of the external and internal sphincters have not been shown to improve the functional results.68 The association of pudendal neuropathy can worsen the sphincteroplasty results,69,70 although this result has not been corroborated in other studies.71,72
Other TreatmentsIn general, it seems that the repair of sphincter anatomy injuries is necessary but should be reinforced with other treatments that could improve functional results, especially in the mid to long term. Proper rehabilitation of the pelvic floor both pre- and post-op could be important, especially when the sphincter injury is old and the anatomical defect is associated with atrophy due to prolonged hypofunctionality. Biofeedback and sacral or tibial nerve stimulation treatments can also play an important role in improving the results. Furthermore, the indications for sacral neuromodulation have been extended to include patients with unrepaired sphincter defects, which has provided good results,73–79 although there have been no randomized studies comparing this technique with sphincteroplasty. Likewise, some groups have applied tibial stimulation in cases of fecal incontinence with sphincter defect, resulting in improved symptoms.80,81
ConclusionsThe fecal incontinence rate after childbirth is high. It is important to detect and avoid, if possible, any possible factors and actions that involve risk (episiotomy, forceps, etc.). The etiopathogenesis of this incontinence is multifactorial; the most important related factors are perineal tears that affect anal sphincters, trauma to the pudendal nerves and injury to other components of the levator ani.
When sphincter injuries occur, it is essential to detect and treat them properly. Likewise, it is important to evaluate the appearance of fecal incontinence at the post-partum consultation. In cases with persistent sequelae, it is necessary to refer the patient to teams with experience in the treatment of fecal incontinence.
Anal sphincteroplasty is the standard treatment of obstetrical sphincter injuries. However, it may be necessary to include adequate pre-and post-operative physiotherapy or associate other treatments in some cases in order to improve mid- and long-term results. Electrical stimulation therapies seem to improve the functionality of patients with unrepaired sphincter lesions, although clinical trials are needed to compare this therapy with surgical sphincter repair.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Rodríguez R, Alós R, Carceller MS, Solana A, Frangi A, Ruiz MD, et al. Incontinencia fecal posparto. Revisión de conjunto. Cir Esp. 2015;93:359–367.