The prevalence of duodenal diverticula in the population varies from 0.16% to 22%.1 Generally, the presentation is asymptomatic and the finding is incidental during imaging tests. When diverticula cause symptoms, these usually include hemorrhage, diverticulitis, formation of bezoars, obstruction, perforation, pancreatitis, extrinsic compression of the bile ducts or cholangitis.2,3
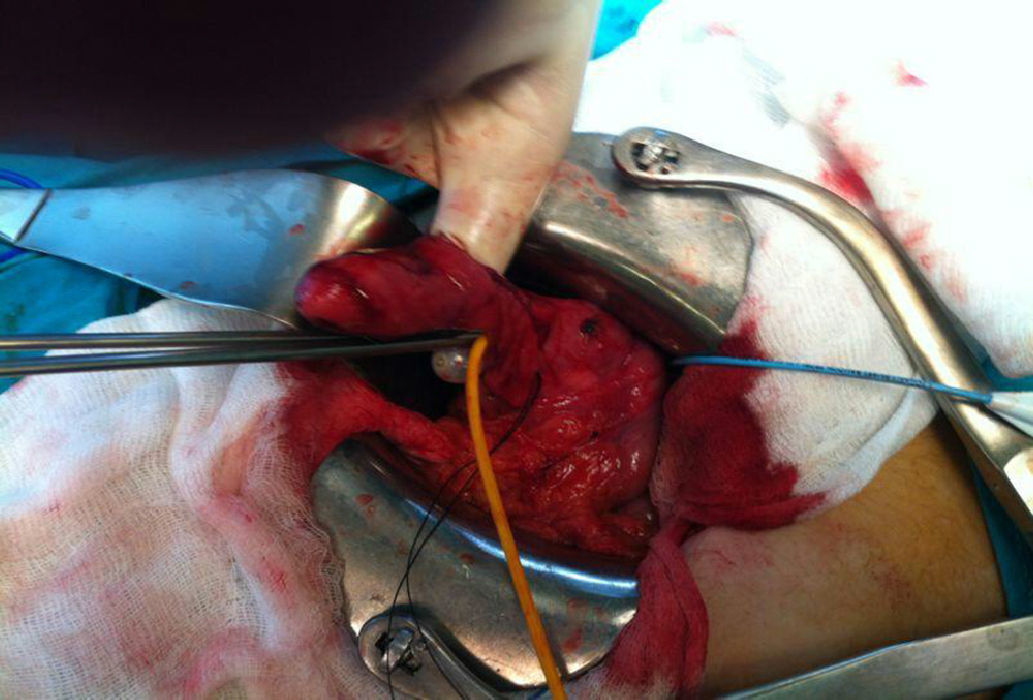
We present the case of a 16-year-old patient with no medical history of interest who came to our emergency department on successive occasions due to epigastric pain. The patient was diagnosed with acute pancreatitis and hospitalized for further studies. Abdominal ultrasound and magnetic resonance cholangiography were normal. Gastrointestinal transit test showed evidence of an intraluminal duodenal diverticulum that occupied the lumen from the knee of the duodenum up until the third portion. Gastroscopy confirmed the existence of the diverticulum situated close to the major papilla. The patient was scheduled for surgery, which included duodenotomy, diverticulectomy, and hemostatic suture. Postoperative evolution was favorable, and the patient was discharged from the hospital on the eighth day after the procedure.
DiscussionDuodenal diverticula are congenital in young patients and acquired in adults. The congenital types are usually true diverticula and contain all the layers of the duodenal wall, while the acquired ones are usually false (herniations of the duodenal mucous membrane through the muscular layer). They can present in the second, third or fourth portion of the duodenum, with a preference for the second.4 Only 10% cause symptoms.5 In our case, possibly the accumulation of intestinal material in the diverticulum was the cause of the compression of the pancreatic duct or the bile duct, causing recurrent pancreatitis.6 Another cause is the colonization of the diverticulum by bacteria that produce beta-glucuronidases, favoring the formation of calcium bilirubinate. The therapeutic possibilities in cases of duodenal diverticula that cause pancreatitis symptoms are endoscopic resection, diverticulectomy by laparotomy or laparoscopy7 or biliary enteric bypass by means of Roux-en-Y hepaticojejunostomy.8 The possibility of an intraluminal duodenal diverticulum should be considered in the differential diagnosis in cases of pancreatitis with unknown etiology or in very young patients (Figs. 1 and 2).
Conflict of InterestsThe authors declare that there is no conflict of interest.
Please cite this article as: Saeta Campo R, Coves Alcocer R, Navío Perales J, Maturana Ibáñez V, Meroño Carbajosa E. Pancreatitis de repetición en paciente de 16 años. Cir Esp. 2014;92:564–565.