To present our experience of patients with Hirschsprung disease (HD) operated by transanal endorrectal descent (TED).
MethodsA retrospective study performed of TEDs. We correlate fundamentally the aganglionic segment length with: complications, need for colostomy and surgical approach.
ResultsBetween 2003 and 2012 we performed 73 TED (57 men), 78.6% diagnosed in the neonatal period. The aganglionic segment length evidenced in the enema was correlated with surgical findings in 68.9% of cases, being higher in the short forms than in the long segments (80.9 vs 44%, P<.001). Four patients required preoperative colostomy. The mean age of surgery was 6.3 months (4.5–33.7). Short forms represented 64.4% of cases. The abdominal approach was necessary in 10 patients, nine of these were long/total colonic aganglionic segment. Postoperative enterocolitis presented in 10.9% (nine patients), with no relation with the length of aganglionic or the existence of residual dysplasia. Obstructions occurred in 19.2% of the long form or pancolonic forms. Currently, of the evaluable patients, five present constipation and 12 present occasional leakage.
ConclusionsTED is the surgery of choice for patients with HD. The majority can be handled by preoperative “nursing” without colostomy. The diagnostic tests of choice are manometry with suction biopsy. No significant correlation was found between enterocolitis and length of aganglionic segment, although we observed a drastic reduction of postoperative enterocolitis, since the introduction of technical changes, such as the use of postoperative rectal tubes and the posterior section of the cuff muscles.
Presentar nuestra experiencia en el tratamiento de pacientes con enfermedad de Hirschsprung (EH) intervenidos mediante descenso endorrectal transanal (DET).
MétodosEstudio retrospectivo de los DET realizados. Correlacionamos, fundamentalmente, longitud del segmento agangliónico, con complicaciones, necesidad de colostomía y vía de abordaje.
ResultadosEntre 2003 y 2012 hemos realizado 73 DET (57 varones), 78,6% diagnosticados en el periodo neonatal. La longitud agangliónica objetivada en el enema se correspondió con los hallazgos quirúrgicos en un 68,9% de los casos; esta correspondencia fue mayor en las formas cortas que en las largas o pancolónicas (80,9 vs. 44%; p<0,001). Cuatro pacientes precisaron colostomía preoperatoria. La edad media al descenso fue de 6,3 meses (rango 4,5-33,7). El 64,4% eran formas cortas. El abordaje abdominal fue necesario en 10 pacientes (13,6%), 9 de ellos aganglionismos largos o pancolónicos. El 10,9% (8 pacientes) ha presentado enterocolitis postoperatoria, sin relación con la longitud agangliónica ni con la existencia de displasia residual. La suboclusión por bridas se presentó en el 19,2% de las formas largas o pancolónicas. Actualmente, de los pacientes valorables, 5 tienen hábito estreñido y 12 presentan escapes ocasionales.
ConclusionesEl DET es la cirugía de elección para pacientes con EH. La mayoría pueden manejarse con «nursing» preoperatorio, sin colostomía. Las pruebas diagnósticas de elección son la manometría y la biopsia rectal por succión. No hemos encontrado correlación entre la existencia de enterocolitis y la longitud del segmento agangliónico, aunque hemos observado una reducción drástica de las enterocolitis postoperatorias, desde la introducción de modificaciones técnicas, como la sonda rectal posquirúrgica y la sección posterior del manguito muscular.
Surgery has progressed notably over the last two decades in the treatment of Hirschprung's disease (HD). It now consists of a single operation instead of several-stage surgery, and is performed in the first months of life without the need for pre-surgical colostomy in the majority of cases.1 The treatment of HD traditionally involved the need for several surgical operations, with their corresponding general anaesthesia and hospital admission during more than the first year of life. Colostomy used to be performed at the moment of diagnosis, followed in a second operation by resection of the aganglionic segment and pull-through of the intestine with normal nerves, and then closure of the colostomy in a third operation.
In 1964 Soave described endorrectal mucosectomy.2 In the same year Boley described a widely accepted modification, consisting of performing anastomosis during the same operation, through the abdomen. These techniques have been used without any major change for the last 30 years.3 In 1980, So et al. described endorectal pull-through in 20 newborn babies without prior colostomy.4 In 1995 Georgeson et al.5 described transanal mucosectomy assisted by abdominal laparoscopy. In 1998, de la Torre-Mondragón and Ortega-Salgado6 described totally transanal mucosectomy, colectomy and pull-through in the treatment of rectosigmoid HD in a single surgical operation.
This work has the aim of evaluating the results of our experience in HD patients operated on using transanal endorectal pull-through (TEP). The improvements arising from technical modifications introduced during our experience are also analysed.
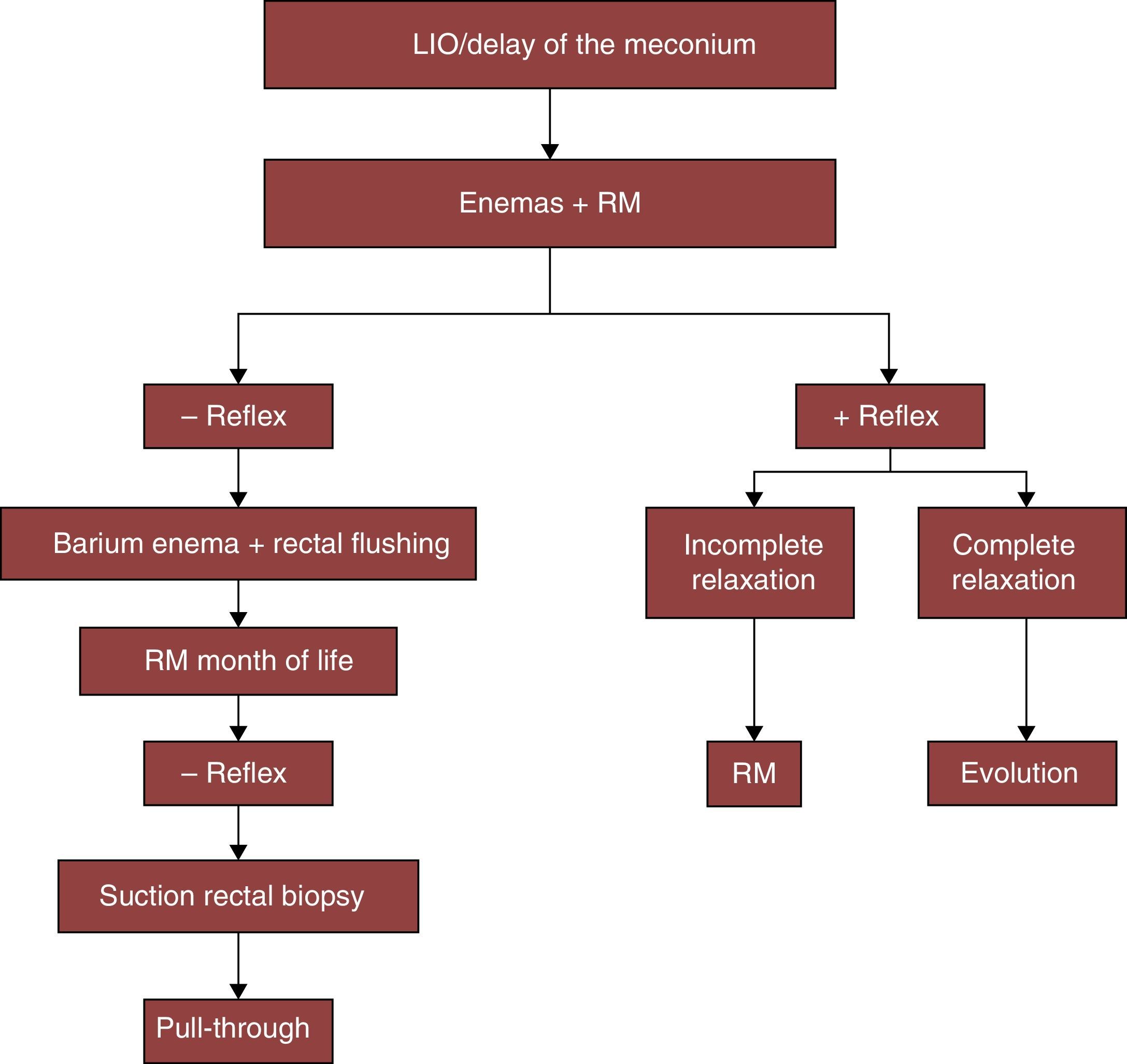
MethodsWe undertook a retrospective study of patients diagnosed HD and operated using TEP in our hospital, by revising hospital clinical histories. Given the clinical suspicion of HD, we apply an established protocol for diagnosis and treatment, as shown in the algorithm of Fig. 1. The absence of anal sphincter inhibitory reflex in anorectal manometry and suction rectal biopsy is considered to be definitive diagnostic tests. Pre-operative preparation consists of rectal flushing.
The following variables were analysed:
- •
Family and personal history.
- •
Form of clinical presentation (delayed evacuation of the meconium, constipation, abdominal swelling, vomiting or lower intestinal obstruction).
- •
Age at diagnosis (neonatal, or after the first month of life).
- •
Additional diagnostic tests (simple X-ray of the abdomen, contrast enema, anorectal manometries and suction rectal biopsy).
- •
Pre-operative complications and the need for colostomy.
- •
Age and weight at TEP, technical modifications used and hospitalisation.
- •
Post-operative complications.
- •
Aganglionic length and the existence of residual dysplasia.
- •
The current state of the patient (continence, incomplete pull-through).
The relationship between the length of the aganglionic segment and the existence of residual dysplasia and the need for pre-operative colostomy found in the histopathological study were studied, together with the existence of pre- and postoperative enterocolitis and the capacity to remain continent in assessable patients (over 4 years old and with normal neurological development).
Statistical AnalysisA descriptive study of the data was performed, showing qualitative variables by frequencies and percentages; the average and range (minimum–maximum) of quantitative variables are shown.
To analyse the association of radiologically aganglionic segment length groups with the other qualitative variable–Pearson's chi-squared test or Fischer's exact test–were used.
The level of significance was considered to stand at P<.05. Data were analysed using SPSS 19.0.
ResultsA total of 73 TEP were performed from 2003 to 2012 (16 females and 57 males). Diagnosis took place during the neonatal period in 78.6% of cases, at an average age of 8.6 days (range: 2–24 days).
The average time of gestation was 38.8 weeks (range: 34–42 weeks), with an average weight at birth of 3151g (range: 1986–4595g). Three patients had a family history of HD.
With respect to the initial clinical symptoms, delay in evacuation of the meconium was reported in 65.5% of cases, accompanied by abdominal swelling in 53.4% and vomiting in 23.3% of the newborn babies. About 28.8% presented symptoms of lower intestinal obstruction at birth. Only four patients (5.5%) were diagnosed following the development of enterocolitis symptoms.
The results of simple abdominal X-ray showed swelling of the intestinal loops in 53.4% of cases, while 28.8% presented lack of distal air and 1.4% presented fecaloma.
Associated malformations were present in 24 patients (32.9%): six cases were associated with congenital cardiopathies, three with neurological alterations, five with IgA deficit and celiac disease, while six patients were carriers of trisomy 21.
Contrast enema showing the transition zone was taken as proof of HD in 75% of cases. The length of the radiologically aganglionic segment agreed with surgical findings in 68.9% (50) cases. This correlation was significantly higher in short Hirschsprung segments than it was in long or pancolonic ones (80.9 vs 44%; P<.001).
The anorectal manometry that showed the absence of reflex anal inhibition took place at an average age of 48 days (range: 17–134 days). Suction rectal biopsy for subsequent definitive diagnosis took place at an average age of 67 days (range: 45.5–167 days).
Pre-operative colostomy was necessary in four patients: two due to the impossibility of home nursing and one due to intestinal obstruction. The other colostomy was performed in another hospital. The other patients were treated by home nursing without the need for a colostomy prior to TEP surgery.
The average age at TEP of patients diagnosed neonatally was 4.5 months (range: 2.9–6.3 months). Average weight at the TEP operation was 6525g (range: 5600–7500g).
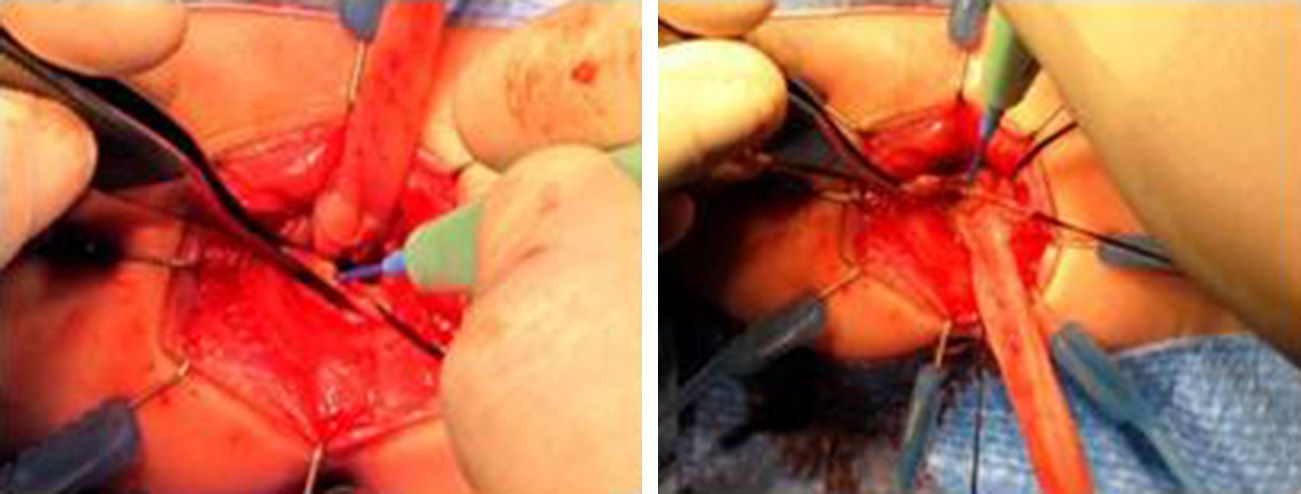
We have made two changes to the technique described by de la Torre. The first is the use of a postoperative rectal drain (Fig. 2). The second change is the subsequent resection of the residual seromuscular layers (Fig. 3), as described by other authors.7
A total of 73 TEP were performed:
- •
Without subsequent myotomy and with no rectal catheter in the first 34 patients.
- •
Without subsequent myotomy and with a rectal catheter in the following four patients.
- •
With myotomy and with a rectal catheter in the last 39 patients.
The abdominal approach using laparotomy was necessary in 10 patients (13.6%), nine of whom presented long or pancolonic aganglionism. In eight of these cases pull-through was carried out with ileoanal anastomosis and protective ileostomy in the same TEP operation.
The definitive histopathological study found that in 64.4% (47) cases the length of the aganglionic zone corresponded to short or rectosigmoid segments, while 27.4% (20) cases were long segments and 8.2% (six) cases presented pancolonic involvement. In 33.3% of cases intestinal dysplasia was detected in the intestinal segment pulled through, with giant submucosal ganglia.
Three patients presented immediate postoperative complications. One needed colostomy due to perforation of the rear face of the pulled-through colon, probably due to ischaemia. In the two remaining patients iatrogenic dehiscence of the anastomosis occurred when inserting the rectal catheter, due to the development of abdominal swelling.
Respecting late complications following TEP, eight patients (10.9%) developed enterocolitis, without any statistically significant relationship with aganglionic length or the existence of residual dysplasia. Sub-obstruction due to adhesions occurred in 8.2% of the total number of patients, and it presented in up to 19.2% of the long or pancolonic forms. Stenosis of the pulled-through intestine anastomosis occurred in four (5.5%) patients, making Hegar dilation necessary for a longer period. Incomplete pull-through was detected in follow-up using rectal manometry and biopsy in two patients.
All patients were examined 2 weeks after the operation in out-patient visits to our hospital. The anus was gently calibrated and dilated every week for the first three months after the operation, until the correct calibre for the age of the child was attained.
With regards to continence, of the patients who can be assessed in visits (over 4 years old, with normal neurological psychomotor development), 5 tend to be constipated and 12 present occasional incontinence.
DiscussionThe aim of TEP in HD is to resect the aganglionic intestinal segment and pull-through intestine with correct enteric nerves transrectally, performing an anal anastomosis with minimum damage to the muscular sphincters.
Since de la Torre Mondragón and Ortega Salgado6 described TEP in 1998, several papers have been published which show that this approach is a safe and not very invasive surgical technique. The advantages that have been described for single operation TEP are: reduction of the postoperative ileus, an early start to enteral feeding, an earlier recovery and hospital discharge as well as reduced hospital costs. It also achieves a reduction in the risks associated with intra-abdominal pelvic dissection, such as reduced bleeding, less damage to other pelvic organs, fewer adherences, less postoperative pain and better cosmetic results.8,9
If the contrast enema shows the transition zone to be rectosigmoid, it is highly probable that it will be possible to perform the procedure only using a transanal endorectal approach10; if it is higher, the patient will have to be prepared for colon mobilisation using laparotomy or laparoscopy.11
The postoperative correlation between aganglionic length and the results of the opaque enema amounted to 68.9% in our study. This is very similar to the results of other studies reported in the literature.10
In our series, 10 patients required concomitant laparotomy for additional mobilisation of the colon. In pancolonic forms we systematically practiced ileostomy simultaneously with the TEP. The aim of this is to achieve adaptation of the ileum and more consistent production of faeces, making the closure properly to prevent perianal irritation and poor intestinal absorption.
One of our technical modifications to TEP is the insertion of a rectal catheter in the theatre after surgery. This catheter prevents external anal sphincter spasm and oedema after surgery, reducing secondary abdominal swelling due to the postoperative ileus. Moreover, it renders immediate postoperative rectal catheterisation unnecessary, as this may be traumatic for the anastomosis.
As surgical techniques improved, in our series the duration of hospitalisation has been reduced to the current time of 5 days.
With regard to the pulled-through zone, histopathological study reveals that there may be residual intestinal neuronal dysplasia, as occurred in 33% of our patients. But contrary to what could be expected, we found no greater risk of postoperative complications in patients with residual intestinal dysplasia. Nor were more postoperative complications found in those cases with a long aganglionic segment.
The reported frequency of postoperative enterocolitis in the literature varies from 12% to 33%. Results published by other authors are more surprising. In 84 patients So et al. found no postoperative enterocolitis, attributing their results in part to suitable and early anal dilations to prevent anal stenosis.12,13 Possible risk factors for enterocolitis have been reported: a very long muscular sleeve, inadequate freeing of the internal anal sphincter achalasia, dehiscence of the coloanal anastomosis, coloanal anastomosis stenosis,7 the funnel effect of the rectal seromuscular sleeve14 and intrinsic alterations in the humoral immunity and microflora of the intestinal mucosa.15
In our experience, subsequent resection of the seromuscular sleeve prevents the funnel effect of the same on the pulled-through intestine. Moreover, the postoperative rectal catheter prevents spasm and oedema of the EAS, thereby preventing paralytic ileus and abdominal swelling. All of these factors favour early enteral tolerance and hospital discharge. These two technical modifications have also led to a drastic reduction in enterocolitis in our series.
To conclude, we have introduced technical improvements into the treatment of HD using TEP. The first of these was the use of a rectal catheter, inserted in the operating theatre at the end of coloanal anastomosis. The second modification was to perform a subsequent myotomy of the seromuscular sleeve, as well as the traditional previous myotomy. The rectal catheter prevents abdominal swelling caused by the postoperative paralytic ileus which sometimes occurs. Subsequent myotomy prevents the development of postoperative enterocolitis, which may be associated with complications that may even be mortal without early diagnosis and treatment.
Please cite this article as: Martínez-Criado Y, Cabrera R, Moya MJ, Valladares JC, López-Alonso M, De Agustín Asensio JC. Descenso endorrectal transanal en la enfermedad de Hirschsprun: evolución y resultados. Cir Esp. 2015;93:561–566.