Neuroendocrine tumors (NET) of the breast are uncommon, representing less than 2% of malignant mammary gland tumors.1 They can be primary or metastatic, and there are no clinical or radiological data that differentiate between them. Therefore, their diagnosis is provided by immunohistochemistry, their origin and the presence or absence of markers such as mammaglobin or GCDFP-15.2 The differential diagnosis is important in order to establish the therapeutic strategy.
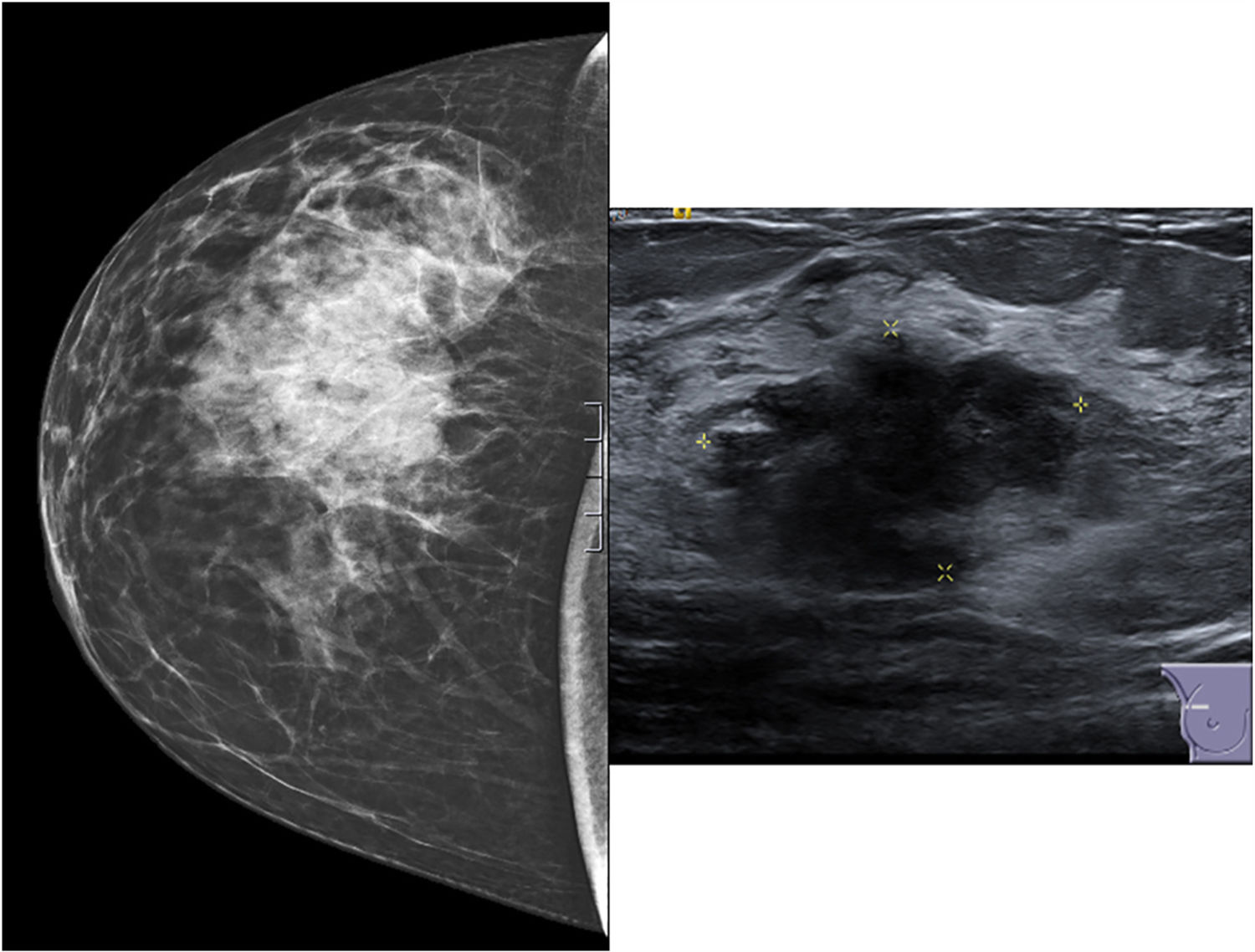
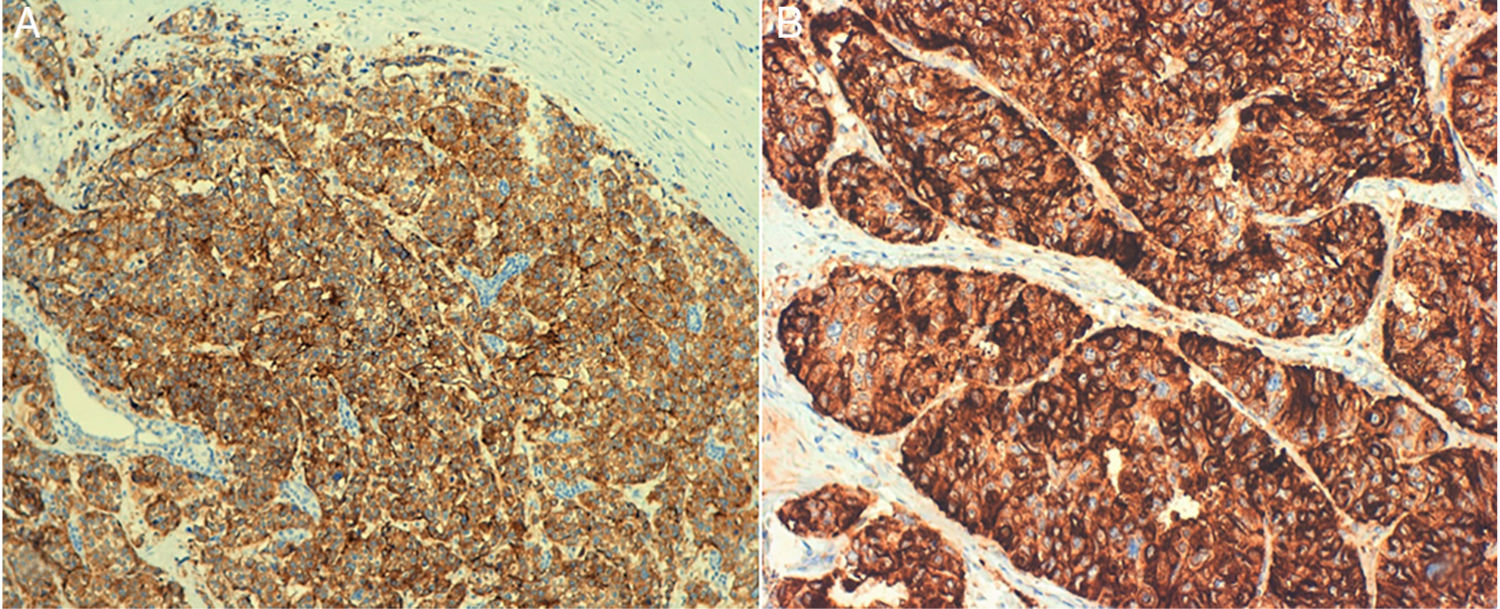
A 64-year-old woman, with no history of interest, consulted for a nodule in the right breast that had been progressing for several months, with no other symptoms. The mammography study showed a tumor with satellite nodules, measuring 44 mm × 22 mm in the upper outer quadrant of the right breast. The ultrasound study detected a mass with irregular morphology and margins that was hypoechoic and associated with multiple satellite nodules, with no suspicious axillary lymph nodes (Fig. 1). Ultrasound-guided core-needle biopsy confirmed neuroendocrine carcinoma with positive hormone receptors and negative HercepTest. Immunohistochemistry showed the mass was positive, in its entirety, for neuroendocrine markers (synaptophysin and chromogranin) (Fig. 2). Negativity for TTF1, CK7, CK20 and CDx2 ruled out a pulmonary or digestive origin, and positivity for hormone receptors led to the suspicion of a primary breast origin. After a normal PET/CT, surgical treatment was indicated with mastectomy due to the tumor size together with selective sentinel lymph node biopsy, which isolated 2 lymph nodes that were negative (stage IIa). The definitive histopathology results reported a poorly differentiated neuroendocrine carcinoma measuring 45 mm with lymphovascular invasion. The definitive immunohistochemistry results were positive for chromogranin, synaptophysin, mammaglobin and GCDFP-15 and negative for CD56, which guided the diagnosis more towards neuroendocrine carcinoma than infiltrating ductal carcinoma with neuroendocrine differentiation. The patient received adjuvant treatment with anthracyclines and taxanes and is currently disease-free after 6 months of follow-up.
Primary NET of the breast are rare neoplasms that originate in enterochromaffin cells. Fyerter and Hartmann were the first to report 2 patients with primary carcinoid tumor of the breast in 1963,3 describing them as tumors with the presence of argyrophil cells and the ability to produce hormones. Since 2003, the World Health Organization has included NET in their classification of breast tumors as a specific histological type, requiring for diagnosis that more than 50% of the cells express neuroendocrine markers, chromogranin and/or synaptophysin.4 In 2012, the World Health Organization created 3 different categories: well-differentiated NET, poorly differentiated/small-cell and invasive carcinoma with neuroendocrine differentiation. This definition includes variants in which mucinous and/or apocrine phenotypes may coexist.5 In the literature, NET of the breast are reported as incidental pathological findings after surgery, or during differentiation with another breast carcinoma, while pure neuroendocrine tumors are very rare to find and represent <1% of breast carcinomas.6 The incidence of these tumors increases with age, and they are mainly observed in postmenopausal women. Their presentation is usually as palpable tumors, although clinically and radiologically there are no specific characteristics differentiating them from invasive breast carcinomas. The secretion of vasoactive hormones by these tumors is rare, unlike other extra-mammary carcinoids.7 The diagnosis is therefore based on the histological study, presenting nests of small cells that are well circumscribed with hyperchromatic nucleus, positive argyrophil reaction and the presence of small neurosecretory granules separated by highly vascularized stroma bands and dense areas of collagen, with a papillary and microglandular pattern. The immunohistochemistry study frequently reveals the expression of positive hormone receptors and negative HER-2, as in our case. The granules are positive for neuron-specific enolase, chromogranin and/or synaptophysin.8 Currently, positive GCDFP-15 and mammaglobin are considered markers to differentiate primary NET of the breast from metastatic tumors, since the latter would not express them, and their determination is essential for the differential diagnosis.2 Vascular and lymphatic system invasion has also been described, as observed in our patient.
Regarding the treatment of these lesions, a standard treatment has not been established and most clinicians rely on their experience with invasive ductal carcinoma, based on tumor stage at the time of diagnosis. The role of specific treatments, such as platinum-based chemotherapy, somatostatin analogues, peptide receptor radionuclide therapy or temozolomide, still remains unclear.9
The prognosis of this type of tumor has also not been well defined, although recent studies show that it is similar to that of conventional infiltrating ductal carcinomas.10
Please cite this article as: Marín Hernández C, Galindo Fernández PJ, Caballero Illanes A, Guzmán F, Parrilla Paricio P. Carcinoma neuroendocrino primario de mama. Cir Esp. 2020;98:110–112.